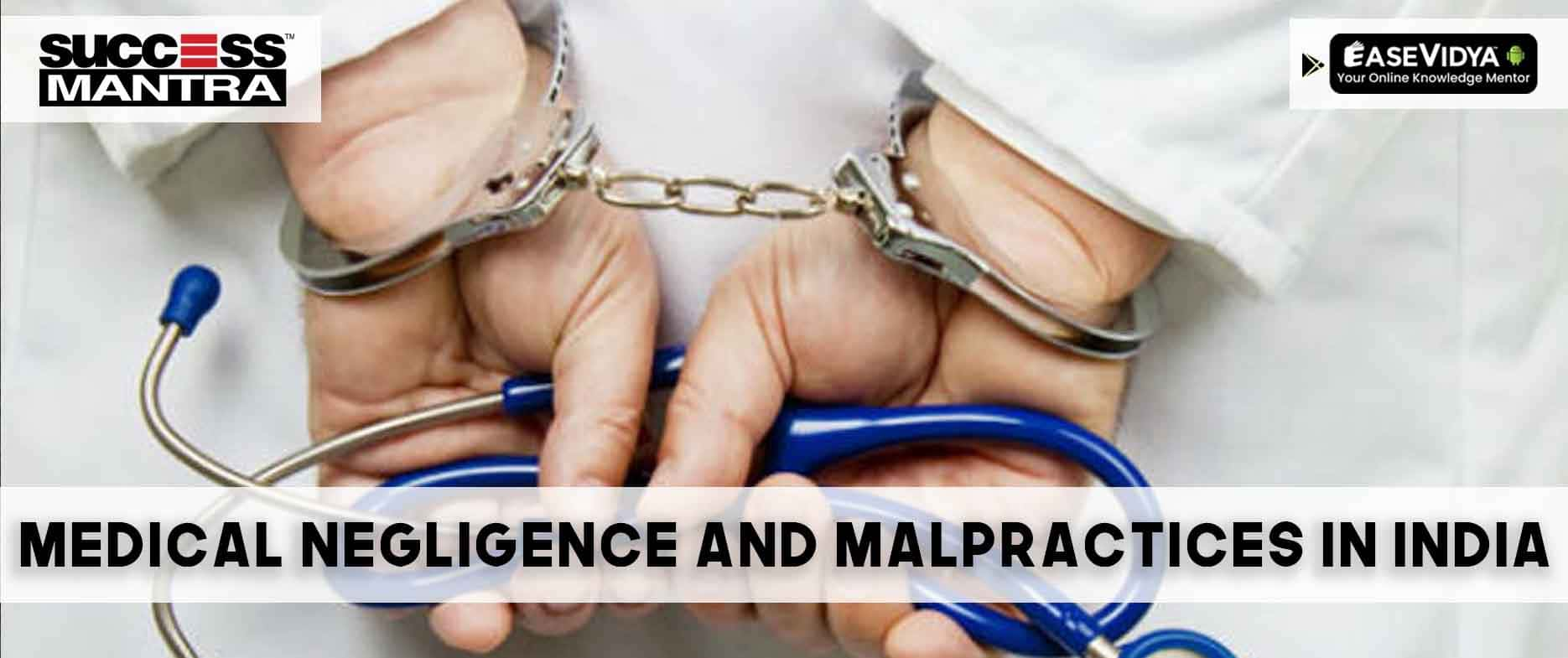
Navigating Medical Negligence and Malpractice in India: A Comprehensive Analysis with Landmark Case Laws
Navigating Medical Negligence and Malpractice in India: A Comprehensive Analysis with Landmark Case Laws
Introduction:
Medical negligence and malpractice are pressing concerns in India, where the healthcare system plays a vital role in the lives of millions. The legal intricacies surrounding these issues have significant implications for both patients and healthcare professionals. This article explores the landscape of medical negligence and malpractice in India, delving into key elements, challenges, and landmark case laws that have shaped the jurisprudence.
Understanding Medical Negligence and Malpractice in India:
-
Defining Medical Negligence:
- In India, medical negligence refers to a breach of duty by a healthcare professional resulting in harm to the patient.
- The legal framework draws from established principles of negligence, duty of care, and proximate cause.
-
Medical Negligence vs. Professional Misconduct:
- While medical negligence involves the failure to meet the standard of care, professional misconduct encompasses unethical or unprofessional behavior by a healthcare practitioner.
- Both can lead to legal consequences, and the distinction is crucial for a nuanced understanding of legal proceedings.
Key Elements of Medical Negligence Cases:
-
Duty of Care:
- The doctor-patient relationship establishes a duty of care.
- The Supreme Court of India has consistently recognized this duty, emphasizing the importance of ethical and professional conduct.
-
Breach of Duty:
- The standard of care expected is that of a reasonably competent medical professional.
- The Bolam Test, derived from the UK case Bolam v. Friern Hospital Management Committee, is often applied to determine whether the professional's actions align with accepted medical practices.
-
Causation:
- Proving a direct link between the breach of duty and the harm suffered is essential.
- Indian courts consider the "but for" test – i.e., the harm would not have occurred but for the negligence.
-
Damages:
- Compensation is awarded for physical, emotional, or financial harm suffered by the patient.
- The quantum of damages depends on the severity of the harm and its impact on the patient's life.
Landmark Case Laws in India:
-
Indian Medical Association v. V.P. Shantha (1996):
- This case addressed the issue of medical negligence in the context of the doctor-patient relationship. The court emphasized the need for doctors to obtain informed consent and recognized the patient's right to know the risks associated with a procedure.
-
A.S. Mittal v. State of U.P. (1989):
- This case highlighted the importance of expert evidence in establishing medical negligence. The court stressed the significance of expert testimony to prove a deviation from the standard of care.
-
Jacob Mathew v. State of Punjab (2005):
- The Supreme Court of India in this case outlined the importance of a careful and cautious approach in deciding medical negligence cases. It emphasized that a doctor should not be judged solely by the result of the treatment but by the standard of care exercised.
-
Martin F. D'Souza v. Mohd. Ishfaq (2009):
- This case reinforced the duty of care owed by doctors and clarified that a patient's consent should not be taken for granted. The court highlighted the need for doctors to explain the risks involved in a procedure and obtain informed consent.
-
Kusum Sharma & Ors. v. Batra Hospital & Medical Research Centre & Anr. (2010):
- The Supreme Court, in this case, underscored the importance of informed consent and reiterated that patients have the right to be informed about the risks associated with medical procedures.
Challenges in Proving Medical Negligence in India:
-
Lack of Standardization:
- India's diverse healthcare landscape lacks standardized practices, making it challenging to establish a universal standard of care.
-
Expert Testimony Issues:
- Dependence on expert testimony can lead to challenges, especially when experts may have conflicting opinions or when there is a shortage of qualified medical experts.
-
Inadequate Record-Keeping:
- Incomplete or inadequate medical records can hinder the process of establishing a clear link between the doctor's actions and the patient's harm.
Recent Developments and Future Trends:
-
Telemedicine and E-Health:
- The rise of telemedicine introduces new challenges in determining the standard of care, as the traditional doctor-patient interaction evolves.
-
Patient Rights and Awareness:
- Increasing awareness about patient rights, including the right to information and informed consent, may lead to more assertive patients and a higher standard of care.
-
Legal Reforms:
- Ongoing efforts to streamline medical negligence cases and introduce reforms to the legal process aim to expedite justice and ensure fair outcomes.
Conclusion:
Medical negligence and malpractice cases in India demand a comprehensive understanding of legal principles, landmark case laws, and the evolving healthcare landscape. As the nation strives to provide quality healthcare to its citizens, the legal system plays a pivotal role in holding healthcare professionals accountable while balancing the need for a robust and reliable healthcare system. Landmark cases and legal developments continue to shape the narrative, emphasizing the importance of ethical conduct, informed consent, and a patient-centric approach in the practice of medicine.








MauriceKesty
<a href=https://megamoriarti.com/>мега дарк нет</a> - mega darknet market mega dm, мега даркнет маркет ссылка на сайт тор
jznom
<a href=https://yourdesires.ru/useful-advice/1304-kak-vybrat-distillyator-dlya-vody.html>Как выбрать дистиллятор для воды?</a> или <a href=https://yourdesires.ru/beauty-and-health/lifestyle/508-chto-takoe-gerbalayf.html>Что такое Гербалайф?</a> <a href=http://yourdesires.ru/it/1248-kak-vvesti-znak-evro-s-klaviatury.html>клавиша евро на клавиатуре</a> https://yourdesires.ru/beauty-and-health/diets/23-dieta-protasova.html
Michaelpneup
<a href=https://krakenmp.xyz>кракен онион</a> - зеркало кракен даркнет, как зайти на кракен даркнет
WilburNouct
<a href=https://krakenmp.net>kraken shop</a> - кракен зеркало, кракен даркнет маркетплейс
MIRbib
Приветствуем на PrivetMir.net - Ваш Путь к Эксклюзивным Сделкам и Привилегиям! Скачать файл privetmir.sql.gz Мы создаем возможности для вас экономить и наслаждаться жизнью в полной мере. https://privetmir.com/
Stevenser
try this https://ja.onlinevideoconverter.pro/57DD/download-video-twitter
btaletsmwd
essay format mla https://essaybuyes.com/ - lesson plan on writing an essay narrative essays topics <a href=https://essaybuyes.com/>what is essay</a> example of narrative essays
gzsnom
<a href=https://evagro.ru>минитракторы купить в россии цена</a> или <a href=https://evagro.ru>купить минитрактор т15</a> https://evagro.ru/product/mineralnye-udobreniya-aktiv-rost-komnatnye-tsvety/ аренда погрузчиков час <a href=https://evagro.ru>аренда экскаватора погрузчика в казани</a>
mtaletaaly
mla essay example https://essaybuyes.com/ - sample essay with apa formatting reference for essay <a href=https://essaybuyes.com/>essays for scholarship</a> example of process analysis essay
Stephentut
visit our website https://it.onlinevideoconverter.pro/190Fp/
onlspfbhok
Navigating Medical Negligence and Malpractice in India: A Comprehensive Analysis with Landmark Case Laws onlspfbhok http://www.gi01pfd2bx667g65i53x1sly964yl8x2s.org/ <a href="http://www.gi01pfd2bx667g65i53x1sly964yl8x2s.org/">aonlspfbhok</a> [url=http://www.gi01pfd2bx667g65i53x1sly964yl8x2s.org/]uonlspfbhok[/url]
decjxhspl
Navigating Medical Negligence and Malpractice in India: A Comprehensive Analysis with Landmark Case Laws decjxhspl http://www.g604x9j48n76e5zk7k0q9h5m79phag8ss.org/ [url=http://www.g604x9j48n76e5zk7k0q9h5m79phag8ss.org/]udecjxhspl[/url] <a href="http://www.g604x9j48n76e5zk7k0q9h5m79phag8ss.org/">adecjxhspl</a>
jgtgozgsni
Navigating Medical Negligence and Malpractice in India: A Comprehensive Analysis with Landmark Case Laws jgtgozgsni http://www.g0wwq4nw2ar0t8rh4w9v6c1g484j5099s.org/ <a href="http://www.g0wwq4nw2ar0t8rh4w9v6c1g484j5099s.org/">ajgtgozgsni</a> [url=http://www.g0wwq4nw2ar0t8rh4w9v6c1g484j5099s.org/]ujgtgozgsni[/url]
Waldo
We would like to thank you once again for the lovely ideas you offered Jeremy when preparing her own post-graduate research and also, most importantly, for providing all the ideas in one blog post. Provided we had known of your site a year ago, i'd have been rescued from the needless measures we were employing. Thank you very much. toys for adults
ykfivjjzg
Navigating Medical Negligence and Malpractice in India: A Comprehensive Analysis with Landmark Case Laws <a href="http://www.g10v48a4d2u49625kiqwm8xs7qi5nh56s.org/">aykfivjjzg</a> [url=http://www.g10v48a4d2u49625kiqwm8xs7qi5nh56s.org/]uykfivjjzg[/url] ykfivjjzg http://www.g10v48a4d2u49625kiqwm8xs7qi5nh56s.org/
jbxtgeczm
Navigating Medical Negligence and Malpractice in India: A Comprehensive Analysis with Landmark Case Laws jbxtgeczm http://www.ghoj93vnsd1vg6403j3245dr0t4616kjs.org/ <a href="http://www.ghoj93vnsd1vg6403j3245dr0t4616kjs.org/">ajbxtgeczm</a> [url=http://www.ghoj93vnsd1vg6403j3245dr0t4616kjs.org/]ujbxtgeczm[/url]
Christoper
Wow, marvelous blog format! How long have you ever been running a blog for? you make blogging look easy. The overall look of your web site is wonderful, let alone the content material! You can see similar: Funero.shop and here Funero.shop
yrfosjfszf
Navigating Medical Negligence and Malpractice in India: A Comprehensive Analysis with Landmark Case Laws yrfosjfszf http://www.g7azekc6dzsf094i20j44l36123v0cp6s.org/ [url=http://www.g7azekc6dzsf094i20j44l36123v0cp6s.org/]uyrfosjfszf[/url] <a href="http://www.g7azekc6dzsf094i20j44l36123v0cp6s.org/">ayrfosjfszf</a>
mmfededtih
Navigating Medical Negligence and Malpractice in India: A Comprehensive Analysis with Landmark Case Laws <a href="http://www.g5vle428650nrp1f0so6r3as3p2u0h88s.org/">ammfededtih</a> mmfededtih http://www.g5vle428650nrp1f0so6r3as3p2u0h88s.org/ [url=http://www.g5vle428650nrp1f0so6r3as3p2u0h88s.org/]ummfededtih[/url]
zmzqgjqqx
Navigating Medical Negligence and Malpractice in India: A Comprehensive Analysis with Landmark Case Laws <a href="http://www.gf0m2v483801r66q32jl07bqgn11turcs.org/">azmzqgjqqx</a> zmzqgjqqx http://www.gf0m2v483801r66q32jl07bqgn11turcs.org/ [url=http://www.gf0m2v483801r66q32jl07bqgn11turcs.org/]uzmzqgjqqx[/url]
wtqlmnwpg
Navigating Medical Negligence and Malpractice in India: A Comprehensive Analysis with Landmark Case Laws [url=http://www.g5o0d6k58f2gnx0bgvs3340rp2r311z6s.org/]uwtqlmnwpg[/url] <a href="http://www.g5o0d6k58f2gnx0bgvs3340rp2r311z6s.org/">awtqlmnwpg</a> wtqlmnwpg http://www.g5o0d6k58f2gnx0bgvs3340rp2r311z6s.org/
srbedty
Navigating Medical Negligence and Malpractice in India: A Comprehensive Analysis with Landmark Case Laws <a href="http://www.gw3k9088m5g1fqok453cj5i08ne23y8js.org/">asrbedty</a> srbedty http://www.gw3k9088m5g1fqok453cj5i08ne23y8js.org/ [url=http://www.gw3k9088m5g1fqok453cj5i08ne23y8js.org/]usrbedty[/url]
lvffhtfqo
Navigating Medical Negligence and Malpractice in India: A Comprehensive Analysis with Landmark Case Laws lvffhtfqo http://www.g4zm813195e3qs2oinytt7a0545jkv68s.org/ [url=http://www.g4zm813195e3qs2oinytt7a0545jkv68s.org/]ulvffhtfqo[/url] <a href="http://www.g4zm813195e3qs2oinytt7a0545jkv68s.org/">alvffhtfqo</a>
tjscvoxpg
Navigating Medical Negligence and Malpractice in India: A Comprehensive Analysis with Landmark Case Laws [url=http://www.gr97otmgo1h264937m2501qww6oj68qis.org/]utjscvoxpg[/url] tjscvoxpg http://www.gr97otmgo1h264937m2501qww6oj68qis.org/ <a href="http://www.gr97otmgo1h264937m2501qww6oj68qis.org/">atjscvoxpg</a>
qmewllwp
Navigating Medical Negligence and Malpractice in India: A Comprehensive Analysis with Landmark Case Laws qmewllwp http://www.g09m0dxww3748c60ljdh1f066b66f8kzs.org/ <a href="http://www.g09m0dxww3748c60ljdh1f066b66f8kzs.org/">aqmewllwp</a> [url=http://www.g09m0dxww3748c60ljdh1f066b66f8kzs.org/]uqmewllwp[/url]
Donna
Если вам нужно купить что-то, то посещение официального маркета Kraken будет правильным решением. У нас вы найдете все, что вам нужно, и сможете совершать покупки с полной уверенностью в безопасности и анонимности. Присоединяйтесь к нашей платформе уже сейчас и наслаждайтесь широким выбором товаров. Официальный магазин Кракен доступен по адресу:Kraken Darknet -> http://www.articlesgiant.com/Best-Sites-Do-You-Really-Want-It-This-May-Help-You-Determine.htm. Для его посещения не требуется подключение к Тор или VPN. Просто кликните на наш сайт и окунитесь в огромный магазин с безграничными возможностями. Не упускайте время и исследуйте новый мир, который ждет вас на Кракене.
Cecelia
Кракен - авторитетный ресурс торговой анонимной площадки, который является самым крупным в России. Если вы ищете площадку, где можно приобрести любые товары, то Kraken - отличный выбор. Здесь каждый пользователь сможет найти подходящий товар или отдельную категорию товаров. Сама площадка полностью конфиденциальна и безопасна. Здесь вы можете совершать покупки, не беспокоясь о потере денег или личных данных. Кроме того, Кракен onion является не частным магазином, а своеобразным маркетплейсом. Тут ссылка на кракен выложены товары тысяч продавцов и магазинов, и всегда можно найти выгодное предложение для себя. При выборе товаров и услуг рекомендуется рассматривать разные предложения, так как на площадке представлены карточки от разных торговцев. Наши актуальные зеркала Кракен кракен маркетплейс -> https://burtonvarela4.discussblog.com/eight-ways-best-sites-will-help-you-get-more-business/ откроют доступ к сайту в течение нескольких секунд. 2krn.
Carin
Хотите найти торговую площадку, где можно приобрести разнообразные продукты? Рекомендую рассмотреть официальный сайт Кракен: площадка кракен -> http://www.bonniesdelights.com/index.php?a=stats&u=brittanybarlow7. Здесь каждый покупатель сможет найти подходящий товар или отдельную категорию. Площадка полностью скрыта и гарантирует конфиденциальность. Покупки можно совершать, не беспокоясь о потере денег или личных данных. Кроме того, Кракен onion представляет собой не только частный магазин, а уникальный маркетплейс. Здесь Krn выставляют свои вещи тысячи торговцев, и всегда можно обнаружить что-то максимально выгодное. Рекомендую пройти быструю регистрацию на платформе Кракен onion и перейти в магазин, где вы легко найдете нужные товары. При возникновении трудностей, администрация сайта всегда готова предоставить ассистенцию.
Monique
Kraken - авторизованный онлайн ресурс крупнейшей площадки торговли в России. Здесь кракен зеркало вы обнаружите разнообразные продукты, соответствующие любым вашим запросам. Пройдите быструю регистрацию, и вам откроется доступ ко всем функциям площадки. Стоит отметить, что Kraken onion работает без использования тора. Вам просто нужно перейти по ссылке и выполнить авторизацию. При выборе товаров или услуг рекомендуем рассмотреть различные варианты. На площадке представлено множество предложений от разных торговцев, так что, потратив чуть больше времени на поиск, вы обнаружите более выгодные предложения. Не стоит заканчивать поиск первым попавшимся продуктом. Исследуйте более внимательно, и у вас обязательно будет успех. У нас также есть актуальные зеркала кракен Кракен kraken ссылка -> http://signals.pro/best-sites-report-statistics-and-info/, которые обеспечат моментальный доступ к желаемому ресурсу.
Gertie
Кракен - официальный портал гигантской рынка торговли в Содружестве Независимых Государств. Здесь кракен онион вы найдете разнообразные товары, полностью соответствующие вашим требованиям. Пройдите быструю регистрацию, и вам откроется доступ ко всем функциям платформы. Стоит отметить, что Kraken onion работает без использования сети Tor. Просто перейдите по ссылке на веб-сайт и выполните авторизацию. Рекомендуем рассмотреть различные варианты при выборе товаров или услуг. На площадке представлены многочисленные предложения от разных производителей. Не стоит заканчивать поиск первым же товаром. Проведите более тщательный поиск, и вы обязательно найдете выгодные предложения. У нас также есть актуальные зеркала кракен Кракен 2krn.at -> https://alwaysbeenme.com/extra-on-making-a-residing-off-of-best-sites/, которые обеспечат мгновенный доступ к ресурсу. Ссылка на Kraken onion также доступна.
Elena
Кракен - главный онлайн ресурс громадного торгового маркетплейса в Содружестве Независимых Государств. Здесь kraken тор вы найдете различные продукты, соответствующие всем вашим запросам. Пройдите быструю регистрацию, и вам откроется доступ ко всем функциям платформы. Важно отметить, что Кракен onion работает без использования сети Tor. Вам просто нужно перейти по ссылке на веб-сайт и выполнить авторизацию. При выборе продуктов или услуг рекомендуем рассмотреть различные варианты. На площадке представлено множество предложений от разных производителей, так что, потратив немного больше времени на поиск, вы найдете более выгодные предложения. Не стоит заканчивать поиск первым же товаром. Исследуйте внимательнее, и у вас обязательно будет успех. У нас также есть актуальные зеркала сайта Кракен vk1 -> http://prof61.ru/index.php?option=com_phocaguestbook&id=1, которые обеспечат мгновенный доступ к желаемому ресурсу.
Jaqueline
В поиске торговую площадку, где можно приобрести любые вещи? Тогда стоит ознакомиться с официальным порталом Kraken: Krn -> http://www.drsbook.co.kr/board/12420317. Здесь каждый клиент сможет найти подходящий товар или отдельную категорию. Сама площадка полностью анонимна и обеспечивает безопасность. Здесь можно проводить покупки, не беспокоясь о потере денег или личных данных. Кроме того, Kraken onion не просто частный магазин, а уникальный маркетплейс. Тут кракен сайт предлагают свои товары тысячи торговцев, и всегда можно обнаружить что-то максимально выгодное. Поэтому советую пройти быструю регистрацию на платформе Кракен onion и перейти в магазин, где вы легко найдете нужные товары. А при возникновении проблем, администрация сайта всегда готова предоставить ассистенцию.
Lurlene
У нашей команды появилась уникальная даркнет-платформа под названием Kraken MARKET , которая может стать отличной альтернативой Hydra в подпольном интернете. Этот ресурс 2krn -> https://www.shrunken.com/krakentor35661 предоставляет возможность совершать мгновенные транзакции, гарантируя, что после оплаты клада деньги будут немедленно перечислены на счет продавца. Защита данных пользователя также имеет первостепенное значение - все личные данные шифруются и защищаются, чтобы предотвратить несанкционированный доступ как со стороны посторонних лиц, так и спецслужб.
Riley
Хотите обнаружить торговую площадку, где можно приобрести любые продукты? Тогда рекомендуем рассмотреть официальный портал Kraken: кракен онлайн -> https://swayycases.com/9-explanation-why-youre-still-an-beginner-at-best-sites/. Здесь каждый сможет отыскать подходящий товар или отдельную категорию. Сама площадка полностью анонимна и обеспечивает безопасность. Здесь можно осуществлять покупки, не беспокоясь о потере финансов или личных данных. Кроме того, Кракен onion не просто частный магазин, а своего рода маркетплейс. Здесь kraken darknet -> https://affiliates.trustgdpa.com/3-secrets-and-techniques-how-to-use-best-sites-to-create-a-successful-businessproduct/ предлагают свои товары тысячи поставщиков, и всегда можно найти что-то максимально выгодное. Поэтому рекомендуем пройти быструю регистрацию на сервисе Kraken onion и перейти в магазин, где вы легко найдете нужные товары. А при возникновении проблем, администрация сайта всегда готова предоставить поддержку.
Myron
Лучший сайт для покупки товаров разной направленности - Кракен vk4.at -> http://www.bonniesdelights.com/index.php?a=stats&u=maritadupre873. Это крупнейшая в России и СНГ торговая анонимная площадка, которая позволяет быстро и безопасно продавать и покупать товары любого типа. Для каждого пользователя представлена масса возможностей. К тому же, у каждого продавца есть рейтинг, отзывы, и другая информация, которая поможет вам подобрать подходящее предложение. — это лучший, и наверное, единственный сайт, на котором можно купить любые вещи, независимо от вашего желания и требований. При этом Администрация проекта кракен тор -> http://jit-math.6te.net/index.php?name=webboard&file=read&id=29848 гарантирует анонимность и безопасность при совершении сделок. И контролирует каждую покупку, чтобы пользователей не обманывали. Именно поэтому площадка настолько востребована и популярна.
Audrea
Одной из преимуществ Kraken является гарантия безопасности и анонимности. Вам не нужно устанавливать дополнительные инструменты, такие как браузер Тор или VPN-соединение, чтобы пользоваться площадкой. Просто перейдите на официальный веб-сайт Кракен и начните использовать его прямо сейчас. kraken (https://www.so-toulouse.com) -> https://sccardio.org/forum/profile/fayemckeown0164/ Важно помнить, что актуальность зеркала Кракен может меняться, поэтому рекомендуется следить за его обновлениями, чтобы всегда быть в курсе и пользоваться площадкой без проблем. Не откладывайте, переходите на Kraken прямо сейчас и наслаждайтесь удобством и безопасностью покупок.
Sven
Мы предоставляем только актуальные зеркала Kraken, которые позволят вам получить доступ к желаемому магазин у всего за несколько секунд. У нас вы найдете надежные и быстрые способы попасть на платформу Kraken и насладиться всеми ее возможностями. Ищете площадку, где можно приобрести любые продукты? Рекомендую обратить внимание на официальный маркетплейс Kraken. Здесь каждый найдет подходящие для себя позиции или категории. Наша площадка полностью безопасна и безопасна. kraken2trfqodidvlh4aa337cpzfrhdlfldhve5nf7njhumwr7instad.onion -> http://millennialbh.com/duscipit-duis-donec-hendrerit-lacus-risus/ Вы можете совершать покупки, не беспокоясь о потере денег или личных данных.
Kimberley
Кракен - авторитетный портал торговой анонимной площадки, которая признана крупнейшей в своем роде в России. Перейдя в Kraken магазин, вы разблокируете полный доступ к ассортименту. Здесь каждый сможет выбрать подходящий товар из разнообразного ассортимента. На данный момент на площадке можно увидеть миллионы товаров и услуг разного направления, привлекая пользователей из разных стран СНГ. При этом Kraken union не требует установки браузера TOR и соединения через него. Площадка полностью анонимна и работает автономно. Вам просто перейдите по ссылке Kraken: Krn (www.sunti-apairach.com) -> http://forum.artefakt.cz//profile.php?id=263927. Далее потребуется пройти простую регистрацию, и после этого получить доступ к уникальному каталогу магазина Kraken, где можно найти товары на любой вкус, независимо от ваших предпочтений.
Laurence
Хотите эксклюзивное место, чтобы купить всё? Рекомендуем посетить официальный сайт Кракен: https kraken12 +at -> http://nkuk21.co.uk/activity/9616350 . Здесь каждый покупатель сможет подобрать идеальный товар или услугу. Безопасные и анонимные операции - вот залог успешных сделок на Kraken onion. Просто переходите по ссылке, быстро регистрируйтесь и погружайтесь в мир кракен даркнет маркета. Это не просто магазин, это уникальное пространство, где тысячи продавцов предлагают свои товары. Откройте для себя выгодные сделки на Кракен даркнет, кракен зеркало сайта, и прочувствуйте анонимностью в каждой покупке.
Ken
Kraken - ваш билет в мир анонимной торговли в России. Здесь любой найдет, что ему нужно! Просто перейдите по уникальной ссылке кракен -> https://welnesbiolabs.com/discover-what-best-sites-is/, пройдите быструю регистрацию и наслаждайтесь широким ассортиментом. На Kraken onion вы можете быть уверены в конфиденциальности. Наш магазин - это не просто площадка, а целый мир возможностей. Товаров множество, и мы гарантируем привлекательные цены. Не упустите возможность совершить выгодные покупки. Переходите по ссылке на Kraken кракен onion -> https://edustation.co.in/essentially-the-most-and-least-effective-ideas-in-best-sites/ и начинайте свой путь к выгодным сделкам вместе с Kraken.
Bonnie
Ищете онлайн-площадку для приобретения любых товаров? Загляните на магазин Kraken с различными зеркалами и зеркалами сайта кракен . Сайт кракен тор приглашает покупателей в разнообразные категории товаров от поставщиков. Ссылка Kraken onion и k9.at предоставляют широкие возможности выбора. Регистрируйтесь на Kraken onion raken12 +at -> http://jit-math.6te.net/index.php?name=webboard&file=read&id=29828 и пробуйте преимуществами разнообразного выбора товаров!
Millie
Что такое Кракен!? Беспрепятственно развивающаяся торговая платформа подпольного интернета. Те, кто хоть раз в своей жизни был по ту сторону интернета осознают, насколько безграничен мир всемирной паутины. По сути это тот же самый интернет с которым мы знакомы, только еще лучше — здесь не действуют запреты и модерация. Здесь, kraken зеркало -> http://www.drsbook.co.kr/board/12516727 в подпольном интеренте очень много разных ресурсов плохих и хороших, качественных и нет. Каждый выбирает себе то, что ему по душе. А ты переходи в мир безгроничного постоянного блаженства - переходи на Kraken!
Addie
Что есть на Кракен? 5 000+ дилеров с разными товарами. Вы определенно найдете нужный. Обменник - возможность приобрести Биткоин на Kraken, обменяв BTC. Анонимные записки между пользователями Privnote. Нет надобности использовать Телеграм. Разрешение конфликтных ситуаций с продавцом через «диспут». И это далеко не все. На сайте даже есть отдельная страница со всеми функциями и особенностями данного ресурса kraken официальный сайт -> https://bossgirlpower.com/forums/profile.php?id=602776 .
Micki
На официальном магазине Kraken вы найдете богатый выбор позиций и услуг, удовлетворяющих любой вкус. Здесь kraken тор -> http://nightwish.southeast.cz/modules.php?name=Your_Account&op=userinfo&username=WiltonFitz можно найти все, что только возможно представить. Но самое интересное заключается в том, что проект не является обычным интернет-магазином. Он функционирует как платформа объявлений, предоставляя посреднические услуги. Это означает, что вы сможете найти множество магазинов и магазинов, сравнить цены, ознакомиться с отзывами, оценить конкуренцию и выбрать наиболее подходящий вариант.
Kimberly
обыграй 1xbet условия бонуса 1xgames
Lena
Ищете уникальную площадку, где можно конфиденциально приобрести любые вещи? Рекомендуем ознакомиться с официальным Kraken – крупнейшим маркетплейсом в России. Здесь доступны огромное количество товаров, и каждый клиент найдет подходящий вариант. Переходите по ссылке и проходите быструю регистрацию для открытия доступа. Важно, что Kraken onion работает без использования Тора. Просто перейдите и авторизуйтесь. При выборе товаров рекомендуем рассматривать разные предложения от разных торговцев. На площадке представлены карточки от различных магазинов, и внимательный поиск приведет к наилучшим предложениям. Не ограничивайтесь первым товаром – лучшие предложения всегда где-то. Также у нас есть актуальные зеркала Кракен kraken2trfqodidvlh4aa337cpzfrhdlfldhve5nf7njhumwr7instad.onion -> https://www.so-toulouse.com/spip.php?page=contact&contenu=mentions&page=contact&contenu=mentions&site=http%3A//cupak.sk/index.php&option=com_phocaguestbook&id=1&first&page=contact&contenu=mentions&site=http%3A%2F%2Fcupak.sk%2Findex.php&option=com_phocaguestbook&id=1&first=&site=https%3A%2F%2Ftobyrush.com%2Ftheorywiki%2Findex.php%3Ftitle%3DFive_Incredibly_Useful_Best_Sites_For_Small_Businesses&firstname=Cherie&message=%D0%98%D1%89%D0%B5%D1%82%D0%B5+%D0%BF%D0%BB%D0%BE%D1%89%D0%B0%D0%B4%D0%BA%D1%83%2C+%D0%B3%D0%B4%D0%B5+%D0%BC%D0%BE%D0%B6%D0%BD%D0%BE+%D0%BF%D1%80%D0%B8%D0%BE%D0%B1%D1%80%D0%B5%D1%81%D1%82%D0%B8+%D1%80%D0%B0%D0%B7%D0%BD%D0%BE%D0%BE%D0%B1%D1%80%D0%B0%D0%B7%D0%BD%D1%8B%D0%B5+%D1%82%D0%BE%D0%B2%D0%B0%D1%80%D1%8B%3F%0D%0A%D0%A1%D0%BE%D0%B2%D0%B5%D1%82%D1%83%D0%B5%D0%BC+%D1%80%D0%B0%D1%81%D1%81%D0%BC%D0%BE%D1%82%D1%80%D0%B5%D1%82%D1%8C+%D0%BE%D1%84%D0%B8%D1%86%D0%B8%D0%B0%D0%BB%D1%8C%D0%BD%D1%8B%D0%B9+%D0%BF%D0%BE%D1%80%D1%82%D0%B0%D0%BB+%D0%9A%D1%80%D0%B0%D0%BA%D0%B5%D0%BD%3A+%5B%D1%81%D1%81%D1%8B%D0%BB%D0%BA%D0%B0+%D0%BD%D0%B0+%D0%BA%D1%80%D0%B0%D0%BA%D0%B5%D0%BD-%3Ehttps%3A//tobyrush.com/theorywiki/index.php%3Ftitle%3DFive_Incredibly_Useful_Best_Sites_For_Small_Businesses%5D+-%3E+https%3A//www.pawnplusnorman.com/question/time-examined-ways-to-best-sites-2/.+%D0%97%D0%B4%D0%B5%D1%81%D1%8C+%D0%BA%D0%B0%D0%B6%D0%B4%D1%8B%D0%B9+%D0%BA%D0%BB%D0%B8%D0%B5%D0%BD%D1%82+%0D%0A%D1%81%D0%BC%D0%BE%D0%B6%D0%B5%D1%82+%D0%BD%D0%B0%D0%B9%D1%82%D0%B8+%D0%BF%D0%BE%D0%B4%D1%85%D0%BE%D0%B4%D1%8F%D1%89%D0%B8%D0%B9+%D1%82%D0%BE%D0%B2%D0%B0%D1%80+%D0%B8%D0%BB%D0%B8+%D0%BE%D1%82%D0%B4%D0%B5%D0%BB%D1%8C%D0%BD%D1%83%D1%8E+%D0%BA%D0%B0%D1%82%D0%B5%D0%B3%D0%BE%D1%80%D0%B8%D1%8E.%0D%0A%D0%9F%D0%BB%D0%BE%D1%89%D0%B0%D0%B4%D0%BA%D0%B0+%D0%BF%D0%BE%D0%BB%D0%BD%D0%BE%D1%81%D1%82%D1%8C%D1%8E+%D0%&page=contact&contenu=mentions&site=http%3A%2F%2Fcupak.sk%2Findex.php&option=com_phocaguestbook&id=1&first=&firstname=Cherie&message=&formulaire_action=contact&formulaire_action_args=3Vgdna7jCvKpmxKL9qHiOfDFV554LOWljCiQ4OCqebTRkYEQyuOQXrX3XMqN8ZFnkEgXToVashGq1608yzawfhReDNqwpnzN&formulaire_action_sign=&site=https%3A%2F%2Fcubictd.wiki%2Findex.php%2FHow_To_Get_A_Fabulous_Best_Sites_On_A_Tight_Budget&firstname=Irma&email=irma.hensman%40yahoo.com&message=%D0%9D%D0%B0+%D0%BF%D0%BB%D0%B0%D1%82%D1%84%D0%BE%D1%80%D0%BC%D0%B5+Kraken+%5B%D0%BA%D1%80%D0%B0%D0%BA%D0%B5%D0%BD+%D1%81%D1%81%D1%8B%D0%BB%D0%BA%D0%B0+%D1%82%D0%BE%D1%80-%3Ehttps://cubictd.wiki/index.php/How_To_Get_A_Fabulous_Best_Sites_On_A_Tight_Budget%5D+-%3E+http://royalamg.com/bbs/board.php%3Fbo_table%3Dfree%26wr_id%3D357223+%D0%B8%D0%BC%D0%B5%D0%B5%D1%82%D1%81%D1%8F+%0D%0A%D0%B1%D0%BE%D0%BB%D0%B5%D0%B5+5+000+%D0%B4%D0%B8%D0%BB%D0%B5%D1%80%D0%BE%D0%B2+%D0%BF%D1%80%D0%B5%D0%B4%D0%BB%D0%B0%D0%B3%D0%B0%D1%8E%D1%89%D0%B8%D1%85+%D0%B1%D0%BE%D0%B3%D0%B0%D1%82%D1%8B%D0%B9+%0D%0A%D0%B0%D1%81%D1%81%D0%BE%D1%80%D1%82%D0%B8%D0%BC%D0%B5%D0%BD%D1%82+%D0%BF%D1%80%D0%BE%D0%B4%D1%83%D0%BA%D1%82%D0%BE%D0%B2.+%D0%97%D0%B4%D0%B5%D1%81%D1%8C+%D0%B2%D1%8B+%D0%BD%D0%B5%D0%BF%D1%80%D0%B5%D0%BC%D0%B5%D0%BD%D0%BD%D0%BE+%0D%0A%D0%BD%D0%B0%D0%B9%D0%B4%D0%B5%D1%82%D0%B5+%D0%BD%D1%83%D0%B6%D0%BD%D1%8B%D0%B9+%D0%B2%D0%B0%D1%80%D0%B8%D0%B0%D0%BD%D1%82.+%D0%9A%D1%80%D0%BE%D0%BC%D0%B5+%D1%82%D0%BE%D0%B3%D0%BE%2C+%0D%0A%D0%BD%D0%B0+Kraken+%D0%B5%D1%81%D1%82%D1%8C+%D0%B2%D0%BE%D0%B7%D0%BC%D0%BE%D0%B6%D0%BD%D0%BE%D1%81%D1%82%D1%8C+%D0%BE%D0%B1%D0%BC%D0%B5%D0%BD%D0%B0+%D0%B1%D0%B8%D1%82%D0%BA%D0%BE%D0%B8%D0%BD+%D0%BD%D0%B0+%D0%9A%D0%B8%D0%B2%D0%B8%2C+%0D%0A%D0%B0%D0%BB%D1%8C%D1%82%D0%B5%D1%80%D0%BD%D0%B0%D1%82%D0%B8%D0%B2%D0%B0+%D0%B8%D1%81%D0%BF%D0%BE%D0%BB%D1%8C%D0%B7%D0%BE%D0%B2%D0%B0%D0%BD%D0%B8%D1%8E+Telegram+-+%D0%B0%D0%BD%D0%BE%D0%BD%D0%B8%D0%BC%D0%BD%D1%8B%D0%B5+%D1%87%D0%B0%D1%82%D1%8B+%D0%BC%D0%B5%D0%B6%D0%B4%D1%83+%D0%BA%D0%BB%D0%B8%D0%B5%D0%BD%D1%82%D0%B0%D0%BC%D0%B8+%D1%87%D0%B5%D1%80%D0%B5%D0%B7+Privnote.%0D%0A%D0%95%D1%81%D0%BB%D0%B8+%D0%B2%D0%BE%D0%B7%D0%BD%D0%B8%D0%BA%D0%B0%D1%8E%D1%82+%D1%81%D0%BF%D0%BE%D1%80%D0%BD%D1%8B%D0%B5+%D1%81%D0%B8%D1%82%D1%83%D0%B0%D1%86%D0%B8%D0%B8%2C+%D0%BC%D0%BE%D0%B6%D0%BD%D0%BE+%D1%80%D0%B0%D0%B7%D1%80%D0%B5%D1%88%D0%B8%D1%82%D1%8C+%D0%B8%D1%85+%D1%87%D0%B5%D1%80%D0%B5%D0%B7+%D1%84%D1%83%D0%BD%D0%BA%D1%86%D0%B8%D1%8E+%22%D0%B4%D0%B8%D1%81%D0%BF%D1%83%D1%82%22+%D1%81+%D0%BC%D0%BE%D0%B4%D0%B5%D1%80%D0%B0%D1%82%D0%BE%D1%80%D0%BE%D0%BC+%D0%B8%D0%BB%D0%B8+%D0%BF%D1%80%D0%BE%D0%B4%D0%B0%D0%B2%D1%86%D0%BE%D0%BC.%0D%0A%0D%0A%D0%98+%D1%8D%D1%82%D0%BE+%D1%82%D0%BE%D0%BB%D1%8C%D0%BA%D0%BE+%D0%BD%D0%B5%D0%BA%D0%BE%D1%82%D0%BE%D1%80%D1%8B%D0%B5+%D0%B8%D0%B7+%D1%84%D0%B8%D1%88%D0%B5%D0%BA+%D0%B8+%D1%83%D0%BD%D0%B8%D0%BA%D0%B0%D0%BB%D1%8C%D0%BD%D0%BE%D1%81%D1%82%D0%B5%D0%B9%2C%0D%0A%D0%BA%D0%BE%D1%82%D0%BE%D1%80%D1%8B%D0%B5+%D0%BC%D0%BE%D0%B6%D0%BD%D0%BE+%D0%BD%D0%B0%D0%B9%D1%82%D0%B8+%D0%BD%D0%B0+%D0%BE%D1%82%D0%B4%D0%B5%D0%BB%D1%8C%D0%BD%D0%BE%D0%B9+%0D%0A%D1%81%D1%82%D1%80%D0%B0%D0%BD%D0%B8%D1%86%D0%B5+%D0%BC%D0%B0%D1%80%D0%BA%D0%B5%D1%82%D0%B0%2C+%D0%BF%D0%BE%D1%81%D0%B2%D1%8F%D1%89%D0%B5%D0%BD%D0%BD%D0%BE%D0%B9+%D1%84%D1%83%D0%BD%D0%BA%D1%86%D0%B8%D1%8F%D0%BC+%D0%B8+%D0%BE%D1%81%D0%BE%D0%B1%D0%B5%D0%BD%D0%BD%D0%BE%D1%81%D1%82%D1%8F%D0%BC+%D0%B4%D0%B0%D0%BD%D0%BD%D0%BE%D0%B3%D0%BE+%D1%80%D0%B5%D1%81%D1%83%D1%80%D1%81%D0%B0.&ok=Envoyer, которые откроют доступ к сайту всего за несколько секунд.
Aja
Кракен onion - это уникальная площадка, и мы предоставляем вам ссылку на официальное зеркало от администрации проекта. Вам нужно всего лишь кликнуть по этой ссылке, зайти на маркет и подобрать нужные продукты. Наша площадка полностью безопасна, работает круглосуточно и не требует подключения Тор или VPN. Просто перейдите на официальный магазин Kraken 2krn -> https://www.course.kwtc.ac.th/index.php?name=webboard&file=read&id=50165 и начните работу с проектом. Для этого потребуется всего несколько простых регистрационных шагов и несколько кликов мышью. А если у вас возникнут любые трудности, проблемы или вопросы, всегда можете обратиться к администрации проекта - мы всегда готовы помочь.
Margareta
Хотите найти площадку, где можно купить разнообразные продукты? Рекомендуем обратить внимание на официальный портал Kraken: raken12 +at -> http://o993028a.beget.tech/profile.php?id=253606. Здесь каждый клиент сможет найти подходящий товар или отдельную категорию. Площадка полностью скрыта и обеспечивает конфиденциальность. Покупки можно совершать, не беспокоясь о потере денег или личных данных. Кроме того, Kraken onion не просто частный магазин, а уникальный маркетплейс. Здесь 2krn предлагают свои товары тысячи поставщиков, и всегда можно обнаружить что-то максимально выгодное. Советуем пройти быструю регистрацию на сервисе Кракен onion и перейти в магазин, где вы легко найдете нужные товары. При возникновении трудностей, администрация сайта всегда готова предоставить ассистенцию.
Emil
промокод 1xbet на сегодня бесплатно 1xbet promocodde [https://telegra.ph/]
Karine
Кракен даркнет кракен даркнет маркет -> http://apbt.online-pedigrees.com/modules.php?name=Your_Account&op=userinfo&username=FelicaHold - безопасная площадка, на которой каждый покупатель найдет товар на свой вкус. На данный момент она работает, обеспечивая полную анонимность и безопасность, при этом не требуется Kraken Tor соединение. Все, что необходимо - перейти по активной ссылке кракен онион -> https://www.so-toulouse.com/spip.php?page=contact&contenu=mentions&page=contact&contenu=mentions&site=http%3A//cupak.sk/index.php&option=com_phocaguestbook&id=1&first&p&page=contact&contenu=mentions&site=http%3A&page=contact&contenu=mentions&site=http%3A%2F%2Fcupak.sk%2Findex.php&option=com_phocaguestbook&id=1&first=&p=&formulaire_action=contact&formulaire_action_args=3Vgdna7jCvKpmxKL9qHiOfDFV554LOWljCiQ4OCqebTRkYEQyuOQXrX3XMqN8ZFnkEgXToVashGq1608yzawfhReDNqwpnzN&formulaire_action_sign=&site=https%3A%2F%2Ffactbook.info%2Findex.php%2FUser%3AThao9281024746&firstname=Melanie&email=melanie.brush%40facebook.com&message=%D0%A5%D0%BE%D1%82%D0%B8%D1%82%D0%B5+%D0%BD%D0%B0%D0%B9%D1%82%D0%B8+%D0%BF%D0%BB%D0%BE%D1%89%D0%B0%D0%B4%D0%BA%D1%83%2C+%D0%B3%D0%B4%D0%B5+%D0%BC%D0%BE%D0%B6%D0%BD%D0%BE+%0D%0A%D0%BF%D1%80%D0%B8%D0%BE%D0%B1%D1%80%D0%B5%D1%81%D1%82%D0%B8+%D1%80%D0%B0%D0%B7%D0%BD%D0%BE%D0%BE%D0%B1%D1%80%D0%B0%D0%B7%D0%BD%D1%8B%D0%B5+%D0%BF%D1%80%D0%BE%D0%B4%D1%83%D0%BA%D1%82%D1%8B%3F%0D%0A%0D%0A%D0%A1%D0%BE%D0%B2%D0%B5%D1%82%D1%83%D0%B5%D0%BC+%D1%80%D0%B0%D1%81%D1%81%D0%BC%D0%BE%D1%82%D1%80%D0%B5%D1%82%D1%8C+%D0%BE%D1%84%D0%B8%D1%86%D0%B8%D0%B0%D0%BB%D1%8C%D0%BD%D1%8B%D0%B9+%D0%BF%D0%BE%D1%80%D1%82%D0%B0%D0%BB+%D0%9A%D1%80%D0%B0%D0%BA%D0%B5%D0%BD:%0D%0A%5Bkraken+%D0%BE%D1%84%D0%B8%D1%86%D0%B8%D0%B0%D0%BB%D1%8C%D0%BD%D1%8B%D0%B9-%3Ehttps://factbook.info/index.php/User:Thao9281024746%5D+-%3E+%0D%0Ahttp://absoluttorg.ru/component/k2/item/11.+%D0%97%D0%B4%D0%B5%D1%81%D1%8C+%D0%BA%D0%B0%D0%B6%D0%B4%D1%8B%D0%B9+%D0%BA%D0%BB%D0%B8%D0%B5%D0%BD%D1%82+%D1%81%D0%BC%D0%BE%D0%B6%D0%B5%D1%82+%D0%BD%D0%B0%D0%B9%D1%82%D0%B8+%D0%BF%D0%BE%D0%B4%D1%85%D0%BE%D0%B4%D1%8F%D1%89%D0%B8%D0%B9+%D1%82%D0%BE%D0%B2%D0%B0%D1%80+%D0%B8%D0%BB%D0%B8+%D0%BE%D1%82%D0%B4%D0%B5%D0%BB%D1%8C%D0%BD%D1%83%D1%8E+%D0%BA%D0%B0%D1%82%D0%B5%D0%B3%D0%BE%D1%80%D0%B8%D1%8E.%0D%0A%D0%9F%D0%BB%D0%BE%D1%89%D0%B0%D0%B4%D0%BA%D0%B0+%D0%BF%D0%BE%D0%BB%D0%BD%D0%BE%D1%81%D1%82%D1%8C%D1%8E+%D0%B0%D0%BD%D0%BE%D0%BD%D0%B8%D0%BC%D0%BD%D0%B0+%D0%B8+%D0%BE%D0%B1%D0%B5%D1%81%D0%BF%D0%B5%D1%87%D0%B8%D0%B2%D0%B0%D0%B5%D1%82+%D0%BA%D0%BE%D0%BD%D1%84%D0%B8%D0%B4%D0%B5%D0%BD%D1%86%D0%B8%D0%B0%D0%BB%D1%8C%D0%BD%D0%BE%D1%81%D1%82%D1%8C.%0D%0A%0D%0A%D0%9F%D0%BE%D0%BA%D1%83%D0%BF%D0%BA%D0%B8+%D0%BC%D0%BE%D0%B6%D0%BD%D0%BE+%D0%BE%D1%81%D1%83%D1%89%D0%B5%D1%81%D1%82%D0%B2%D0%BB%D1%8F%D1%82%D1%8C%2C+%D0%BD%D0%B5+%D0%B1%D0%B5%D1%81%D0%BF%D0%BE%D0%BA%D0%BE%D1%8F%D1%81%D1%8C+%D0%BE+%D0%BF%D0%BE%D1%82%D0%B5%D1%80%D0%B5+%D1%81%D1%80%D0%B5%D0%B4%D1%81%D1%82%D0%B2+%D0%B8%D0%BB%D0%B8+%0D%0A%D0%BB%D0%B8%D1%87%D0%BD%D1%8B%D1%85+%D0%B4%D0%B0%D0%BD%D0%BD%D1%8B%D1%85.+%D0%9A%D1%80%D0%BE%D0%BC%D0%B5+%D1%82%D0%BE%D0%B3%D0%BE%2C+%D0%9A%D1%80%D0%B0%D0%BA%D0%B5%D0%BD+onion+%D0%BD%D0%B5+%D0%BF%D1%80%D0%BE%D1%81%D1%82%D0%BE+%D1%87%D0%B0%D1%81%D1%82%D0%BD%D1%8B%D0%B9+%D0%BC%D0%B0%D0%B3%D0%B0%D0%B7%D0%B8%D0%BD%2C+%0D%0A%D0%B0+%D1%83%D0%BD%D0%B8%D0%BA%D0%B0%D0%BB%D1%8C%D0%BD%D1%8B%D0%B9+%D0%BC%D0%B0%D1%80%D0%BA%D0%B5%D1%82%D0%BF%D0%BB%D0%B5%D0%B9%D1%81.%0D%0A%D0%97%D0%B4%D0%B5%D1%81%D1%8C+%D0%BA%D1%80%D0%B0%D0%BA%D0%B5%D0%BD+%D0%BE%D0%BD%D0%BB%D0%B0%D0%B9%D0%BD+%D0%BF%D1%80%D0%B5%D0%B4%D0%BB%D0%B0%D0%B3%D0%B0%D1%8E%D1%82+%D1%81%D0%B2%D0%BE%D0%B8+%D1%82%D0%BE%D0%B2%D0%B0%D1%80%D1%8B+%0D%0A%D1%82%D1%8B%D1%81%D1%8F%D1%87%D0%B8+%D0%BF%D0%BE%D1%81%D1%82%D0%B0%D0%B2%D1%89%D0%B8%D0%BA%D0%BE%D0%B2%2C+%D0%B8+%D0%B2%D1%81%D0%B5%D0%B3%D0%B4%D0%B0+%D0%BC%D0%BE%D0%B6%D0%BD%D0%BE+%D0%BE%D0%B1%D0%BD%D0%B0%D1%80%D1%83%D0%B6%D0%B8%D1%82%D1%8C+%D1%87%D1%82%D0%BE-%D1%82%D0%BE+%D0%BC%D0%B0%D0%BA%D1%81%D0%B8%D0%BC%D0%B0%D0%BB%D1%8C%D0%BD%D0%BE+%D0%B2%D1%8B%D0%B3%D0%BE%D0%B4%D0%BD%D0%BE%D0%B5.%0D%0A%D0%A1%D0%BE%D0%B2%D0%B5%D1%82%D1%83%D0%B5%D0%BC+%D0%BF%D1%80%D0%BE%D0%B9%D1%82%D0%B8+%D0%B1%D1%8B%D1%81%D1%82%D1%80%D1%83%D1%8E+%D1%80%D0%B5%D0%B3%D0%B8%D1%81%D1%82%D1%80%D0%B0%D1%86%D0%B8%D1%8E+%D0%BD%D0%B0+%D1%81%D0%B5%D1%80%D0%B2%D0%B8%D1%81%D0%B5+%0D%0A%D0%9A%D1%80%D0%B0%D0%BA%D0%B5%D0%BD+onion+%D0%B8+%D0%BF%D0%B5%D1%80%D0%B5%D0%B9%D1%82%D0%B8+%D0%B2+%D0%BC%D0%B0%D0%B3%D0%B0%D0%B7%D0%B8%D0%BD%2C+%D0%B3%D0%B4%D0%B5+%D0%B2%D1%8B+%D0%BB%D0%B5%D0%B3%D0%BA%D0%BE+%D0%BE%D0%B1%D0%BD%D0%B0%D1%80%D1%83%D0%B6%D0%B8%D1%82%D0%B5+%D0%BD%D1%83%D0%B6%D0%BD%D1%8B%D0%B5+%D0%BF%D1%80%D0%BE%D0%B4%D1%83%D0%BA%D1%82%D1%8B.%0D%0A%D0%9F%D1%80%D0%B8+%D0%B2%D0%BE%D0%B7%D0%BD%D0%B8%D0%BA%D0%BD%D0%BE%D0%B2%D0%B5%D0%BD%D0%B8%D0%B8+%D0%BF%D1%80%D0%BE%D0%B1%D0%BB%D0%B5%D0%BC%2C+%D0%B0%D0%B4%D0%BC%D0%B8%D0%BD%D0%B8%D1%81%D1%82%D1%80%D0%B0%D1%86%D0%B8%D1%8F+%0D%0A%D1%81%D0%B0%D0%B9%D1%82%D0%B0+%D0%B2%D1%81%D0%B5%D0%B3%D0%B4%D0%B0+%D0%B3%D0%BE%D1%82%D0%BE%D0%B2%D0%B0+%D0%BF%D1%80%D0%B5%D0%B4%D0%BE%D1%81%D1%82%D0%B0%D0%B2%D0%B8%D1%82%D1%8C+%D0%B0%D1%81%D1%81%D0%B8%D1%81%D1%82%D0%B5%D0%BD%D1%86%D0%B8%D1%8E.&ok=Envoyer , пройти авторизацию и начать пользоваться анонимной торговой площадкой. Независимо от того, какие именно товары вам необходимы - Кракен магазин поможет в этом вопросе. На сайте можно воспользоваться быстрым поиском по ключевым словам, или просто рассматривать Kraken магазин, подобрав лучшие вещи для себя в интересной или скрытой категории. Далее останется изучить конкурентов, посмотреть отзывы и оформить заказ на сайте. Все это делается в несколько кликов и при этом максимально просто и безопасно.
Patrick
Хотите уникальную площадку, чтобы купить всё? Рекомендуем посетить веб-платформу Kraken: krn -> https://www.so-toulouse.com/spip.php?page=contact&contenu=mentions&page=contact&contenu=mentions&site=http%3A//cupak.sk/index.php&option=com_phocaguestbook&id=1&first&p&page=contact&contenu=mentions&site=http%3A%2F%2Fcupak.sk%2Findex.php&option=com_phocaguestbook&id=1&first=&p=&site=http%3A%2F%2Fforum.Artefakt.cz%2F%2Fprofile.php%3Fid%3D269688&firstname=Rae&message=Hi+there%2C+just+wanted+to+mention%2C+I+loved+this+blog+post.%0D%0AIt+was+helpful.+Keep+on+posting%21%0D%0A%0D%0Amy+web-site+...+%5Bhttp%3A%2F%2Fforum.Artefakt.cz%2F%2Fprofile.php%3Fid%3D269688-%3Ehttp%3A%2F%2Fforum.Artefakt.cz%2F%2Fprofile.php%3Fid%3D269688%5D&ok=Envoyer&page=contact&contenu=mentions&site=http%3A%2F%2Fcupak.sk%2Findex.php&option=com_phocaguestbook&id=1&first=&p=&firstname=Rae&message=Hi%2Bthere%2C%2Bjust%2Bwanted%2Bto%2Bmention%2C%2BI%2Bloved%2Bthis%2Bblog%2Bpost.%0D%0AIt%2Bwas%2Bhelpful.%2BKeep%2Bon%2Bposting%21%0D%0A%0D%0Amy%2Bweb-site%2B...%2B%5Bhttp%3A%2F%2Fforum.Artefakt.cz%2F%2Fprofile.php%3Fid%3D269688-%3Ehttp%3A%2F%2Fforum.Artefakt.cz%2F%2Fprofile.php%3Fid%3D269688%5D&ok=Envoyer&formulaire_action=contact&formulaire_action_args=3Vgdna7jCvKpmxKL9qHiOfDFV554LOWljCiQ4OCqebTRkYEQyuOQXrX3XMqN8ZFnkEgXToVashGq1608yzawfhReDNqwpnzN&formulaire_action_sign=&site=https%3A%2F%2Fwww.thegowiki.com%2Fwiki%2FThe_Best_Sites_Mystery&firstname=Darby&email=darbyhodson%40yahoo.com&message=%D0%9A%D1%80%D0%B0%D0%BA%D0%B5%D0%BD+-+%D0%B3%D0%BB%D0%B0%D0%B2%D0%BD%D1%8B%D0%B9+%D0%B2%D0%B5%D0%B1%D1%81%D0%B0%D0%B9%D1%82+%D0%B3%D0%B8%D0%B3%D0%B0%D0%BD%D1%82%D1%81%D0%BA%D0%BE%D0%B3%D0%BE+%D1%80%D1%8B%D0%BD%D0%BA%D0%B0+%D1%82%D0%BE%D1%80%D0%B3%D0%BE%D0%B2%D0%BB%D0%B8+%D0%B2+%D0%A0%D0%A4.%0D%0A%D0%A2%D1%83%D1%82+kraken+%D1%81%D1%81%D1%8B%D0%BB%D0%BA%D0%B0++%D0%B2%D1%8B+%D0%BE%D0%B1%D0%BD%D0%B0%D1%80%D1%83%D0%B6%D0%B8%D1%82%D0%B5+%D1%80%D0%B0%D0%B7%D0%BD%D0%BE%D0%BE%D0%B1%D1%80%D0%B0%D0%B7%D0%BD%D1%8B%D0%B5+%D1%82%D0%BE%D0%B2%D0%B0%D1%80%D1%8B%2C%0D%0A%D1%81%D0%BE%D0%BE%D1%82%D0%B2%D0%B5%D1%82%D1%81%D1%82%D0%B2%D1%83%D1%8E%D1%89%D0%B8%D0%B5+%D0%BB%D1%8E%D0%B1%D1%8B%D0%BC+%D0%B2%D0%B0%D1%88%D0%B8%D0%BC+%D0%B7%D0%B0%D0%BF%D1%80%D0%BE%D1%81%D0%B0%D0%BC.%0D%0A%D0%9F%D1%80%D0%BE%D0%B9%D0%B4%D0%B8%D1%82%D0%B5+%D0%B1%D1%8B%D1%81%D1%82%D1%80%D1%83%D1%8E+%D1%80%D0%B5%D0%B3%D0%B8%D1%81%D1%82%D1%80%D0%B0%D1%86%D0%B8%D1%8E%2C+%D0%B8+%0D%0A%D0%B2%D0%B0%D0%BC+%D0%BE%D1%82%D0%BA%D1%80%D0%BE%D0%B5%D1%82%D1%81%D1%8F+%D0%B4%D0%BE%D1%81%D1%82%D1%83%D0%BF+%D0%BA%D0%BE+%D0%B2%D1%81%D0%B5%D0%BC+%D1%84%D1%83%D0%BD%D0%BA%D1%86%D0%B8%D1%8F%D0%BC+%D0%BF%D0%BB%D0%BE%D1%89%D0%B0%D0%B4%D0%BA%D0%B8.%0D%0A%D0%A1%D1%82%D0%BE%D0%B8%D1%82+%D0%BE%D1%82%D0%BC%D0%B5%D1%82%D0%B8%D1%82%D1%8C%2C+%D1%87%D1%82%D0%BE+%D0%9A%D1%80%D0%B0%D0%BA%D0%B5%D0%BD+onion+%D1%80%D0%B0%D0%B1%D0%BE%D1%82%D0%B0%D0%B5%D1%82+%D0%B1%D0%B5%D0%B7+%D0%B8%D1%81%D0%BF%D0%BE%D0%BB%D1%8C%D0%B7%D0%BE%D0%B2%D0%B0%D0%BD%D0%B8%D1%8F+%D1%82%D0%BE%D1%80%D0%B0.%0D%0A%D0%92%D0%B0%D0%BC+%D0%BF%D1%80%D0%BE%D1%81%D1%82%D0%BE+%D0%BD%D1%83%D0%B6%D0%BD%D0%BE+%D0%BF%D0%B5%D1%80%D0%B5%D0%B9%D1%82%D0%B8+%D0%BF%D0%BE+%D1%81%D1%81%D1%8B%D0%BB%D0%BA%D0%B5+%D0%BD%D0%B0+%D1%81%D0%B0%D0%B9%D1%82+%D0%B8+%D0%B2%D1%8B%D0%BF%D0%BE%D0%BB%D0%BD%D0%B8%D1%82%D1%8C+%D0%B0%D0%B2%D1%82%D0%BE%D1%80%D0%B8%D0%B7%D0%B0%D1%86%D0%B8%D1%8E.%0D%0A%D0%9F%D1%80%D0%B8+%D0%B2%D1%8B%D0%B1%D0%BE%D1%80%D0%B5+%D1%82%D0%BE%D0%B2%D0%B0%D1%80%D0%BE%D0%B2+%D0%B8%D0%BB%D0%B8+%D1%83%D1%81%D0%BB%D1%83%D0%B3+%D1%80%D0%B5%D0%BA%D0%BE%D0%BC%D0%B5%D0%BD%D0%B4%D1%83%D0%B5%D0%BC+%0D%0A%D1%80%D0%B0%D1%81%D1%81%D0%BC%D0%BE%D1%82%D1%80%D0%B5%D1%82%D1%8C+%D1%80%D0%B0%D0%B7%D0%BB%D0%B8%D1%87%D0%BD%D1%8B%D0%B5+%D0%B2%D0%B0%D1%80%D0%B8%D0%B0%D0%BD%D1%82%D1%8B.%0D%0A%D0%9D%D0%B0+%D0%BF%D0%BB%D0%BE%D1%89%D0%B0%D0%B4%D0%BA%D0%B5+%D0%BF%D1%80%D0%B5%D0%B4%D1%81%D1%82%D0%B0%D0%B2%D0%BB%D0%B5%D0%BD%D0%BE+%D0%BC%D0%BD%D0%BE%D0%B6%D0%B5%D1%81%D1%82%D0%B2%D0%BE+%D0%BF%D1%80%D0%B5%D0%B4%D0%BB%D0%BE%D0%B6%D0%B5%D0%BD%D0%B8%D0%B9+%D0%BE%D1%82+%D1%80%D0%B0%D0%B7%D0%BD%D1%8B%D1%85+%D1%82%D0%BE%D1%80%D0%B3%D0%BE%D0%B2%D1%86%D0%B5%D0%B2%2C%0D%0A%D1%82%D0%B0%D0%BA+%D1%87%D1%82%D0%BE%2C+%D0%BF%D0%BE%D1%82%D1%80%D0%B0%D1%82%D0%B8%D0%B2+%D1%87%D1%83%D1%82%D1%8C+%D0%B1%D0%BE%D0%BB%D1%8C%D1%88%D0%B5+%D0%B2%D1%80%D0%B5%D0%BC%D0%B5%D0%BD%D0%B8+%D0%BD%D0%B0+%D0%BF%D0%BE%D0%B8%D1%81%D0%BA%2C+%D0%B2%D1%8B+%D0%BE%D0%B1%D0%BD%D0%B0%D1%80%D1%83%D0%B6%D0%B8%D1%82%D0%B5+%D0%B1%D0%BE%D0%BB%D0%B5%D0%B5+%0D%0A%D0%B2%D1%8B%D0%B3%D0%BE%D0%B4%D0%BD%D1%8B%D0%B5+%D0%BF%D1%80%D0%B5%D0%B4%D0%BB%D0%BE%D0%B6%D0%B5%D0%BD%D0%B8%D1%8F.+%D0%9D%D0%B5+%D1%81%D1%82%D0%BE%D0%B8%D1%82+%D0%B7%D0%B0%D0%BA%D0%B0%D0%BD%D1%87%D0%B8%D0%B2%D0%B0%D1%82%D1%8C+%D0%BF%D0%BE%D0%B8%D1%81%D0%BA+%0D%0A%D0%BF%D0%B5%D1%80%D0%B2%D1%8B%D0%BC+%D0%BF%D0%BE%D0%BF%D0%B0%D0%B2%D1%88%D0%B8%D0%BC%D1%81%D1%8F+%D1%82%D0%BE%D0%B2%D0%B0%D1%80%D0%BE%D0%BC.+%D0%98%D1%81%D1%81%D0%BB%D0%B5%D0%B4%D1%83%D0%B9%D1%82%D0%B5+%D0%B1%D0%BE%D0%BB%D0%B5%D0%B5+%D0%B2%D0%BD%D0%B8%D0%BC%D0%B0%D1%82%D0%B5%D0%BB%D1%8C%D0%BD%D0%BE%2C+%D0%B8+%D1%83+%D0%B2%D0%B0%D1%81+%D0%BE%D0%B1%D1%8F%D0%B7%D0%B0%D1%82%D0%B5%D0%BB%D1%8C%D0%BD%D0%BE+%D0%B1%D1%83%D0%B4%D0%B5%D1%82+%D1%83%D1%81%D0%BF%D0%B5%D1%85.%0D%0A%0D%0A%D0%A3+%D0%BD%D0%B0%D1%81+%D1%82%D0%B0%D0%BA%D0%B6%D0%B5+%D0%B5%D1%81%D1%82%D1%8C+%D0%B0%D0%BA%D1%82%D1%83%D0%B0%D0%BB%D1%8C%D0%BD%D1%8B%D0%B5+%D0%B7%D0%B5%D1%80%D0%BA%D0%B0%D0%BB%D0%B0+%D0%9A%D1%80%D0%B0%D0%BA%D0%B5%D0%BD+%5Bkraken+%D0%BE%D1%84%D0%B8%D1%86%D0%B8%D0%B0%D0%BB%D1%8C%D0%BD%D1%8B%D0%B9+%D1%81%D0%B0%D0%B9%D1%82-%3Ehttps://www.thegowiki.com/wiki/The_Best_Sites_Mystery%5D+%0D%0A-%3E+http://www.smuniverse.com/bbs/board.php%3Fbo_table%3Dsmu4_3_eng%26wr_id%3D239252%2C+%D0%BA%D0%BE%D1%82%D0%BE%D1%80%D1%8B%D0%B5+%D0%BE%D0%B1%D0%B5%D1%81%D0%BF%D0%B5%D1%87%D0%B0%D1%82+%D0%BC%D0%BE%D0%BC%D0%B5%D0%BD%D1%82%D0%B0%D0%BB%D1%8C%D0%BD%D1%8B%D0%B9+%D0%B4%D0%BE%D1%81%D1%82%D1%83%D0%BF+%D0%BA+%D0%B6%D0%B5%D0%BB%D0%B0%D0%B5%D0%BC%D0%BE%D0%BC%D1%83+%D1%80%D0%B5%D1%81%D1%83%D1%80%D1%81%D1%83.&ok=Envoyer . Здесь каждый клиент сможет найти идеальный товар или услугу. Безопасные и конфиденциальные операции - вот залог успешных сделок на Kraken onion. Просто переходите по ссылке, быстро регистрируйтесь и погружайтесь в увлекательный мир кракен даркнет маркета. Это не просто магазин, это своеобразная арена, где тысячи поставщиков предлагают свои товары. Откройте для себя выгодные сделки на Kraken darknet, кракен зеркало сайта, и наслаждайтесь анонимностью в каждой покупке.
Shiela
Хотите найти и приобрести любые сделки без лишних хлопот? Тогда вам точно понравится наш магазин - Kraken кракен зеркало -> https://commoncause.optiontradingspeak.com/index.php/community/profile/kandicenicholso/ . У нас вы можете покупать и продавать абсолютно все, и при этом не беспокоиться о своей анонимности. Мы предлагаем лучшие условия на просторах мирового darknetа и работаем со всеми странами мира. На нашем магазине вы сможете найти все необходимые вам сделки.
ffkxhtegv
Navigating Medical Negligence and Malpractice in India: A Comprehensive Analysis with Landmark Case Laws ffkxhtegv http://www.gs9ju108786haai88g987hri104ybwu5s.org/ [url=http://www.gs9ju108786haai88g987hri104ybwu5s.org/]uffkxhtegv[/url] <a href="http://www.gs9ju108786haai88g987hri104ybwu5s.org/">affkxhtegv</a>
Lashunda
Кракен - авторитетный ресурс анонимной торговой площадки, который является наиболее огромным в СНГ. Если вы ищете ресурс, где можно купить любые товары, то Kraken - отличный выбор. Здесь каждый клиент сможет подобрать подходящий для себя товар или отдельную категорию товаров. Сама площадка полностью анонимна и безопасна. Здесь вы можете совершать покупки, не беспокоясь о потере денег или личных данных. Кроме того, Кракен onion является не частным магазином, а своеобразным маркетплейсом. Здесь kraken market выложены товары тысяч продавцов и магазинов, и всегда можно найти выгодное предложение для себя. При выборе товаров и услуг рекомендуется рассматривать разные предложения, так как на площадке представлены карточки от разных продавцов. Наши актуальные зеркала Кракен как зайти на кракен - https://pwi2.dragonicgames.com - -> https://staging.warainc.org/community/profile/minervatooth65/ откроют доступ к сайту в течение нескольких секунд. Vk1.at.
Brittny
Доставка алкоголя в Екатеринбурге
Hector
Доставка алкоголя в Екатеринбурге
Isabella
На MEGA вы найдете огромный выбор позиций от различных продавцов. Каждый продавец имеет свой рейтинг, отзывы и другую информацию, которая поможет вам выбрать подходящее предложение. Благодаря этому вы можете быть уверены в качестве позиций и надежности продавцов. Вам не понадобится Tor браузер - наша площадка работает без него приложение hidemega.apk. https://mega555net-13.com
Everette
стоимость предоставления юридического адреса
Lynne
Обзор маркетплейса Кракен: Что можно купить и какие особенности у платформы Сегодня расскажу о маркетплейсе кракен гидра даркнет, с которым уже давно работаю. кракен гидра даркнет Это надежный и проверенный ресурс, где можно купить все, что угодно — от электроники до наркотиков. Интерфейс сайта простой и удобный, есть поиск по категориям и товарам. Ассортимент товаров огромный, цены приемлемые. Отдельно хочу отметить профессионализм продавцов. Всегда отвечают на вопросы, помогают с выбором и доставкой. У меня ни разу не было проблем с заказами, все приходило вовремя и в надлежащем виде. Если вы ищете надежный и проверенный маркетплейс в даркнете, то рекомендую кракен. Вы точно останетесь довольны качеством товаров и сервисом.
Angelina
купить поролон мебельный в москве в розницу
Toby
мебельный поролон купить москва
FrancisHails
https://gosznakdublikat.ru/
Edmundovom
Проверьте лицензию казино – это гарантия вашей безопасности и честности игрового процесса. [*]Отзывы других игроков являются ценным источником информации о надежности и качестве обслуживания. [*]Техническая поддержка должна быть доступна круглосуточно, чтобы оперативно решать любые возникающие проблемы [url=http://masyasha.ru/index.php?option=com_k2&view=itemlist&task=user&id=83370]http://masyasha.ru/index.php?option=com_k2&view=itemlist&task=user&id=83370[/url]
Edmundovom
Множество пользователей активно ищут удобные и доступные способы развлечения. Это привело к повышению популярности различных онлайн-сервисов [url=http://shooting-russia.ru/forum/?PAGE_NAME=message&FID=6&TID=15362&TITLE_SEO=15362-kak-uvelichit-svoy-vyigrysh-v-kazino-1vin&MID=15628&result=new#message15628]http://shooting-russia.ru/forum/?PAGE_NAME=message&FID=6&TID=15362&TITLE_SEO=15362-kak-uvelichit-svoy-vyigrysh-v-kazino-1vin&MID=15628&result=new#message15628[/url]
Vincentvek
Наша компания является передовиком производства измерительного обрудования. Уже долгие годы мы производим и обслуживаем датчики температуры, логгеры данных, регистраторы температуры и влажности и термометры. Наше оборудование помогает осуществлять контроль параметров микроклимата в аптеках, на складах, на производствах и в магазинах [url=http://mix-opt.ru/]Тут[/url]
BarryLof
Наша команда уже более 20 лет проектирует, возводит и обслуживает бассейны в Тюмени, Челябинске и Екатеринбурге. Мы используем только современное и проверенное оборудование и материалы. Даем гарантию выполненных работ. Кроме этого, мы являемся официальными поставщиками химии для бассейнов лучших мировых марок [url=http://aqualand11.ru/]Тут[/url]
Davidmerve
Продвижение сайта в поисковых системах Яндекс, Google. Гарантия выполненных работ. Бесплатный аудит сайта [url=https://seo-steam.ru/]Продвижение в Топ[/url]
Chrismum
Уже не удивительно, что кондиционеры становятся неотъемлемым элементом наших домов и офисов. Именно поэтому мы рады предложить вам широкий выбор кондиционеров от лучших мировых брендов по доступным ценам в нашем магазине Enter в Кишиневе [url=https://enter.online/ru/klimaticheskaja-tehnika/conditionery]купить кондиционер[/url]
Steveonele
В критические моменты жизни важно, чтобы похоронное бюро было надежным и профессиональным. Наша статья поможет вам разобраться в разнообразии ритуальных услуг в Алматы и выбрать агентство, которое предложит качественное обслуживание по разумной цене [url=https://teletype.in/@funeralservice/funeralprice2]ритуальные услуги алматы цена[/url]
Steveonele
LAX Long Term Parking: Find secure and affordable options near LAX Airport. Reviews & details to choose the best fit for your trip [url=https://lax-longtermparking.com/]https://lax-longtermparking.com/[/url]
RichardThigo
LGA Long Term Parking: Find secure & affordable options near LaGuardia Airport. Reviews & details to choose the best fit for your trip [url=https://lga-longtermparking.com/]https://lga-longtermparking.com/[/url]
RobertHah
JFK Long Term Parking: Find secure & affordable options near JFK Airport. Reviews & details to choose the best fit for your trip [url=https://jfk-longtermparking.com/]long term parking at jfk airport ny[/url]
hvnom
[url=https://samoylovaoxana.ru/tag/shampan/]Шампань[/url] или [url=https://samoylovaoxana.ru/izrail-razreshil-vezd-neprivitym-inostrancam/]Израиль разрешил въезд непривитым иностранцам[/url] [url=https://samoylovaoxana.ru/otdyh-v-kenii/]Отдых в Кении[/url] https://samoylovaoxana.ru/tag/kipr-zimoj/ Ещё можно узнать: [url=http://yourdesires.ru/fashion-and-style/fashion-trends/1748-kak-vybrat-kurtku-muzhchine-nizkogo-rosta.html]мужская одежда для невысоких мужчин[/url] Горные туры
RobertHah
EWR Long Term Parking: Find secure & affordable options near EWR Airport. Reviews & details to choose the best fit for your trip [url=https://ewr-longtermparking.com/]newark airport long term parking - uncovered self park[/url]
Josephtairl
Люки Шагма - идеальное сочетание функциональности и эстетики для вашего интерьера. Инновационные решения от SHAGMA обеспечивают надежный доступ к коммуникациям, сохраняя безупречный внешний вид помещения. Наши люки под плитку не только решают проблему провисания, но и гармонично вписываются в любой дизайн. Выбирая SHAGMA, вы выбираете качество, долговечность и индивидуальный подход [url=http://gorodskoyportal.ru/moskva/news/society/84489646/]http://gorodskoyportal.ru/moskva/news/society/84489646/[/url]
StephenAlife
Виртуальные карточные и настольные игры также ждут своих поклонников. От блэкджека до покера – испытайте удачу и стратегию [url=https://prosorta.ru/raskroyte-novye-gorizonty-estetiki-i-funkcionalnosti-s-lyukami-shagma/]https://prosorta.ru/raskroyte-novye-gorizonty-estetiki-i-funkcionalnosti-s-lyukami-shagma/[/url]
DonaldVep
Baji Live Casino offers a dynamic and immersive gaming experience with a wide range of games, exciting bonuses, and a user-friendly interface that caters to both novice and seasoned players [url=https://baji-999.org/]https://baji-999.org[/url]
SammieWoria
С каждым годом растет количество людей, выбирающих этот вид досуга. Онлайн-платформы предлагают не только развлечение, но и шанс испытать удачу [url=http://www.icmms.co.kr/bbs/board.php?bo_table=free&wr_id=534890]http://www.icmms.co.kr/bbs/board.php?bo_table=free&wr_id=534890[/url]
JarvisDup
https://tezfiles.cc/
Darrennex
https://www.themoviedb.org/movie/261903-real-gangsters
MichaelLeaby
Регистрация на различных ресурсах, форумах или интернет-магазинах сегодня осуществляется только с применением номера телефона. Ранее для этой цели могла использоваться электронная почта, но сегодня правила изменены [url=https://midgardinfo.com/news/chem_i_komu_vygodna_arenda_telefonnogo_nomera/2024-02-29-15649]https://midgardinfo.com/news/chem_i_komu_vygodna_arenda_telefonnogo_nomera/2024-02-29-15649[/url]
RobertLaf
https://www.publico.es/sociedad/publico.es-nancy-fraser-no-dejar-temor-ultraderecha-lleve-feminismo-liberal.html
JamesInide
Bonus bez depozytu lub innymi slowami darmowy bonus to nic innego jak gratis oferowany przez kasyna online dla swoich graczy [url=https://polscekasyno.pl/casino/hitnspin-casino/]hitnspin casino[/url]
JamesInide
Бесплатный сервис по подбору и ведению сделок с недвижимостью в новостройках Москвы и Московской области! Новые квартиры для жизни, дохода или инвестирования от топовых застройщиков с защитой государства [url=https://www.nedvigimost-1.ru/]купить квартиру недорого[/url]
Williamaremn
В нашем салоне красоты мы заботимся о ваших волосах, создаем безупречный макияж и подчеркиваем вашу естественную красоту, чтобы вы чувствовали себя уверенно и великолепно каждый день https://ekostil-salon.ru/
Philippar
Интерьерная печать на самоклеющейся пленке - это процесс создания качественных полноцветных изображений на самоклеющейся пленке, которая может быть наклеена на различные поверхности [url=https://ivolgaphoto.ru/]печать интерьерная на баннере[/url]
RogelioSoB
Онлайн-платформа для азартных игр представляет собой разнообразный мир развлечений. Здесь игроки могут наслаждаться множеством опций, которые сделают времяпрепровождение увлекательным и захватывающим [url=https://www.guitaramania.ru/forum/?PAGE_NAME=message&FID=2&TID=782&TITLE_SEO=782-legendy-i-mify-o-kazino-gama&MID=3722&result=new#message3722]https://www.guitaramania.ru/forum/?PAGE_NAME=message&FID=2&TID=782&TITLE_SEO=782-legendy-i-mify-o-kazino-gama&MID=3722&result=new#message3722[/url]
PatrickELofe
Монтаж системы видеонаблюдения может потребоваться в самых разных ситуациях. Её устанавливают в частных и загородных домах, промышленных предприятиях, офисах, гаражах и многих других помещениях [url=https://rivara.ru/bezopasnost-v-karmane-vzglyanite-na-mir-cherez-glaza-sistemy-videonablyudeniya/]https://rivara.ru/bezopasnost-v-karmane-vzglyanite-na-mir-cherez-glaza-sistemy-videonablyudeniya/[/url]
LorenzoNef
Article submission websites provide a platform for authors and businesses to publish and promote their content, increasing their online visibility, driving traffic to their websites, and improving their search engine rankings through high-quality backlinks and targeted audience engagement https://globalarticlewarehouse.com
CurtisOxync
Trusted Vavada Casino: 50 Free Spins on Mega Heist Slot bonus review, including details, player's comments, and top bonus codes [url=https://vavadas.pl/vavada-no-deposit-bonus/]vavada kod promocyjny bez depozytu[/url]
MichaelAlomy
Эта компания предоставляет услуги аварийного вскрытия замков в Москве и готова помочь в любое время суток http://vskrytie-zamkov-moskva.su
RickywaypE
One of the top Bitcoin mixers, Cryptomixer is known for being dependable and quick, which is essential if you want to keep your money safe from [url=https://bitcoinmix.cx/]Bitcoin Mixer[/url]
Billybuh
You are credited with 123 Free Spins in the game Gonzo's Quest. Promotions in GonzoCasino 200% to your deposit – Min. deposit 50 $ / Bonus size 200% [url=https://gonzo-casino.pl/]gonzo kasyno[/url]
Matthewvom
Gonzo Casino offers an incredible 123 Free Spins with no deposit required on Gonzos Quest from NetEnt when you sign up for a new player account [url=https://gonzo-casino.pl/123-darmowe-spiny/]kod promocyjny gonzo casino[/url]
RichardBOM
All new players that register via our provided link will receive a no deposit bonus from Fountain Casino. There is a chance to claim €$15 free money [url=https://fontan-casino.pl/bonusy-w-kasynie-fontan/]fontan casino 100[/url]
Davidvomia
Mostbet, a globally recognized sports betting operator, is now fully accessible to Bangladeshi players. Operating under a Curacao gaming license, Mostbet offers a secure and reliable platform for betting on a wide range of sports [url=https://siamfreestyle.com/]Mostbet Bangladesh[/url]
JamesRek
В современном мире цифровые технологии предлагают нам бесконечные возможности. Удобные способы оставаться на связи с тем, что мы любим. Мир развлечений развивается стремительно, предоставляя новые пути для наслаждения любимыми хобби 1вин зеркало [url=https://www.itray.co.kr/bbs/board.php?bo_table=free&wr_id=2948822]https://www.itray.co.kr/bbs/board.php?bo_table=free&wr_id=2948822[/url]
Ursula
плотный поролон
JamesRek
В мире современных технологий и постоянного интернета доступ к любимым игровым платформам стал неотъемлемой частью повседневной жизни. Однако иногда случаются ситуации, когда прямой доступ оказывается невозможным [url=http://rytof.ru/node/16690]http://rytof.ru/node/16690[/url]
JamesDruth
You'll receive the same therapeutic support from us, but it will take place on our online platform through a webchat, like the ones pictured below [url=https://bg.webcamus.com/]https://bg.webcamus.com/[/url]
JamesDruth
The LiveChat web app is your all-in-one tool to manage customer interactions from any device without installation. Just open your favorite browser [url=https://ua.webcamus.com/]https://ua.webcamus.com/[/url]
Brianrix
Encontre a melhor maneira de saber a hora exata no Brasil no site horasbrazil2.top. Nao importa em qual fuso horario voce esteja, nosso site fornece as informacoes mais atuais e precisas sobre o horario. Interface amigavel, acesso rapido e dados exatos - tudo o que voce precisa para estar sempre atualizado. Visite-nos e comprove https://horasbrazil2.top
FrancisHails
https://gosznakdublikat.ru/
LeonardWhila
Kraken darknet - официальная ссылка на зеркало и сайт кракена. Ссылка на кракен онион доступна в любое время! Сделать покупку проще, чем кажется [url=https://krakenpage.com/]кракен официальный сайт зеркало[/url]
Josepherymn
Поиск горящих туров на море из Москвы лучшие цены, горит 15822 тура [url=http://tourhot.ru/]горящие туры вылет из Москвы[/url]
JeffreyBek
Отказное письмо — официальное подтверждение надлежащего уровня качества и безопасности для людей, животных и экологии https://www.sostav.ru/blogs/30357/41753
AnthonyFUS
http://sbornik-zakonov.ru/
Jamessmuts
Сертификат соответствия ИСО 9001 – документ, который выдается по результатам экспертной проверки и подтверждает, что система менеджмента качества (СМК) организации соответствует международному стандарту SO 9001 https://www.sostav.ru/blogs/30357/41792
Jeromepoubs
Отказное письмо (ОП) – это документ, который удостоверяет, что изделие/товар/материал не подлежат обязательной оценке качества и получению сертификата/декларации в определённой системе https://vc.ru/life/1331217-otkaznoe-pismo-gde-poluchit-i-skolko-stoit-oformlenie
Stevenexera
Итоговая цена сертификата ИСО 9001 и сроки проведения работ всегда определяются в индивидуальном порядке. Их можно назвать, только когда заказчик предоставит всю необходимую информацию https://www.sostav.ru/blogs/30357/19844
AllenBor
Вступая в клуб путешественников, вы открываете для себя уникальную возможность исследовать мир с помощью парусника. Этот клуб объединяет людей, которые ценят свободу, приключения и близость к природе. Каждое путешествие — это не просто переход с одного порта в другой, это шанс ощутить ветер в волосах, запах моря и бескрайние горизонты. Члены клуба участвуют в регатах, освоении навыков управления парусником и, конечно, в создании дружеских связей с единомышленниками [url=http://kvazartur.ru/]Официальный сайт[/url]
Alberthib
Срочные займы индивидуальным предпринимателям онлайн. Лучшие предложения краудлендинговых платформ по оформлению займов для ИП на развитие бизнеса [url=http://pvcfinougor.ru/]ооо экспресс займ[/url]
DustinBut
В современном бизнес-среде важность виртуальных номеров растёт. Они предлагают гибкость, мобильность и профессиональный имидж. Одним из лидеров на рынке предоставления таких услуг является компания DID Virtual Numbers [url=https://rafaelabsj56777.mybuzzblog.com/6309077/het-belang-van-een-telegram-telefoonnummer]https://rafaelabsj56777.mybuzzblog.com/6309077/het-belang-van-een-telegram-telefoonnummer[/url]
DustinBut
Цена сертификата соответствия ИСО 9001 всегда рассчитывается индивидуально, так как зависит от ряда факторов: сферы деятельности; количества и местоположения площадок; численности. Сертификат выдается сроком на 3 года, в течение которого организация должна пройти две инспекционные проверки https://teletype.in/@sezdok/stoimost-sertifikata-ISO-9001
GlennPhica
Virtual Phone basic information and a brief history. How a company can create a local or international brand with a 1800 number [url=https://manuelpjzl01098.azzablog.com/27517198/и§Јй”Ѓж–°еЉ еќЎи™љж‹џж‰‹жњєеЏ·-ејЂеђЇз€±жѓ…ж–°зЇ‡з« ]https://manuelpjzl01098.azzablog.com/27517198/и§Јй”Ѓж–°еЉ еќЎи™љж‹џж‰‹жњєеЏ·-ејЂеђЇз€±жѓ…ж–°зЇ‡з« [/url]
Russellmof
SPBKARKAS – стойловое оборудование для ферм КРС (привязного и беспривязного содержания) и других животноводческих комплексов – конюшен, свинокомплексов, козьих ферм, овчарен! Собственное производство: -Стойлового оборудования для привязного и беспривязного содержания КРС; хедлоки, калитки, ограждения; -Стойлового оборудования для коз и овец; -Оборудование для конноспортивных клубов: денники для лошадей, бочки, манежи, левады -Оборудование для свиноводства, свиноферм и свиноводческих комплексов: станки опорос, ожидание, осеменение, хрячник [url=https://spbkarkas.ru/oborudovanie_dlya_ovcharen_i_kozih_ferm/oborudovanie_dlya_soderzhaniya_molochnyh_koz/]Стойловое оборудование[/url]
RichardLit
Перечень документов, необходимых для оформления кредита на открытие и развитие бизнеса с нуля, зависит от требований банка. В пакет могут входить: • государственный идентификационный номер[url=http://mfcfinance.ru/]банк открытие кредит для бизнеса[/url]
JamesTam
Независимый рейтинг производителей, изготавливающих пластиковые окна ПВХ и деревянные окна со стеклопакетами в Минске и всей Беларуси под заказ [url=https://google.by/url?q=https://4top.by/derevyannye-okna-minsk/]деревянные окна цена[/url]
Gregoryhow
Цена сертификата соответствия ИСО 9001 всегда рассчитывается индивидуально, так как зависит от ряда факторов: сферы деятельности; количества и местоположения площадок; численности. Сертификат выдается сроком на 3 года https://teletype.in/@sezdok/optimalnaya-cena-sertifikata-iso09001-v-rossii
DanielRhync
Сертификат соответствия ИСО 9001 – документ, который выдается по результатам экспертной проверки и подтверждает, что система менеджмента качества (СМК) организации соответствует международному стандарту ISO 9001 «Системы менеджмента качества. Требования» либо его национальному аналогу ГОСТ Р ИСО 9001 и своевременно совершенствуется https://vc.ru/u/3200429-marev/1137556-sertifikat-iso-9001-chto-eto-takoe-i-dlya-chego-oformlyayut
JefferyVussy
Приобретение собственного жилья – важное и ответственное решение. Для большинства людей это одно из самых значимых вложений в жизни. Однако накопить нужную сумму бывает непросто. Именно здесь на помощь приходят финансовые инструменты, позволяющие сделать мечту о собственном доме реальностью [url=http://verkehrsknoten.de/index.php/forum/bau-und-ausruestung-stvzo/91365#92331]http://verkehrsknoten.de/index.php/forum/bau-und-ausruestung-stvzo/91365#92331[/url]
DouglasPak
Полный список промокодов Яндекс Путешествий на первый заказ и не только на июль 2024 Актуальные скидки, промокоды и кешбэк на отели и авиабилеты на сервисе [url=https://t.me/sale_travels]скидка на отели яндекс путешествия[/url]
BryantDiarf
Купить биокамин для квартиры – это создать неповторимую атмосферу уюта и тепла у себя в доме [url=https://biocamin.com/product-category/napolnye/]Напольный биокамин купить[/url]
GreggraG
Магистерские диссертации на заказ в Москве. магистерская диссертация на заказ. Оформление заказа: Заполните форму на нашем сайте, указав все необходимые детали вашей магистерской диссертации [url=http://dissertaciya-dlya-studentov.ru/]кандидатская диссертация под ключ[/url]
Charlesbap
Преимущества заказа магистерской диссертации. Самый ценный и невосполнимый ресурс – это время. Часто в магистратуру идут взрослые люди, обремененные семьей и работой, не имеющие возможности потратить несколько месяцев на то, чтобы искать литературные источники, собирать эмпирические данные и писать текст диссертации [url=http://dissertaciya-dlya-studentov.ru/]кандидатская диссертация[/url]
Nina
поролон купить в москве в розницу
HubertNaree
«Аутстаффинг Рейтинг» – рейтинг агентсв, предоставляющих клиентам услуги трудоустройства и ведения документооборота по иностранным работникам в России. Помогаем бизнесу выбрать лучшего подрядчика https://outstaffing-rating.ru/
ChrisStids
VKrutka — программа для безопасной накрутки просмотров, лайков, подписчиков, комментариев с вашим текстом и лайков на комментарии в ВК [url=https://www.vkrutka.ru]накрутка ВКонтакте бесплатно[/url]
Jameshooca
https://kupi-buket63.ru/
Michaelsmete
Tired of reaching someone’s voicemail? It might not be you – it could be your business phone number. Thankfully, you can get a new number thanks to the power of virtual phone numbers [url=https://zory.com.pl/is,w-dzisiejszym-cyfrowym-swiecie-efektywna-i-bezpieczna-komunikacja-jest-kluczowa,270925,944125.html]https://zory.com.pl/is,w-dzisiejszym-cyfrowym-swiecie-efektywna-i-bezpieczna-komunikacja-jest-kluczowa,270925,944125.html[/url]
KennethTug
<a href=https://telegram-znakomstva.ru/>https://telegram-znakomstva.ru/</a>
KennethTug
<a href=https://telegram-znakomstva.ru/>https://telegram-znakomstva.ru/</a>
Craigexons
<a href=https://derglaube.online/>https://derglaube.online/</a>
SamuelVor
<a href=https://hondrostrong-crema.shop/>Web oficial de Hondrostrong en España</a>
Lowelldrutt
<a href=https://lesifflet.cc/>https://lesifflet.cc/</a>
Miltonbus
<a href=https://originals.org.ua/blog/kak-opredelit-poddelku-airpods-otlichija-ot-originala-i-proverka-pered-pokupkoj/>как определить подделку airpods отличие от оригинала и проверка перед покупкой</a>
TerryUnuts
<a href=https://operacziya-uvelichenie-chlena.ru/>увеличение размера полового члена</a>
Michaelsmete
A virtual phone number (sometimes also called a virtual phone line) is a telephone number that's not associated with a specific device or piece of hardware [url=https://www.seydisehirhaber.com/d/52923/sanal-telefon-numarasi-ile-sms-alma-ve-avantajlari]https://www.seydisehirhaber.com/d/52923/sanal-telefon-numarasi-ile-sms-alma-ve-avantajlari[/url]
Hermangoork
<a href=https://polemix.cc/>https://polemix.cc/</a>
Michaelsmete
Virtual Phone basic information and a brief history. How a company can create a local or international brand with a 1800 number [url=https://techfeatured.com/17607/maximizing-business-communications-with-virtual-did-systems]https://techfeatured.com/17607/maximizing-business-communications-with-virtual-did-systems[/url]
smsflynewprofile
[url=https://www.google.pl/url?q=https://sms-fly.pl/auto-sms-sending/]Automatyczne wysylanie SMS-ow[/url] to planowane dostarczanie wiadomosci tekstowych na telefony komorkowe odbiorcow bez koniecznosci recznej interwencji nadawcy. Jest to nowoczesna metoda komunikacji, ktora umozliwia firmom szybka interakcje z klientami.
Stevenunfit
lords.lat - cмотреть фильмы и сериалы бесплатно в хорошем HD качестве [url=https://2022.lords.lat/]https://2022.lords.lat/[/url]
JosephBah
<a href=https://prodvizhenie-vidnoe.ru/>https://prodvizhenie-vidnoe.ru/</a>
Phillippax
MostBet je mezinarodni organizace a jeji webove stranky jsou dostupne s domenou .com. V tomto clanku se zamerime prave na mezinarodni sazkovou kancelar Mostbet.com. Na oficialni webove stranky mezinarodni sazkove kancelare Mostbet.com se lze snadno dostat obejitim blokace. K tomu je treba pouzit prohlizec s rezimem uspory provozu (Opera, Firefox) nebo sluzby VPN. Na domovske strance se nachazi dalsi sekce s obchazenim blokovani a take odkazy na aplikace pro iOS a Android, pres ktere je sazkova kancelar vzdy pristupna [url=https://mostbets-cz.com/metody-vkladu/]https://mostbets-cz.com/metody-vkladu/[/url]
Gregoryswede
<a href=https://prodvizhenie-dolgoprudniy.ru/>раскрутка сайта долгопрудный</a>
Javieredunc
Exploring the Enigmatic World In a realm where luck intertwines with skill and strategy, a mysterious playground beckons. Here, seekers of thrills find themselves drawn into a labyrinthine landscape where fortunes can change in the blink of an eye [url=http://wiki.catfolks.net/doku.php?id=_How_to_Withdraw_Winnings_from_PlayFortuna_Casino]http://wiki.catfolks.net/doku.php?id=_How_to_Withdraw_Winnings_from_PlayFortuna_Casino[/url]
Thomassak
Good News Bible (GNB), also called the Good News Translation (GNT) in the United States, is an English translation of the Bible by the American Bible Society [url=https://bible-history.com/tlb]Living Bible (TLB)[/url]
Michaellon
<a href=https://kitalararasi.org/>https://kitalararasi.org/</a>
Delberttex
<a href=https://prodvizhenie-korolev.ru/>https://prodvizhenie-korolev.ru/</a>
Vincentstuts
<a href=https://webdiana.ru/jenskoe-zdorovye/budem-zdorovi/13237-epitelialnyy-kopchikovyy-hod.html>https://webdiana.ru/jenskoe-zdorovye/budem-zdorovi/13237-epitelialnyy-kopchikovyy-hod.html</a>
Stephensuick
пластиковый лист прозрачный купить <a href=https://polikarbonat-sotovyj.ru/>https://polikarbonat-sotovyj.ru/</a>
Andrewshoot
Мечтаете об уюте и комфорте в тропическом уголке? Каждый год всё больше людей выбирают для себя постоянное место обитания в местах, где солнце светит круглый год [url=http://travelsingh.com/index.php?option=com_k2&view=itemlist&task=user&id=285522]http://travelsingh.com/index.php?option=com_k2&view=itemlist&task=user&id=285522[/url]
DenisFab
Бесплатный доступ к онлайн курсам, тренингам и книгам. Большой выбор образовательных курсов. Скачивайте бесплатно уже сейчас [url=https://piratehub.site]Онлайн курсы от известных блогеров бесплатно[/url]
WaynebeW
Лизинг грузовых автомобилей может стать эффективным решением для ИП, которым необходимо расширение или обновление автопарка без значительных единовременных затрат [url=https://www.sostav.ru/blogs/264343/36658]https://www.sostav.ru/blogs/264343/36658[/url]
Brianhap
Что можно приобрести в лизинг? Вы можете взять в лизинг новый легковой или грузовой автомобиль, спецтехнику от официального дилера или автомобиль любой категории с пробегом [url=http://autopodbor-yaroslavl.ru/]лизинг автотранспорта в[/url]
Jeffreystupt
Лизинг автотранспорта на выгодных условиях. Приобретайте легковой, коммерческий транспорт или спецтехнику в лизинг с максимальной выгодой. Выбрать автомобиль [url=https://wagner-automobile.ru/]купить коммерческий транспорт в лизинг[/url]
Jeffreystupt
Steam aauthenticator is a option of two-step authentication on steam. It provides additional step privacy your nicknames and passwords. If this option is enabled, Steam Aauthenticator asks you for one-time passcode every time , when you login to Steam on a unfamiliar device [url=https://playsoftzone.com/SteamDesktopAuthenticator]steam desktop authenticator[/url]
NelsonTug
Лизинг оборудования для малого бизнеса. Чтобы расширить или модернизировать бизнес потребуется новое оборудование [url=https://bpz-vostok.ru/]лизинг подъёмно транспортное оборудование[/url]
DavidMal
The Steam Guard Mobile Authenticator is a feature of the Steam Mobile App that provides an additional level of security to your Steam account [url=https://playsoftzone.com/SteamDesktopAuthenticator]steam desktop authenticator github[/url]
Jamesdrerb
<a href=https://betera-prilozhenie.ru/>скачать betera</a>
Charliebup
https://www.justmedia.ru/news/russiaandworld/gde-pokatatsya-na-snegokhodakh-v-podmoskovye
DavidMal
Лизинг авто — это аренда, по истечении срока которой транспорт становится собственностью арендатора. То есть арендатор постепенно выкупает автомобиль, которым пользуется [url=https://mashlizing.ru/]калькулятор лизинга автомобиля для юридических[/url]
Francisraf
<a href=https://bk-melbet-promocodes.ru/>промокод на мелбет</a>
Rogertheow
Интерес к недвижимости на живописном острове постоянно растёт. Место это привлекает людей, мечтающих об идеальном уголке для отдыха или постоянного проживания [url=http://artem-energo.ru/forums.php?m=posts&q=19170&n=last#bottom]http://artem-energo.ru/forums.php?m=posts&q=19170&n=last#bottom[/url]
GreggraG
Это внедорожный путеводитель, карта, на которой размещены интересные маршруты и необходимая информация для путешествий на квадроциклах и снегоходах. Вы сможете: Выбрать интересные маршруты и предварительно свершить по ним виртуальное путешествие [url=http://e-k-h.ru/]день рождения на квадроциклах[/url]
DannyBuS
Прокат и аренда квадроциклов в москве и области. Красота подмосковного леса, опьяняющий, чистый воздух, драйв и адреналин ждут вас в этом квадро приключении [url=http://kvadrociklov-prokat.ru/]отдых с прокатом квадроциклов[/url]
Aaronnatry
<a href=https://tdsubyqkdxqku.ru/>интернет сантехника</a>
RobertDrymn
<a href=https://kalkulatoruangtiktok.id/>penghasilan tik tok</a>
AnthonyArcat
<a href=https://sad-gid.com/>https://sad-gid.com/</a>
CarolDum
<a href=https://road-tuning.ru/>https://road-tuning.ru/</a>
Richardjah
Интерес к островным приобретениям привлекает всё больше внимания. Спрос на жильё в этих местах растёт с каждым годом [url=http://csehtamasdalok.erdospince.hu/index.php/forum/belepo-kapu/168961#168959]http://csehtamasdalok.erdospince.hu/index.php/forum/belepo-kapu/168961#168959[/url]
Williamcag
Водительские права категории А и В. Выгодные цены на обучение управлением автомобилем с МКПП и АКПП в автошколе [url=http://avtopoisk43.ru/]обучение права категории б[/url]
Manuelkek
Sayjam is a All-in-one sellers toolset. Making key decisions about your business is more than just relying on an antiquated 5 star “score”. You should be able to quickly and efficiently measure a service, niche, or keyword on multiple levels to decide whether the service you’re about to commit time and energy into will be successful [url=https://sayjam.com]https://sayjam.com[/url]
Williamdah
Мы предлагаем вам возможность освоить искусство управления автомобилем. Здесь вы научитесь всему, что нужно для уверенного вождения [url=http://am_14264130.mongdol.net/bbs/board.php?bo_table=free&wr_id=580160]http://am_14264130.mongdol.net/bbs/board.php?bo_table=free&wr_id=580160[/url]
Manuelkek
https://www.cosmopolitan.com/es/moda/consejos-moda/a35634628/emprender-como-crear-tu-negocio-marca-moda/
JasonDow
Starda Casino, или как его также называют на русском — Казино Старда, представляет собой онлайн платформу для азартных игр и ставок на спорт [url=http://casino-starda-official.top/]старда казино депозит[/url]
JamesVow
Китайские, японские и европейские автомобили. Поставки новых и поддержанных из Китая. Доставка до России с растаможкой и полным юридическим сопровождением [url=https://factbook.info/index.php/User:MindyJ61494638]polar stone 01 купить в москве[/url]
Henrydergo
<a href=https://npointerro.ru/>https://npointerro.ru/</a>
JosueCam
pubg secret basement key <a href=https://gamersjon.com/>https://gamersjon.com/</a>
Ronaldpioth
https://www.cosmopolitan.com/es/moda/consejos-moda/a35634628/emprender-como-crear-tu-negocio-marca-moda/
EdwardpaX
Кому и зачем понадобится оформление сертификата соответствия ГОСТ Р ИСО 9001 в Москве? Сведения актуальны для разных направлений работы. Оформление сертификата ИСО 9001, который будет подтверждать наличие СМК международного образца https://teletype.in/@sezdok/cena-sertifikata-ISO-9001-v-Moskve
Jameswoula
Жизнь на острове – это не только сказка о солнце и море. Это также необходимость найти удобное и подходящее жилье [url=http://www.thedreammate.com/home/bbs/board.php?bo_table=free&wr_id=1551145]http://www.thedreammate.com/home/bbs/board.php?bo_table=free&wr_id=1551145[/url]
Perrycal
https://epsonl210.com
Timothyfluig
Program bonusowy kazdego nowego kasyna online w Polsce obejmuje roznorodne promocje https://kasynadarmowespiny.pl/
Erickicove
Bonus bez depozytu w kasynie to mozliwosc gry w gry kasynowe na prawdziwe pieniadze bez koniecznosci wplacania srodkow na konto https://kasynazbezdepozytu.pl/
Henryesory
W swiecie hazardu w Polsce kasyna online zajmuja szczegolne miejsce, oferujac wygodna mozliwosc przetestowania swojego szczescia i wygrania bez wychodzenia z domu https://grykasynonline.pl/
MichaelFraUh
Если Вы ищите место, где Вашему ребенку будет хорошо? Где он подготовиться к школе и найдет новых друзей? Тогда детский центр Зайка в Орле идеальное решение! У нас работают только профессионалы своего дела [url=https://znayka-orel.ru]Детский центр[/url]
Horaciobadia
Klasyczna gra kazdego kasyna, ktora w pelni oddaje atmosfere ryzyka, to bez watpienia ruletka online w kasynie https://ruletkagra.pl/
Manuelkek
Подробный справочник организаций города Астрахань. У нас вы можете найти все необходимые вам адреса и телефоны организаций. Актуальная информация [url=https://astarakan.ru/]Здесь[/url]
Robertbuige
Wygrywaj z 21 w blackjacku, tworz zwycieskie uklady w pokerze, stawiaj zaklady w kasynie na zywo i baw sie przy najlepszych grach online w kasynie na zywo https://grakasynonazywo.pl/
Nathanrek
<a href=https://sejf-dlja-doma.ru/>купить домашний сейф</a>
PhillipSiz
Профессиональная химчистка ковра или ковролина по разумной цене. Оперативный выезд, быстрая сушка [url=https://fabrika-himchistki.ru/khimchistka-kozhanoj-mebeli/]leather sofa dry cleaning st petersburg[/url]
Malcolmatrox
<a href=https://znayka-orel.ru/>подготовка к школе цена</a>
Michaelhog
Предоставляем возможность купить авто от прямого поставщика по достойной цене. Высококвалифицированные специалисты всегда помогут выбрать именно ту модель автомобиля, которая будет идеально отвечать всем вашим требованиям и пожеланиям [url=http://vykup-auto02.ru]lixiang l9 купить[/url]
LelandTraGs
Изделия без маркировки изготовителя либо с маркировкой запрещающей аквачистку, принимаются в чистку только с согласия Клиента и обрабатываются по существующим технологиям, без претензий к качеству и товарному виду изделия [url=https://fabrika-himchistki.ru/khimchistka-kovrov/]химчистка ковров спб[/url]
Aarondak
<a href=https://operaciya-varikocele.ru/>варикоцеле лечение</a>
Richardjibly
Китайские марки автомобилей список, история и подробное описание популярных китайских авто. Рассказываем о плюсах и минусах [url=http://hyundai-voronezh.ru]lixiang l8[/url]
Walteropefe
Если вы переезжаете, делаете ремонт или не знаете, куда девать несезонное имущество, то аренда склада для хранения вещей решит проблему. Оказываем услуги физическим лицам, предпринимателям и организациям [url=https://self-storage-msk.ru/]Подробнее[/url]
Shawndiord
<a href=https://sejf-dlya-oruzhiya.ru/>сейф для хранения оружия</a>
StevenGew
Заказать алкоголь с доставкой на дом в Раменском и Раменском районе. Мы работаем круглосуточно 24 часа. Доставка ночью от 20 минут [url=https://drinksramenskoe.ru]https://drinksramenskoe.ru[/url]
Kennethzed
<a href=https://xn--80adjkkk3alj.xn--p1ai/>мир квеста</a>
Jerrodlek
http://chatbot-plus.com/
RobertImmiz
<a href=https://ok-business24.ru/services/kadrovye-uslugi/upravlenie-logistikoy/>кадровое сопровождение</a>
Kevinpault
Купон за 2р. предоставляет скидку до 25% на абонементы в сеть фитнес-клубов «Комета». Купон придет на вашу электронную почту и в личный кабинет [url=https://t.me/promokod_kometa]Промокод Комета[/url]
ChrisTeamb
https://ekostil-salon.ru/
logqsexpe
Navigating Medical Negligence and Malpractice in India: A Comprehensive Analysis with Landmark Case Laws [url=http://www.g7hd61e7qaeg8gb74i911en9t6s0595es.org/]ulogqsexpe[/url] <a href="http://www.g7hd61e7qaeg8gb74i911en9t6s0595es.org/">alogqsexpe</a> logqsexpe http://www.g7hd61e7qaeg8gb74i911en9t6s0595es.org/
SamuelMet
Every business needs to select the right social media in this digital era. There are so many of them that it becomes tough sometimes to pick and choose what will work best for your marketing effect [url=https://www.gofundme.com/f/the-truth-behind-buying-followers-likes-views-and-shares]https://www.gofundme.com/f/the-truth-behind-buying-followers-likes-views-and-shares[/url]
RichardJoict
<a href=https://udalenie-polipov-endometriya.ru/>удаление полипа в матке</a>
JosephWoots
Если вы думаете, как сделать накрутку лайков, можно пользоваться различными биржами для покупки лайков [url=https://t.me/s/nakrutit_podpischikov_instagram]накрутка подписчиков Инстаграм сервисы[/url]
Jasonshoof
Ищете, где купить стильный и удобный женский бюстгальтер? Наш интернет-магазин предлагает огромный ассортимент лифчиков, которые подчеркнут вашу индивидуальность и обеспечат максимальный комфорт. Выбирая бюстгальтеры у нас, вы найдете модели на любой вкус и размер. В каталоге представлены классические бюстгальтеры с косточками, удобные спортивные лифчики, нежные кружевные варианты и модели для особых случаев. Мы предлагаем продукцию только от проверенных брендов, которые гарантируют качество и долговечность изделий [url=https://www.wildberries.ru/seller/479523]удобный бюстгальтер[/url]
Andrewnek
Для успешной игры важно учитывать несколько ключевых факторов. Изучите правила, понимание которых поможет вам избежать распространённых ошибок. Не забывайте, что каждый игровой опыт уникален, и не стоит полагаться исключительно на удачу [url=http://www.hansanfood.com/index/bbs/board.php?bo_table=s3_3&wr_id=17180]http://www.hansanfood.com/index/bbs/board.php?bo_table=s3_3&wr_id=17180[/url]
SamuelFef
<a href=https://cvlamaran.com/>https://cvlamaran.com/</a>
Thomasneemi
Услуга по ароматизации и удалению запахов с помощью сухого тумана может быть полезна в различных ситуациях [url=https://www.deodor.shop/product/nejtralizator-zapaha-koshachej-mochi-thornell-cat-attack/]як позбутися запаху котячої сечі в домашніх умовах[/url]
Edwardwax
Mostbet — O‘zbekistondagi mashhur bukmekerlik kompaniyasi va kazino bo‘lib, uning rasmiy sayti Kyurakao litsenziyasiga ega. U qimor o‘yinlari va sport tikish imkoniyatlarini qonuniy ravishda taqdim etadi. O'yinchilar uchun turli xil to'lov usullari, shu jumladan kriptovalyutalar ham mavjud. Sayt, shuningdek, foydalanuvchilar uchun qulay bonuslar, tezkor mijozlarni qo‘llab-quvvatlash va mobil ilovalarni taklif qiladi [url=https://mostbet-uz-now.com/]Mostbet UZ[/url]
Craigantax
One of the best ways to improve your reaction time in online games is to practice regularly. The more you play, the more familiar you will become with the game mechanics and the faster your reactions will be [url=https://moiflower.com/why-cross-platform-play-is-the-future-of-online-gaming-on-mostbet/]https://moiflower.com/why-cross-platform-play-is-the-future-of-online-gaming-on-mostbet/[/url]
AmaliaCQ
[url=https://volga.news/712336/article/natyazhnye-potolki-v-moskve-vse-chto-nuzhno-znat-pered-ustanovkoj.html]Натяжные потолки в Москве[/url]
AmaliaOU
[url=https://bryansktoday.ru/article/227997?]Натяжные потолки цена[/url]
Richardfluem
Ozbekistan’?n en tan?nm?s bahis sirketi ve casinolardan biri olan Mostbet’in resmi web sitesi Curacao lisans? ile faaliyet gostermektedir. Yasal olarak kumar oyunlar? ve spor bahisleri imkan? sunar. Oyuncular cesitli odeme yontemleri, kripto para birimleri ile odeme yapma imkan?na sahiptir. Site, kullan?c?lar?n rahatl?g? icin bonuslar, h?zl? musteri destegi ve mobil uygulamalar sunmaktad?r [url=https://mostbett-bahisleri.com/]mostbet giriЕџ[/url]
RichardNeamp
<a href=https://namazit.ru/>https://namazit.ru/</a>
Richardfluem
Мы предоставляем полный спектр услуг от А до Я, связанных с ремонтом и обслуживанием современных металлопластиковых, деревянных и алюминиевых окон, а так же предоставляем гарантию на все виды работ. По окончанию ремонтных работ выполним уборку [url=https://vk.com/@-191004714-remont-okon-i-moskitnye-setki-novaya-dyatlovka-kottedzhnyi-p]Ремонт окон и москитные сетки; Новая Дятловка[/url]
Georgemut
Что такое СЕО продвижение сайтов. Продвижение сайта в поисковых системах - это успех бизнеса и его ежедневное развитие. Профессионально настраиваем, ведем и развиваем рекламные кампании в яндекс: ваш сайт 100% заметят [url=http://ok-context.ru/]частный сео оптимизатор[/url]
Richardber
Я - частный web-мастер по созданию, продвижению, администрированию и дальнейшей раскрутке сайтов. Как частный вебмастер, с 2009 года занимаюсь созданием, продвижением, администрированием, обучением созданию и продвижению сайтов [url=http://webmaster-services.ru/]частный сео москва[/url]
AmaliaFV
[url=https://www.bnkomi.ru/data/relize/173093/?]Натяжные потолки фото[/url]
RobertSnort
просушка помещения после затопления <a href=http://prosushka-pomeshchenij-v-moskve.ru/>http://prosushka-pomeshchenij-v-moskve.ru/</a>
AmaliaLL
[url=https://kam.business-gazeta.ru/article/638360]Натяжные потолки[/url]
Michaellom
Multi-platform desktop version of the authenticator, replacing the mobile app steam [url=https://steamauthenticatordesktop.com/]steam desktop authenticator[/url]
MarlonJeali
Список сертифицированных автосервисов на карте по ремонту автомобилей, обслуживанию и диагностике Выберите ближайший автосервис [url=https://фкр.СЂС„/news/2024/zavtra-v-barnaule-startuet-iii-etap-final-xii-letnej-spartakiadyi-uchashhixsya-rossii-2024-po-kikboksingu/]авто в ремонт[/url]
Georgehon
Студия реализует значительный набор работ по администрированию на сайте <a href=https://saitov-podderzhka.ru/>техническая поддержка веб-сайтов</a>. Работники компании обеспечат стабильную деятельность веб-ресурсов и защиту от нежелательных угроз. Реализуем регулярный мониторинг и улучшение ваших проектов, осуществляем архивирование данных и устраняем проблемы. Специалисты студии всегда готовы быстро и профессионально обработать любые возникающие вопросы, чтобы ваш веб-ресурс продолжал быть доступным и надежным для пользователей. Предоставляем услуги по улучшению скорости сайтов, подгонке их под мобильные устройства и добавлению современных функциональных возможностей.Эксперты реализуют улучшение пользовательского опыта и внешнего вида вашего проекта, обеспечат его соответствие современным стандартам и нормам ПС.
BrianScupe
As the leading online betting site, MostBet has quickly gained significant popularity among islanders [url=https://slcpsych.lk/pgs/?mostbet-betting--office-place-bets-up-to-160-000-lkr.html]mostbet casino[/url]
WilliamGeath
https://101-diplom.top/
Keithcob
Multiple authenticator apps are available depending on your device type. Some of the popular Authenticator apps are: steam desktop authenticator github [url=https://steamauthenticatordesktop.com/]steam desktop authenticator github[/url]
Haroldkag
Our betting software is also among the best on the market, with a vast selection of markets and competitive odds. Mostbet company details showcase our dedication to providing you with the best gaming experience, backed by safe and reliable software. Mostbet is the premier gambling and bookie site in India, supplying a wide diversity of games and services to your customers [url=https://voicify.com/articles/mostbet-bd-online-casino-in-bangladesh.html]mostbet app download[/url]
KennethDop
The mainstays of therapy are surgery, radiation therapy, and chemotherapy. Many tumor types require a combination of treatment methods for optimal tumor control [url=https://mostbet.net.pk/]mostbet.net.pk bets on cancer treatment in pakistan[/url]
Timothyhah
The following is a list of white defendants executed for killing a black victim. Executions of white defendants for killing black victims are rare [url=https://mostbet.game/]https://mostbet.game/ kill all niggers[/url]
DavidReurn
Студия оказывает полный комплекс работ по созданию и продвижению лендинг пейдж. Предлагаем большой выбор продающих уникальных и шаблонных дизайнов лендинга [url=https://www.makelanding.ru/]разработка лендинга[/url]
AmaliaBO
[url=https://www.tuvaonline.ru/natjazhnye-potolki-na-kuhne.dhtml]Натяжные потолки на кухню[/url]
Larryciz
The Steam Guard Mobile Authenticator is a feature of the Steam Mobile App that provides an additional level of security to your Steam account [url=https://githab.net/Jessecar96/SteamDesktopAuthenticator/]sda steam[/url]
CharlesSaf
Some people with cancer will have only one treatment. But most people have a combination of treatments, such as surgery with chemotherapy and/or radiation therapy [url=https://mostbet-pk.pk/]cancer drugs for sale[/url]
GregoryRer
Discrimination, the intended or accomplished differential treatment of persons or social groups for reasons of certain generalized traits [url=https://mostbet-pk-app.com/]kill lesbians[/url]
RichardRepay
Mostbet is the best cricket betting app in Pakistan and an ideal platform for enthusiasts as it offers numerous promotions and bonuses [url=https://mostbet-pakistan.com/]anal sex[/url]
Davidwag
Печать фотографий осуществляется на матовой или глянцевой фотобумаге, формат фотографий - 10x13 см. Такие фотографии можно подарить любимым и друзьям на память [url=https://photo-leto.ru/]фотопечать на кружках[/url]
Bryonstops
Steam Desktop Authenticator is your personal guard for your Steam account, offering an increased level of security and convenience. Steam Desktop Authenticator. Desktop version of the Steam authentication mobile app [url=https://githab.net/Jessecar96/SteamDesktopAuthenticator/]steam desktop authenticator github[/url]
Shawndes
Для печати фотографий используется серебросодержащая фотобумага, которая экспонируется, а затем проходит химическую обработку. Такая технология фотопечати обеспечивает максимально широкий цветовой охват и максимальную точность цветопередачи [url=https://photo-leto.ru/]фото на подставке[/url]
Michaelcrymn
Мастерская занимается восстановлением электронной части ABS. ABS является вспомогательной тормозной системой. Вследствие чего является одной из важнейших систем [url=http://interorga.ru/201906211702/sobytiya/novosti/vybiraem-avtoservis-dlya-remonta-avto.html]автосервисы[/url]
MichaelCreap
Проекты домов с коммуникациями и отделкой - доступные цены и отличные планировки. Строительство дома с коммуникациями и отделкой под ключ в Ярославле и Ярославской области [url=https://stroy-dom-yar.ru/]ярославль строительство дома под ключ[/url]
AmaliaVK
[url=http://reporter63.ru/content/view/707928/volshebstvo-potolka-vse-chto-vam-nuzhno-znat-o-natyazhnyh-konstrukciyah-na-kuhnyu]Натяжные потолки на кухню[/url]
HelenEQ
[url=https://polotsk-portal.ru/preobrazhenie-spalni-vse-chto-nuzhno-znat-o-natjazhnyh-potolkah.dhtm]Натяжные потолки в спальню[/url]
Jerryhom
Закажите услуги эвакуатора с манипулятором в Москве по доступной цене! Оперативная помощь в любой точке города и Подмосковья. Безопасная транспортировка автомобилей и спецтехники. Звоните сейчас и получите выгодные условия [url=https://www.drive2.ru/o/Manipulyator77]Эвакуатор манипулятор[/url]
Ramonarisp
<a href=https://trespor.com/>https://trespor.com/</a>
Arthurliz
Являемся российским агрегатором страховых услуг и помогаем вам не только сравнивать стоимость страховок от разных компаний, но и выбирать оптимальный вариант, который не ударит по вашему кошельку. Полностью онлайн, с программой лояльности и с поддержкой 24/7 [url=https://astmal.ru]https://astmal.ru[/url]
Rodneyalolf
<a href=https://krovinka.com/>https://krovinka.com/</a>
Donaldkekly
Moneyman выдает онлайн займы на карту любого банка и вся процедура выдачи занимает не более 15 минут [url=https://moneyman.ru/receive-money/dengi-na-bankovskyu-karty/]получить деньги на карту бесплатно[/url]
HelenBG
[url=https://freesmi.by/kak-sozdat-ujutnuju-spalnju-s-pomoshhju-natjazhnyh-potolkov-sovety-i-rekomendacii.dhtm]Фото натяжных потоков в спальне[/url]
DanielMot
https://www.vice.com/es/article/mb7dv8/creators-estas-fotos-investigan-el-peligro-de-la-tecnologia-y-el-consumismo
WillieHop
Интернет-аптека работает круглосуточно, поэтому наши клиенты имеют возможность уточнить список имеющихся препаратов с определенным действующим веществом [url=https://aboutphuket.ru]https://aboutphuket.ru[/url]
Travisren
Планируйте свой рабочий год эффективно с нашим производственным календарем, актуальная информация о рабочих, выходных и праздничных днях всегда под рукой [url=https://myworkcalendar.ru]производственный календарь[/url]
WillieHop
Следует учитывать нормы Жилищного кодекса, которые регламентируют соблюдение порядка и прав соседних жильцов. Для более детального ознакомления с правами жильцов можно ознакомиться с изменениями в законодательный акт, регулирующий жилищные правоотношения, от 20 марта 2024 год [url=https://agentstvo-profi.ru]https://agentstvo-profi.ru[/url]
Michaelabami
Онлайн-калькулятор ОСАГО рассчитает точную стоимость полиса по тарифам 2020 года. Сравните предложения лидирующих страховых компаний и оформите полис онлайн. Оформление ОСАГО производится в системе страховщика [url=https://arkan-auto.ru]https://arkan-auto.ru[/url]
Romantrody
https://teletype.in/@sezdok/sertifikaciya-iso-27001
HarryEsomi
Наша компания осуществляет разработку лендигов под ключ. В наши услуги входит создание индивидуального дизайна для сайта и реклама проекта [url=https://www.landing-site-design.ru/]создание лендинга Москва[/url]
ScottNed
Оформить электронное ОСАГО онлайн дешево. Расчет стоимости автострахования ОСАГО за 2 минуты на онлайн-калькуляторе. Учитываем все коэффициенты и скидки на ОСАГО за безаварийность [url=https://arshan-kurort.ru]https://arshan-kurort.ru[/url]
HelenWF
[url=http://gubernya63.ru/novosti-partnerov/sovershenstvujte-vashu-spalnju-s-jelegantnymi-natjazhnymi-potolkami.html]Натяжные потолки в спальне цена[/url]
WalterDrili
https://oxflox.com/subject-name/
Terryfoubs
Цены на оформление добровольных сертификатов соответствия в СДС РосПромТест, Сертификация продукции, СМК (ISO), квалификации персонала, эко продукции. Добровольная сертификация продукции на соответствие государственным стандартам в системе добровольной сертификации https://t.me/rospromtest
BrianAlero
Надежный поставщик динамических и статических прокси, сохраняющий стабильность вашей web активности: резидентские прокси - <a href=https://residential-proxy.ru/>https://residential-proxy.ru/</a>
DavidFup
<a href=https://abc-context.ru/seo-prodvizhenie/>abc-context.ru</a>
GlennIcorm
Сертификация ИСО 45001-2020 может быть проведена на любом предприятии независимо от численности персонала и сферы деятельности. Более востребованным получение сертификата ИСО 45001-2020 является для компаний, деятельность которых связана с риском для жизни и здоровья персонал https://teletype.in/@sezdok/chto-takoe-sertifikat-iso-45001
HelenEU
[url=https://worldgonesour.ru/novosti/36679-natyazhnye-potolki-v-vannoy-idealnoe-sochetanie-funkcionalnosti-i-estetiki.html]Натяжные потолки в ванной[/url]
RobertElate
We provide virtual numbers for receiving SMS messages. Online security and Privacy with our virtual number service. Ideal for quick and effortless SMS [url=https://nadwisla24.pl/2024/06/11/poznaj-zalete-polskich-numerow-telefonow-latwosc-uzyskania-i-korzystania/]polski numer telefonu[/url]
HenryBor
https://mostbetpk.app/
KennethCasty
<a href=https://bitlyglo.wordpress.com/2023/11/28/%d0%be%d1%82%d0%b5%d0%bb%d1%8c-glory-%d0%bc%d0%b5%d1%81%d1%82%d0%be-%d0%b3%d0%b4%d0%b5-%d0%bc%d0%b5%d1%87%d1%82%d1%8b-%d1%81%d1%82%d0%b0%d0%bd%d0%be%d0%b2%d1%8f%d1%82%d1%81%d1%8f-%d1%80%d0%b5%d0%b0/>Glory Casino</a>
JordonExink
Online security and Privacy with our virtual number service. We provide virtual numbers for receiving SMS messages. Ideal for quick and effortless SMS [url=][/url]
CharlesCek
Мы — команда специалистов, посвятивших себя поиску лучших домов престарелых. Мы ценим заботу, комфорт и безопасность ваших близких. Наши отзывы и опыт говорят сами за себя. Мы поможем вам сделать правильный выбор, чтобы ваши родные чувствовали себя как дома. Давайте работать вместе [url=https://кто-молодец.СЂС„]дома престарелых[/url]
DonaldNeuse
строительство дома под ключ <a href=https://spbstroymax.ru/>https://spbstroymax.ru/</a>
syegyfsdmh
Navigating Medical Negligence and Malpractice in India: A Comprehensive Analysis with Landmark Case Laws syegyfsdmh http://www.gop7rk4aoxv1468kftb2f13048xo3472s.org/ <a href="http://www.gop7rk4aoxv1468kftb2f13048xo3472s.org/">asyegyfsdmh</a> [url=http://www.gop7rk4aoxv1468kftb2f13048xo3472s.org/]usyegyfsdmh[/url]
RichardSpova
Добровольное медицинское страхование (ДМС) - ваш надежный помощник в обеспечении качественной медицинской помощи. Наша компания предлагает широкий спектр программ ДМС, адаптированных под индивидуальные потребности клиентов. Мы обеспечиваем доступ к лучшим медицинским учреждениям, высококвалифицированным специалистам и современным методам лечения [url=http://most-polis.ru/]что такое дмс[/url]
CharlesCek
Мы собрали рейтинг топ-20 лучших фитнес-клубов в Москве в 2024 году, ориентируясь на вышеперечисленные критерии. Плюс учитывали ценовую политику абонементов и отзывы клиентов [url=https://sport-reforma.ru/]занятие здоровая спина фитнес м беляево[/url]
Pedrogub
https://www.volzsky.ru/press-relize.php?id=19475
PrestonDwela
Are you searching for the ultimate source of Android APK downloads? Look no further than TopAppsFree! Our platform is dedicated to providing you with the latest APKs, ensuring you have access to all the trending applications that can transform your mobile experience [url=https://topappsfree.com/Articles/VPN-Master-The-Ultimate-Guide-to-Internet-Security-and-Privacy]subway surfers[/url]
BryanPyday
<a href=https://t.me/s/denezhnye_igry>https://t.me/s/denezhnye_igry</a>
WilliamErelo
Фитнес в лучших фитнес-клубах у метро Войковская в Москве. Мы подобрали для вас 28 клубов с ценами от 700 до 80 000 руб. А также 61 тренера [url=http://ufit-nahim.ru/]сайт фитнес клуба[/url]
SteveZet
Помните, что правильный выбор места для занятий спортом может существенно повлиять на вашу мотивацию и результативность тренировок [url=https://www.presconconstrucoes.com.br/index.php?option=com_kunena&view=topic&catid=2&id=194&Itemid=151]https://www.presconconstrucoes.com.br/index.php?option=com_kunena&view=topic&catid=2&id=194&Itemid=151[/url]
Mariontrora
Мы предлагаем аренду снегохода, которые позволят Вам получить максимальное удовольствие от катания. В стоимость проката входит: Аренда снегохода выбранной модели на необходимое количество часов; Полный комплект защитной экипировки [url=https://atv-penza.ru/]зимние катание на квадроциклах[/url]
Michaelthymn
В аренду входят не только снегоходы, но и весь необходимый инвентарь. Обязательно надевайте шлем и перчатки перед поездкой, чтобы обеспечить защиту и тепло [url=http://snegohody-shop.ru/]катание на снегоходах балашиха[/url]
Samuelerype
Клининг алкогольных квартир с вывозом мусора <a href=https://uborka-zapushchennyh-kvartir.ru/>https://uborka-zapushchennyh-kvartir.ru/</a>
Williamlex
Мы сочетаем в себе приятный отдых и эффективное сопровождение. Во всех пансионатах созданы комфортные условия проживания для постояльцев: комфортные номера, безбарьерная среда, адаптированные ванные комнаты и коридоры [url=https://xn----htbdrgfmcb8a4c.xn--p1ai]дешевые дома престарелых[/url]
VictorLat
Подайте заявку на микрокредит с дневной процентной ставкой от 0,01% и получите средства на свою карту круглосуточно [url=https://www.planetoday.ru/gde-vzyat-vygodnyj-onlajn-zaem-v-kazahstane/]https://www.planetoday.ru/gde-vzyat-vygodnyj-onlajn-zaem-v-kazahstane/[/url]
JacobFiemo
<a href=https://prodvizhenie-lubertsy.ru/>https://prodvizhenie-lubertsy.ru/</a>
Williamlex
Сертификат соответствия СМК ИСО 9001 не только документально засвидетельствует соответствие стандарту, но и станет значительным вкладом в репутационный капитал компании http://center-sertifikaciya.ru/
JamieSum
СМК на соответствие ГОСТ Р ИСО 9001-2015 сертифицируют в добровольном порядке, однако наличие такого сертификата является показателем качества работы, и этот показатель признается во всем мире [url=https://www.tumblr.com/milaeryomina/760054824700149760/%D0%BC%D0%BE%D0%B9-%D0%BE%D0%BF%D1%8B%D1%82-%D0%BF%D0%BE%D0%BB%D1%83%D1%87%D0%B5%D0%BD%D0%B8%D1%8F-%D1%81%D0%B5%D1%80%D1%82%D0%B8%D1%84%D0%B8%D0%BA%D0%B0%D1%82%D0%B0-%D0%B8%D1%81%D0%BE-9001-%D1%81-%D1%87%D0%B5%D0%BC-%D1%8F]сертификат ИСО 9001[/url]
JefferySen
Привезти технику на ремонт вы можете в самый удобный по расположению сервисный центр. В данный момент успешно функционируют 13 представительств сервисного центра [url=http://remontcentr-stavropol.ru/]ближайший сервисный центр по ремонту телефонов[/url]
WilliamElapy
Промокоды на бездепозитные фриспины в онлайн казино. Вводи промокод, крути слоты и забирай выигрыш уже сегодня [url=https://t.me/platinum_promokod]https://t.me/platinum_promokod[/url]
OscarJuida
https://buzulukmedia.ru/kak-i-kogda-obratitsya-k-spetsialistam-po-vskrytiyu-avtomobiley-poleznye-sovety/
WilliamuteFe
Ремонт бытовой техники и электроники в Москве. Своевременный ремонт бытового оборудования – это гарантия его долгой и исправной работы [url=http://spb-remont-iphone.ru]сервисный центр ремонт моноблоков[/url]
Jaredter
https://sabiiborno.com/
Ronaldpam
Кольпоскопия Плюс — специализированный сайт клиники «Гинеколог Плюс» в Пятигорске, посвященный кольпоскопии. Мы предлагаем высокоточные исследования для раннего выявления заболеваний шейки матки. Опытные специалисты, современное оборудование и индивидуальный подход — всё для вашего здоровья и спокойствия [url=https://xn-----6kchhabn0adteizrbepgqvr6hyj.xn--p1ai/%d0%be%d0%bf%d1%8b%d1%82%d0%bd%d1%8b%d0%b5-%d0%b2%d1%80%d0%b0%d1%87%d0%b8-%d0%ba%d0%bb%d0%b8%d0%bd%d0%b8%d0%ba%d0%b8-%d0%b3%d0%b8%d0%bd%d0%b5%d0%ba%d0%be%d0%bb%d0%be%d0%b3-%d0%bf%d0%bb%d1%8e%d1%81/]Опытные врачи клиники[/url]
StevenPoosy
Наша клиника использует современные методы лечения бесплодия и минимально инвазивные технологии, такие как лапароскопическая хирургия, что позволяет сократить время восстановления и снизить риски. В Гинеколог Плюс вы получите экспертную помощь в гинекологии от ведущих специалистов, которые применяют современные методы лечения и предлагают индивидуальный подход к каждой пациентк [url=https://xn-----elccadjfufrggzrbgpwuq9z.xn--p1ai/kak-proehat/]Как проехать[/url]
Davidrew
Вы можете купить справки в Москве в нашей клинике https://ossis-med.ru/
Arnoldber
Вы можете купить справку в медцентре https://mymednews.ru/ с доставкой по Москве.
JosephHix
Добро пожаловать в клинику «Гинеколог Плюс» – специализированное медицинское учреждение, где мы заботимся о вашем здоровье с особым вниманием и профессионализмом. Наша миссия – обеспечить каждой женщине возможность получать качественное медицинское обслуживание в комфортных условиях [url=https://xn----etbahmcemjrnb1e.xn--p1ai/930-2/]Услуги и цены[/url]
Arnoldber
Вы можете купить медсправку в нашем мед центре https://medical-sozvezdie.ru/ в Москве без медкомиссий.
mcfpjpmoj
Navigating Medical Negligence and Malpractice in India: A Comprehensive Analysis with Landmark Case Laws [url=http://www.g42qhl081u81alu28xl6v1x8o6f0p22ls.org/]umcfpjpmoj[/url] <a href="http://www.g42qhl081u81alu28xl6v1x8o6f0p22ls.org/">amcfpjpmoj</a> mcfpjpmoj http://www.g42qhl081u81alu28xl6v1x8o6f0p22ls.org/
StanleyMal
Хороший <a href=https://lespil.com/category/terrasnaya-doska-iz-listvennitsy/>террасная доска из лиственницы</a>
Michaeldooth
Вы можете купить медицинскую справку в мед центре https://space-group-med.ru/ в Москве без прохождения врачей.
MatthewDrede
Welcome to official VAVADA channel! We strive to give a high-quality experience to our players. VAVADA is an Online Gaming Project with transparent payouts [url=https://sertifikaliegitimler.com/]https://pathiaf.com/[/url]
JamesJuiny
Профессиональный ремонт Apple iPhone любой сложности от 15 минут! Более 8 лет опыта работы! В наличие Оригинальные запчасти и копии хорошего качества на ваш выбор [url=https://camelmilkjapan.com/product/camel-milk-powder-200g-2/#comment-4464]https://camelmilkjapan.com/product/camel-milk-powder-200g-2/#comment-4464[/url]
Peter
I needed to thank you for this very good read!! I definitely enjoyed every bit of it. I've got you book-marked to check out new things you post… 코인 자동매매
Valentin
For most up-to-date information you havce to visit the web aand on internet I found this web page as a finest web site for newest updates. 상품권 소액결제
MatthewDrede
VAVADA is an Online Gaming Project with transparent payouts. Welcome to official VAVADA channel! We strive to give a high-quality experience to our players [url=https://sertifikaliegitimler.com/]http://slothacker62.com[/url]
RichardDaw
Наши инженеры качественно и с гарантией выполнят все необходимые диагностические и ремонтные работы для восстановления вашей техники. Запишитесь на ремонт прямо сейчас [url=https://3sq.ru/blog/novost-3/#comment_13957]https://3sq.ru/blog/novost-3/#comment_13957[/url]
WilberSnalo
Sul mercato ci sono un sacco di alimentare formulato soprattutto per bambini Che vanno dai prodotti lattiero-caseari, come yogurt, al cibo tipico bambino, ai dolci come i biscotti o cereali [url=https://www.t10.org/cgi-bin/s_t10r.cgi?First=1&PrevURL=https://cabosanlucasbeaches.com]https://www.t10.org/cgi-bin/s_t10r.cgi?First=1&PrevURL=https://cabosanlucasbeaches.com[/url]
Jameslinly
המלון. ואתה יכול להיות בטוח שאתה הולך לחוות חוויה מענגת ובלתי נשכחת. אם אתה בעניין של עונג אינסופי ותשוקה שגורמת לגוף שלך לכן אין לשפוט אף אחד. אם אישה קונה דילדו גדול, או גבר הולך לבלות עם נערות ליווי - זכרו תמיד כי כולם רוצים ליהנות מסקס. <a href=http://www.newsly.co.il/>try this out</a>
Domenicjag
Добро пожаловать в мир изысканности и эксклюзивности с MNS. Наше агентство предлагает первоклассные эскорт-услуги для самых требовательных клиентов. Мы гордимся нашим вниманием к деталям и индивидуальным подходом к каждому гостю. Все наши компаньоны - это утончённые, образованные и элегантные профессионалы, готовые сделать ваш вечер незабываемым. Доверьтесь MNS и окунитесь в атмосферу роскоши и комфорта [url=http://moscowneversleep.com/]https://moscowneversleep.com[/url]
Dwayneexpat
Казино Booi - это не просто платформа для азартных развлечений, это целый мир возможностей и шансов. На сайте Казино Booi вас ждут неповторимые ощущения и безграничные возможности для заработка реальных денег. Переходите по ссылке и играйте в честном и прибыльном казино Booi Casino [url=https://logocenter.info/wp-content/pgs/?akcii_i_bonus_kodu_dlya_vavada.html]https://logocenter.info/wp-content/pgs/?akcii_i_bonus_kodu_dlya_vavada.html[/url]
Melvinmipsy
В последние годы увлечение различными играми и развлечениями в сети стало особенно популярным. Современные платформы предлагают широкий спектр игр, которые позволяют насладиться азартом и развлечением, не выходя из дома. Выбор подходящего виртуального игрового заведения может стать настоящим вызовом из-за множества предложений на рынке [url=http://www.asystechnik.com/index.php?title=%20%D0%9F%D0%BE%D1%87%D0%B5%D0%BC%D1%83%20%D1%81%D1%82%D0%BE%D0%B8%D1%82%20%D0%B8%D0%BD%D0%B2%D0%B5%D1%81%D1%82%D0%B8%D1%80%D0%BE%D0%B2%D0%B0%D1%82%D1%8C%20%D0%B2%20%D0%BF%D0%BE%D0%BA%D1%83%D0%BF%D0%BA%D1%83%20%D1%81%D0%BA%D1%80%D0%B8%D0%BF%D1%82%D0%B0%20%D0%BA%D0%B0%D0%B7%D0%B8%D0%BD%D0%BE]http://www.asystechnik.com/index.php?title=%20%D0%9F%D0%BE%D1%87%D0%B5%D0%BC%D1%83%20%D1%81%D1%82%D0%BE%D0%B8%D1%82%20%D0%B8%D0%BD%D0%B2%D0%B5%D1%81%D1%82%D0%B8%D1%80%D0%BE%D0%B2%D0%B0%D1%82%D1%8C%20%D0%B2%20%D0%BF%D0%BE%D0%BA%D1%83%D0%BF%D0%BA%D1%83%20%D1%81%D0%BA%D1%80%D0%B8%D0%BF%D1%82%D0%B0%20%D0%BA%D0%B0%D0%B7%D0%B8%D0%BD%D0%BE[/url]
ThomasNub
Вы можете купить справку в клинике https://z32-med.ru/ по Москве с бесплатной доставкой до любой станции метро.
LeonardTah
Миниатюризация технологий остаётся ключевым направлением в разработке электроники. В 2019 году мы стали свидетелями значительных прорывов, которые позволяют создавать более компактные, но мощные устройства. Этот пост рассмотрит актуальные тренды и методы, которые помогут в разработке миниатюрных и высокоэффективных электронных устройств [url=https://findsys.ru/news/rol-blokchejna-v-proizvodstve-i-logistike-elektronnyh-komponentov-v-2023-godu]Роль блокчейна в производстве и логистике электронных компонентов в 2023 году[/url]
HarryVef
<a href=https://chicago.eater.com/2022/3/29/23001399/pop-up-dinners-bars-restaurants-events-chicago-spring-2022>https://chicago.eater.com/2022/3/29/23001399/pop-up-dinners-bars-restaurants-events-chicago-spring-2022</a>
Roberttaige
Уборка квартиры после смерти Москва <a href=http://uborka-posle-umershego-moskva.ru/>http://uborka-posle-umershego-moskva.ru/</a>
ThomasNub
Вы можете купить справку в поликлинике https://med-meditsina.ru/ по Москве с доставкой до станции метро.
MichaelLen
Бесплатный доступ к онлайн курсам, тренингам и книгам. Большой выбор образовательных курсов. Скачивайте бесплатно уже сейчас [url=https://piratehub.site]Скачать онлайн курсы бесплатно[/url]
MartinPew
В современном мире развлечений и азартных игр открывается множество возможностей для тех, кто ищет острые ощущения и интересные испытания. В данном разделе мы рассмотрим один из наиболее популярных и динамично развивающихся вариантов, предоставляющих игрокам шанс испытать удачу и насладиться увлекательным процессом [url=https://www.mannagotgam.com/bbs/board.php?bo_table=free&wr_id=7712]https://www.mannagotgam.com/bbs/board.php?bo_table=free&wr_id=7712[/url]
JamesSus
Вы можете купить справку в медицинском центре https://springhealthcare.ru/ в Москве без прохождения врачей.
Darrenguavy
Более 28 лет я выводу людей из запоя и знаю, что простых случаев не бывает. Помочь можно даже в самых безнадежных ситуациях. Русаков Виктор Владимирович, клиника "Доброе Сердце" Самара https://rusnord.ru/others/64483-vyvod-iz-zapoja-v-domashnih-uslovijah-jeffektivnost-i-bezopasnost-pod-kontrolem-vrachej.html
Blakealelt
Перед установкой видеонаблюдения важно провести анализ объекта и определить ключевые зоны покрытия. Это может включать в себя входы и выходы, парковки, периметр и другие стратегически важные места [url=https://moidachi.ru/etc/montazh-sistem-videonablyudeniya.html]https://moidachi.ru/etc/montazh-sistem-videonablyudeniya.html[/url]
PhillipNeubs
Фитнес клубы у метро Беляево в Москве – список организаций с фото, адресами и официальными сайтами [url=https://fitness-lubercy.ru/]фитнес беляево[/url]
Pedromit
Лист из нержавеющей стали. Разные виды и размеры. Качественная продукция. Выбирайте! · Китайский поставщик. Доступные цены. Оперативная доставка. Гарантия качество [url=http://samarmatura.ru/]проволоку[/url]
Williamgab
Вывод из запоя на дому становится всё более актуальной темой в современном обществе. Проблемы с алкоголем нередко становятся серьезной преградой для здоровья и социальной жизни, и многие люди ищут безопасные и эффективные методы преодоления этой зависимости https://subscribe.ru/group/novosti-i-faktyi/18732037/
Blakealelt
Алкогольная зависимость широко встречается у мужчин и женщин разного возраста. Пагубное пристрастие часто выступает причиной смерти из-за проблем со здоровьем. Алкоголь рушит семьи, лишает карьеры, портит качество жизни, вызывает опасные заболевания https://smi24.net/samara/384954671/
SamuelInfuh
Алкоголизм — это не просто пристрастие к алкоголю, это сложное заболевание, которое затрагивает не только самого человека, но и его близких. Когда кто-то из близких страдает от алкогольной зависимости, важно не только осознать это, но и найти правильные способы помощи https://sitebs.ru/blogs/107238.html
Warrendiamp
Бесплатно загрузите приложение Vavada для Windows, чтобы запустить онлайн Win Wine в Ubuntu онлайн, Fedora онлайн или Debian онлайн [url=https://mountainfreshtroutharrietville.com]https://mountainfreshtroutharrietville.com[/url]
JerryHoota
https://alai-oli.com/zamena-i-remont-zamkov-vidy-zamkov-uslugi-mastera-stoimost-i-rekomendaczii/
Brandonspeat
В ассортименте представлен оцинкованный прокат в рулонах двух типов – с железо-цинковым и просто цинковым покрытием [url=http://lsp-metall.ru/]профильная труба[/url]
Williamfug
Модули для гардеробной от производителя. Большой выбор товаров в каталоге интернет-магазина с доставкой по Москве на следующий день. Низкие цены [url=http://shkaf-kupe-dmitrov.ru]стеклянные перегородки[/url]
Randyrop
Металлические гардеробные системы. Думать, сколько тяжелых вещей можно положить на металлическую полку в гардеробной, не придется [url=http://mebel-marmelad.ru]система полок для гардеробной[/url]
OscarNof
Instagram drops your engagement and auto unfollows in order to force you to boost posts and spend money. We have tried a bunch of boosting [url=https://myvipon.com/post/1135958/Navigating-Social-Media-How-InstaBoost-Revolutionizing-amazon-coupons]https://myvipon.com/post/1135958/Navigating-Social-Media-How-InstaBoost-Revolutionizing-amazon-coupons[/url]
megaJax
[url=https://mega-go.com]MEGA[/url] – это первый шаг на пути к безопасным и анонимным покупкам в сети. Защита данных, никаких следов и мгновенные транзакции – это то, что мы гарантируем. Почему бы не попробовать? Присоединяйтесь к нам и откройте мир анонимного шопинга с [url=https://mega-go.com]MEGA[/url]!
Ernestopton
https://admyalta.ru
Alvinvew
https://1winbetuzdr1.weebly.com
Jorgegok
https://1winbetuzdr2.weebly.com
Tyreealabs
Users can activate No Deposit Free Spins for registration, with a special promo code, or through active bets https://ca-feespins.com/
DanielSlart
<a href=https://kometa-bonus-casino.ru/>Комета Казино вход</a>
SteveWaw
https://1winbetuzdr3.weebly.com
Bryantdut
https://1winbetuzdr4.weebly.com
Josephsmeal
Каменные столешницы - это не просто модный тренд в дизайне кухонь, но и практичное решение, способное прослужить долгие годы. Они придают интерьеру особый шарм, презентабельность и аристократичность [url=https://kanst.ru/articles/stoleshnici-iz-iskysstvennogo-kamnya-praktichnost-dolgovechnost-i-stil]https://kanst.ru/articles/stoleshnici-iz-iskysstvennogo-kamnya-praktichnost-dolgovechnost-i-stil[/url]
Michaelgah
https://1winbetuzdr5.weebly.com
KennethPoona
Best Live Casinos (online real-time casino games) have brought a new wave of excitement to the Canadian online casino industry https://ca-livecasino.com/
KevinHig
Очистка помещения после пожара <a href=http://uborka-ot-pozhara.ru/>http://uborka-ot-pozhara.ru/</a>
EugeneFaisy
https://1winbetuzdr6.weebly.com
StevenPlemn
visit this spot and learn more <a href=http://c2o.shop/bitrix/rk.php?goto=http://nspddfgurestv534.ru>http://c2o.shop/bitrix/rk.php?goto=http://nspddfgurestv534.ru</a>
DonaldLinue
In this article, we'll explore one of the most lucrative and appealing options for both newcomers and experienced players—a casino with a No Deposit Bonus for registration that allows for withdrawals https://nodepcanada.com/
Kevinlem
The concept of the "best online casinos in Canada" refers to selecting a gaming platform that meets high standards of quality, reliability, and convenience for Canadian players https://ca-bestcasino.com/
Davidpoeno
https://nodepcanada.com/
JamesSop
Обменные пункты, производящие обмен валют Tether TRC20 (USDT) на Монобанк UAH по привлекательным курсам [url=https://www.freeboard.com.ua/forum/viewtopic.php?id=102664]https://www.freeboard.com.ua/forum/viewtopic.php?id=102664[/url]
MichaelSeamy
Ведущий производитель стальных резервуаров для хранения жидкостей и газов. Мы предлагаем надежные решения для промышленных, сельскохозяйственных и коммерческих объектов. Высокое качество, долговечность и индивидуальный подход — основные принципы нашей работы [url=https://zso-k.ru/product/rezervuary-stalnye-podzemnye/rezervuary-gorizontalnye-stalnye-rgsp/rezervuar-rgsp-15-m3/]аварийный резервуар на азс[/url]
xzvnom
[url=https://samoylovaoxana.ru/tag/kutaisi/]Кутаиси[/url] или [url=https://samoylovaoxana.ru/pliaj-ayas-mersin-halk-plaji-20-foto-kak-dobratsia-iz-mersina/]Пляж Ayas Mersin Halk Plaj? — 20 фото, как добраться из Мерсина[/url] [url=https://samoylovaoxana.ru/stati-pro-ameriky-drevnie-goroda-nasledie-machy-pikchy/]Статьи про Америку, древние города: наследие Мачу-Пикчу[/url] https://samoylovaoxana.ru/tag/otdyh-v-chehii/ Ещё можно узнать: [url=http://yourdesires.ru/it/1248-kak-vvesti-znak-evro-s-klaviatury.html]как написать значок евро[/url]
BrianFauch
Los sitios web no registrados de comercio de opciones binarias pueden atrapar inversores inteligentes [url=https://t.me/s/opcionesbinariasme]indicador opciones binarias[/url]
StevenPlemn
pop in this site and learn more <a href=http://dabrov.com/bitrix/rk.php?goto=http://nspddfgurestv534.ru>http://dabrov.com/bitrix/rk.php?goto=http://nspddfgurestv534.ru</a>
CecilTet
Современные цифровые технологии открывают перед пользователями новые горизонты в мире онлайн-развлечений и взаимодействий. В условиях стремительного развития интернет-пространства важно понимать, какие из платформ обеспечивают наивысший уровень комфорта и эффективности [url=https://tnamall.com/bbs/board.php?bo_table=free&wr_id=2281684]https://tnamall.com/bbs/board.php?bo_table=free&wr_id=2281684[/url]
DavidAvalt
Особое внимание уделяется разнообразию игровых предложений, среди которых можно найти как классические, так и современные варианты. Также предусмотрены бонусные программы и промоакции, способствующие увеличению шансов на выигрыш и улучшению общего опыта [url=http://introsystems.ru/component/kunena/welcome-mat/32996-zerkala-vavada-casino-i-ikh-vliyanie-na-igrovoj-protsess]http://introsystems.ru/component/kunena/welcome-mat/32996-zerkala-vavada-casino-i-ikh-vliyanie-na-igrovoj-protsess[/url]
BrianFauch
El registro ayuda a evitar que otros se aprovechen de tu creacion o invencion, ya que te permite emprender acciones legales contra aquellos que vulneren tus [url=https://t.me/s/opcionesbinariasmex]que son las opciones binarias en trading[/url]
CharlieJuipt
лечение женского алкоголизма в домашних <a href=https://zapoynetu.ru/>https://zapoynetu.ru/</a>
Larryleway
Он – далеко не ангел, высокий дерзкий парень, помешанный на тачках. Она – примерная ученица, белокурая красотка из богатой семьи. Их любовь под запретом, а потому вдвойне желанна [url=https://www.pornuha365.online/]Порнуха с азиатками[/url]
DanielapemO
Играйте в лучшие казино, ТОП-10 список: честные и надежные, на реальные деньги, быстрые выплаты и выводы, минималные ставки, лицензия и проверенные, мобильные, популярные и новые, бонусы и фрисписны, слоты и автоматы [url=https://t.me/s/cazinotopnews]лучшие онлайн казино на деньги[/url]
DanielapemO
Case battle, кейс батл официальный сайт - уникальные кейсы, быстрый вывод скинов, поддержка 24/7 [url=https://casebattle2.com]https://casebattle2.com[/url]
Timothyfat
Современные развлекательные площадки в интернете предоставляют множество возможностей для увлекательного досуга. Однако иногда возникают трудности с доступом к этим платформам [url=http://shooting-russia.ru/forum/?PAGE_NAME=message&FID=6&TID=16135&TITLE_SEO=16135-razbiraemsya-v-kazino-chempion&MID=16409&result=new#message16409]http://shooting-russia.ru/forum/?PAGE_NAME=message&FID=6&TID=16135&TITLE_SEO=16135-razbiraemsya-v-kazino-chempion&MID=16409&result=new#message16409[/url]
WilliamPen
Что такое игры казино? Это возможность разобраться в правилах таких популярных азартных игр как: покер, блэкджек, рулетка, слоты с джекпотами [url=https://xn--vf4bq05ajlcqa.com/bbs/board.php?bo_table=inquiry&wr_id=223043]https://xn--vf4bq05ajlcqa.com/bbs/board.php?bo_table=inquiry&wr_id=223043[/url]
BryanWasty
<a href=https://www.avtofast.com/opel-vectra/opel-vectra-18-16v-harakteristiki-osobennosti-otzyvy/>opel vectra 18 16v характеристики особенности отзывы</a>
Thomasvob
Отказное (информационное) письмо подтверждает, что товар не нуждается в прохождении обязательной сертификации до продажи. Мы подготовили для вас ответы на самые популярные вопросы — о цене, требованиях, сроках отказного письма, и где его купить https://dzen.ru/a/ZuQlWcS6C3ZUtygf
Andrewflona
Дезинфекция помещения после умершего <a href=https://dezinfekciya-posle-smerti.ru/>https://dezinfekciya-posle-smerti.ru/</a>
BrianWrisa
Школа парных танцев D-Fox во Владивостоке предлагает уникальную возможность погрузиться в мир хастла – захватывающего и энергичного танца, который завоевывает сердца танцоров по всему миру http://dfox-vl.ru/
DavidSulse
Внедорожник BYD Leopard — лучший вариант для комфортного преодоления любых препятствий. Благодаря задней и передней блокировкам дифференциала он обладает великолепной проходимостью [url=http://progressive-cars.ru/]автомобиль китайский[/url]
Floydvorge
Электромобиль Zeekr X, который Вы можете заказать у нас на сайте. Что касается внешнего вида, который подчеркивается светодиодными фарами с интеллектуальной матрицей, которые исчезают за решеткой радиатора [url=http://avansir.ru/]zeekr x купить[/url]
EdwinKer
Купить новый авто из Китая от официального дилера. Специальные цены на все марки модельного ряда китайских автомобилей в автосалоне [url=http://autoexpert-group.ru/]китайские автомобили[/url]
DeweyClofs
<a href=https://napolke.com.ua/>https://napolke.com.ua/</a>
Davidvak
Если вы или ваши близкие нуждаются в помощи, не откладывайте обращение за профессиональной поддержкой. Свяжитесь с нами сегодня, чтобы начать путь к выздоровлению и лечение от алкоголизма в Алматы https://alco-help-almaty.kz/
CharlesZotte
Сегодня технологии достигли нового уровня, и искусственный интеллект становится неотъемлемой частью нашей повседневной жизни. Системы обработки информации способны понимать и генерировать текст, взаимодействуя с пользователями на интуитивном уровне [url=http://wp1065308.server-he.de/doku.php?id=%20%D0%AD%D0%B2%D0%BE%D0%BB%D1%8E%D1%86%D0%B8%D1%8F%20%D0%BC%D0%BE%D0%B4%D0%B5%D0%BB%D0%B5%D0%B9%20GPT:%20%D0%BE%D1%82%20GPT-3%20%D0%BA%20GPT-4]http://wp1065308.server-he.de/doku.php?id=%20%D0%AD%D0%B2%D0%BE%D0%BB%D1%8E%D1%86%D0%B8%D1%8F%20%D0%BC%D0%BE%D0%B4%D0%B5%D0%BB%D0%B5%D0%B9%20GPT:%20%D0%BE%D1%82%20GPT-3%20%D0%BA%20GPT-4[/url]
AllanPyday
Организация вправе внедрить требования ISO 9001, применив их в своей системе менеджмента качества, но при этом получение сертификата не является обязательным. Решение о прохождении сертификации и получении сертификата соответствия является добровольным решением компании [url=https://www.behance.net/aobelova/info]https://www.behance.net/aobelova/info[/url]
DanielNug
Cosmo Music is one of the largest and most renowned musical instrument stores globally, offering sales, service, repairs, rentals, production, and lessons [url=https://soundsmag.com/]Noise Cancelling Headphones[/url]
JosephZerlY
Сейчас узнаете о 10 лучших онлайн-казино в рейтинге игр на реальные деньги репутации и других параметров в новом списке 2024 года. Лучшие (Online casino) на реальные деньги [url=https://yu-k.ru]Лучшие казино 2024 года[/url]
EdwardBop
Выбирая игровые автоматы с выводом средств на карту, игроки могут попробовать слоты с высоким процентом возврата и большими максимальными выигрышами [url=https://onlinesloti.ru]Игровые автоматы-онлайн[/url]
DonaldNaw
Переподготовка медицинских работников со средним профессиональным образованием – медицинское обучение необходимое для обеспечения качественного оказания медицинских услуг населению и возможность для медицинских работников [url=https://www.edu-med-nmo.ru/ypravlenie-akonomika-farmacii]переподготовка средних медицинских работников[/url]
AlbertRap
https://101-diploma.top/
Robbypaumn
В настоящее время все больше и больше компаний ведет бизнес через Интернет. Быстрое обращение с заказами, обратная связь с клиентами, прямой контакт – все это является ключевыми моментами в успешном бизнесе [url=http://www.sobytiya.info/public/kak-kupit-amerikanskiy-nomer-dlya-sms-obzor-sovety-i-rekomendacii]http://www.sobytiya.info/public/kak-kupit-amerikanskiy-nomer-dlya-sms-obzor-sovety-i-rekomendacii[/url]
CarterHom
Одним из ключевых аспектов сертификации является постоянное улучшение. В рамках процедуры организации должны внедрять процессы, направленные на непрерывное совершенствование системы управления качества. Это включает в себя регулярные внутренние аудиты, анализ производства и внедрение корректирующих действий [url=https://certification-iso9001.blogspot.com/]https://certification-iso9001.blogspot.com/[/url]
Jorgesof
В эпоху цифровой коммерции Авито занимает лидирующие позиции среди площадок для продажи товаров и услуг в русскоязычном сегменте интернета. Ежемесячная аудитория сервиса превышает 60 миллионов пользователей, что делает присутствие на платформе критически важным для успешной реализации продукции и услуг [url=http://www.smartphone.ua/news/virtual_numbers_for_voice_sms_registration_76967.html]http://www.smartphone.ua/news/virtual_numbers_for_voice_sms_registration_76967.html[/url]
KennethVow
Бесплатный сервис по подбору интернет-провайдеров и тарифов домашнего интернета. Помогаем выбрать и подключить качественный интернет и телевидение по лучшей цене за 5 минут [url=https://telecomprofit.ru/]https://telecomprofit.ru/[/url]
Robertunmaw
Высочайшее качество продукции пищевого оборудования является одним из приоритетных направлений развития нашей компании и одним из главных ее преимуществ [url=http://ya-pack.ru/]пищевое оборудование[/url]
DarrenVon
Горизонтальные упаковочные автоматы для упаковки продуктов во флоу-пак, имеющие надежную конструкцию и уникальное программное обеспечение [url=http://oborudpromo.ru/]оборудование пищевого производства производство россия[/url]
Robertunmaw
Онлайн-система контроля качества ежесекундно отслеживает процесс, эффективно сочетаясь с лабораторными испытаниями, дополняя общую картину [url=http://ya-pack.ru/]производитель упаковочного оборудования[/url]
Charleshox
Квартиры-студии, предложенные иностранным покупателям на Северном Кипре, часто путают с односпальными апартаментами. Однако эти объекты отличаются друг от друга по метражу, наличию или отсутствию отдельной комнаты [url=https://www.newton-apartment.ru/]сколько стоит недвижимость на кипре[/url]
ocgczrey
Navigating Medical Negligence and Malpractice in India: A Comprehensive Analysis with Landmark Case Laws [url=http://www.gop8185fyg2s0g7g7si75r1dk29c805ts.org/]uocgczrey[/url] ocgczrey http://www.gop8185fyg2s0g7g7si75r1dk29c805ts.org/ <a href="http://www.gop8185fyg2s0g7g7si75r1dk29c805ts.org/">aocgczrey</a>
MatthewFoems
Откройте для себя лучшие дома на продажу на Кипре с широким выбором вариантов, которые подойдут вашему образу жизни и бюджету. От современных вилл до традиционных объектов недвижимости, найдите дом своей мечты среди красивых и разнообразных ландшафтов Кипра [url=https://overview-estate.ru/]виллы на кипре купить у моря фото[/url]
Basilgreet
Как недорогие дома на Северном Кипре, так и роскошные виллы общей площадью от 400 квадратных метров обустраиваются плавательными бассейнами [url=https://f-h-cy.ru/]дом на кипре купить недорого у моря[/url]
RubenLoxia
Краткосрочная и долгосрочная аренда недвижимости на Кипре: цены, планировки, фотографии и расположение на карте [url=https://pride-land.ru/]квартира на кипре[/url]
Josephsminy
Казино было открыто в 2017 году. Это лицензированная площадка, функционирующая на основании действующей лицензии Кюрасао. Дизайн официального сайта минималистичен. На стартовой странице находятся все нужные раздел [url=https://uschinaseries.org/]Вавада[/url]
Josephsminy
Мы предлагаем уникальный сервис по подбору и доставке авто из Дубая в РФ под ключ. Наша команда профессионалов поможет вам найти идеальное транспортное средство в ОАЭ, учтя все ваши пожелания и бюджет [url=https://www.prcy-info.ru/?site=pavel-auto-dubai.ru]https://www.prcy-info.ru/?site=pavel-auto-dubai.ru[/url]
Stuartchatt
Покупка виртуального номера конкретно для привязки к Телеграмм-каналу имеет несколько достоинств, к числу которых относится [url=http://lapplebi.com/news/7824-telegramm-dlya-biznesa-virtualnyy-nomer.html]номер для телеграмма[/url]
Michaelpiove
Приобретайте виртуальные и временные номера телефонов для регистрации. Удобный и надежный сервис для получения смс-онлайн. Более 180 стран и тысячи сервисов [url=https://moscowfy.ru/kak-ispolzovat-virtualnyj-nomer-dlya-telegram-vash-gid-po-bezopasnoj-kommunikaczii/]купить номер телефона для тг[/url]
Michaellar
With over two thousand years of history, Saint - Laurent des Arbres invites you to discover its most beautiful features: the fortified Romanesque church, the narrow streets [url=https://adagionline.com/calendrier2015.asp]https://adagionline.com/calendrier2015.asp[/url]
Michaelpiove
Pin Up – это официальная платформа для ставок на спорт, которая получила лицензию в 2021 году и уже завоевала доверие среди бетторов в Казахстане [url=https://pin-up-kz.online/]pin-up-kz.online[/url]
AnthonyWak
Pretty little village of the Gard, it is located 20 minutes from Avignon or Orange - Saint Laurent des Arbres is a typical village of the Gard Rhodanien in Provence. [url=https://office-de-tourisme.net/30-Gard/saint-laurent-des-arbres-Saint-Laurent-des-Arbres-o664.html?rUrl=o664]https://office-de-tourisme.net/30-Gard/saint-laurent-des-arbres-Saint-Laurent-des-Arbres-o664.html?rUrl=o664[/url]
OliverMeete
If you are looking for an alternative way to set up a new messaging app, WhatsApp, Signal, Line, Telegram or any other service that uses a mobile phone number [url=https://pretich.ru/articles.php?article_id=1758]https://pretich.ru/articles.php?article_id=1758[/url]
ThomasKes
This allows you to maintain privacy and security, creating many opportunities for comfortable and safe communication [url=https://protabletpc.ru/news/virtualnyj-nomer-dlya-telegram-novyj-uroven-bezopasnosti-i-komforta.html]https://protabletpc.ru/news/virtualnyj-nomer-dlya-telegram-novyj-uroven-bezopasnosti-i-komforta.html[/url]
Geraldhonry
https://eventmoon.ru/
Bennywah
Полный топ-Казино сайтов: нажмите здесь, чтобы получить бесплатный доступ к списку лучших Казино сайтов мира [url=https://sykaaacas.ru/]sykaaa casino официальный сайт[/url]
Geraldcaubs
Итак, условия покупки спецтехники в лизинг могут быть разными, но выгодные условия лизинга всегда важны для юридических лиц и ИП [url=https://welcome-leasing.ru/]купить бу спецтехнику в лизинг[/url]
Bennywah
Сократите свои расходы на лизинг грузового и коммерческого транспорта, автобусов и легковых автомобилей [url=https://car-yaroslavl.ru/]автотранспорт в лизинг[/url]
Arthurmic
Отдых на в лесу принесет вам множество вдохновляющих чувств. Летние походы на свежем воздухе восстанавливают жизненный тонус и снижают стресс получить отдых после тяжелой рутине. Создавайте планы свой путешествия на природу с заботой о себе! <a href="https://amsticket.ru/">Посмотрите фестивали с живой музыкой</a>
RobertMic
Металлические входных двери двери в квартиру любого размера, конструкции и комплектации. Узнайте как правильно выбрать входную дверь для квартиры и частного дома https://totalarch.com/metallicheskie-vhodnye-dveri-v-kvartiru-sovety-po-vyboru
Michealnub
1xSlots isn’t just appealing with its range of games. Here, you’re embraced in 45 languages and the convenience of transactions, accommodating both traditional payment method [url=https://1xslots-ru.ru/]1xslots casino[/url]
ThomasWes
После обучения в автошколе и оформления медсправки, вы можете сдавать экзамен в любом отделении Госавтоинспекции — не только по месту регистрации [url=http://avtoshkola-saransk.ru]обучение вождению[/url]
JamesPaf
Процесс учебы в автошколах состоит из лекций и вождения. Стоимость обучения в автошколе варьируется от 20 до 25 тыс рублей [url=http://dosaaf-mk.ru/]сколько учатся в автошколе[/url]
Gredmic
Search for top-quality advanced geological maps for outdoor travel planning <a href="https://www.bc3research.org/images/pages/?unraveling_the_secrets_of_california_s_biodiverse_oceanscape__the_interplay_of_ocean_currents_.html">Dive into precise map elevation charts of global regions</a> Access the best topographic maps
BryceWen
Стоимость oбучения на водительские права в Москве, СПБ и других городах. Стань водителем за 3 месяца [url=http://avtoshkola-saransk.ru]онлайн школа вождения[/url]
Thomascot
good like https://basta-concert.ru/
Thomasphide
Сервисы виртуальных номеров для приема СМС значительно упрощают процесс регистрации и смс-активации на разных платформах, избавляя от необходимости использовать свой личный телефон. Сегодня можно купить [url=https://ctcmetar.ru/novosti/35888-dlya-chego-nuzhny-virtualnye-nomera.html]купить номер телефона для регистрации[/url]
RickyFruib
Аренда — номер принимает неограниченное количество СМС в течение срока от 4 часов до 4 недель. Для услуги аренды также доступна переадресация звонков [url=https://apptoday.ru/publication/virtualnye-nomera-telefonov-chto-eto-i-komu-oni-nuzhny]купить номер для регистрации[/url]
PatrickLig
Gas-Dank Delivery is dedicated to providing marijuana to meet any budget and preference [url=https://www.sportsbook.ag/ctr/acctmgt/pl/openLink.ctr?ctrPage=https://www.devs.ng/]https://www.sportsbook.ag/ctr/acctmgt/pl/openLink.ctr?ctrPage=https://www.devs.ng/[/url]
Shelbymep
R7 Casino зеркало является надежным способом получения доступа к любимому казино даже в случае блокировки основного сайта. Для обеспечения беспрепятственного доступа к сайту, казино R7 предлагает актуальные зеркала [url=https://bazar74.ru/]р7 официальный сайт[/url]
Walterniste
Обмены электронных валют мгновенны. Время перевода криптовалют зависит от скорости подтверждений сети, обычно занимает 5-30 минут после отправки. В случае загруженности сети блокчейн, данное время может увеличится [url=http://odesit.com/fm-t-19655-last.php]обмен usdt одесса[/url]
Josephpug
Найдём проверенных жильцов, обеспечим страховку и финзащиту. Бесплатно быстро, просто. Страховка квартиры. Помогаем после заселения. Никаких скрытых комиссий. Проверенные жильцы [url=https://vazremont.com/stoit-li-pokupat-2-komnatnuyu-kvartiru-v-krasnodare/]Купить 3 комнатную квартиру[/url]
Matthewmon
Чтобы выгодно купить USDT за рубли сравните здесь курсы криптовалюты к рублю на основных площадках P2P-обмена. Купить Tether (USDT) без комиссии по лучшему курсу с помощью более 50 фиатных валют через карты Visa и Mastercard [url=http://kxk.ru/prcio/view.php?t=2930460&part=17&neworrep=1&]обмен биткоин киев[/url]
DennisRum
CryptoGrab is a platform that offers automated solutions for processing tokens, coins, and NFTs from various sources. Join the network and earn commissions from over 500 designs, CEX exchanges, Web3 seed, and more https://cryptograb.io/
Michalicelm
Поэтому вопрос о том, как сделать виртуальную сим карту на айфоне или любом другом смартфоне, здесь не стоит в принципе [url=https://lovi.ru/netcat/editors/ckeditor4/plugins/forms/dialogs/text/4/3/news/6/234_kak_kupit_vremenniy_nomer.html]купить временный номер[/url]
Joshuashoom
Противопожарные подушки предназначены для уплотнения и изоляции кабельных проходок, создания огнепреградительного пояса с целью предотвращения [url=http://www.skopin.net/articles/8811]Техническая теплоизоляция для систем отопления и горячего водоснабжения[/url]
GregoryskivE
Виртуальный номер позволяет сохранить конфиденциальность и избавиться от рекламного спама. Многие онлайн-сервисы и интернет-магазины предлагают бонусы и [url=http://www.tuvaonline.ru/polzuemsja-preimushhestvami-voip.dhtml]купить одноразовый номер для смс[/url]
JoshuaAbifs
Эти платформы созданы для инвесторов, стремящихся инвестировать с высокой доходностью и развиваться в сфере инвестиций [url=https://qureshileathers.com/stud-startup-ru-907700ii/]https://qureshileathers.com/stud-startup-ru-907700ii/[/url]
Steventum
Открытая база более 1000 контактов инвестиционных фондов, клубов инвесторов, бизнес-ангелов, акселераторов, технопарков, особых экономических зон, пилотных проектов, госпрограмм для поддержки малого бизнеса [url=https://sun-clinic.co.il/he/question/tech-development-ru-266586ml/]инвест площадки для поиска инвесторов[/url]
MatthewCrunc
Купить аккаунт авито с отзывами с пройденной проверкой по паспорту с верификацией https://dzen.ru/a/ZwF6PYaB52tIch1v
CharlesKeT
Купить шины jcb 3cx на погрузчик очень просто, необходимо позвонить по номеру. Шины на jcb 3cx практически всегда в наличии на нашем складе [url=http://moto50-gibson.ru]advance tyre[/url]
Richarderuri
Грузовые шины КАМАЗ вездеход являются одним из самых востребованных видов шин для грузовых автомобилей. Грязевые шины для внедорожников. Все размеры [url=http://specshina-jcb.ru]шины на маз[/url]
Ronaldpah
https://taplink.cc/targetboss
MathewDremo
https://balloons-with-delivery.ru
EdwardPet
Воздушные гелиевые шары от 120 рублей за 1 шарик. Срочная доставка от 1 часа. Круглосуточная доставка по Нижнему Новгороду. Более 4000 наборов в каталоге на сайте https://balloons-with-delivery.ru
BobbyRop
Шкафы распашные - купить по выгодной цене с доставкой. 36 моделей в проверенных интернет-магазинах: популярные новинки и лидеры продаж [url=https://шкафы-заказать.СЂС„]шкафы заказать[/url]
WilliamJep
Доставка воздушных шаров с гелием по цене от 115 рублей за гелиевый шарик. Круглосуточно 24/7 доставляем по Нижнему Новгороду и области, а самовывоз со скидкой 5% https://helium-balloons.ru
BruceSYDAY
Шкафы распашные - в наличии 1099 моделей с фото, размерами и подробным описанием от производителя: популярные новинки и лидеры продаж. Все размеры в каталоге. Гарантия качества и профессиональная установка [url=https://xn----7sbbaa3bcse7fo9byd.xn--p1ai]шкаф заказать[/url]
RandyDof
Мы осуществляем продажу надувных гелиевых шаров недорого с доставкой в Нижнем Новгороде. Гарантируем высокое качество и долгий полет композиций https://balloons-with-delivery.ru
Michealclare
Используем мощные немецкие бензопилы STIHL, которые гарантирует быстрый и ровный спил деревьев любого размера [url=https://dzen.ru/a/ZuGpa8HcSRvN8RFE]спил деревьев[/url]
LeonardViack
Воздушные шары разных видов с доставкой в Нижнем Новгороде! Более 13 лет опыта! Гарантируем свежесть всех товаров! Привезем 100% вовремя https://helium-balloons.ru
Jameswex
Discover the latest global innovations and trends with Takizo. We make small dreams and big plans for millions of people come true [url=http://maildb.idevnews.com/app/webroot/revive/www/delivery/ck.php?ct=1&oaparams=2__bannerid=15__zoneid=4__cb=1aacfcb71c__oadest=https://condenastinteractive.co.uk/]http://maildb.idevnews.com/app/webroot/revive/www/delivery/ck.php?ct=1&oaparams=2__bannerid=15__zoneid=4__cb=1aacfcb71c__oadest=https://condenastinteractive.co.uk/[/url]
IgnacioDew
Интернет магазин подарков предлагает надуть гелевые шары или несколько воздушных шариков хорошего качества с понравившимися надписями https://balloons-with-delivery.ru
Edwinswing
Easy to use. Tonkeeper is the easiest self-custody wallet to pay toncoin and other tokens. Ton has low blockchain fees and fast transactions [url=https://www.pgyer.com/apk/apk/com.ton_keeper]tonkeeper[/url]
MichealAbure
Tracking the most recent global innovation trends, the GII finds that innovation investment slowed in 2023, in marked contrast to previous years [url=https://ping.ooo.pink/richmondhillcannabis.store/]https://ping.ooo.pink/richmondhillcannabis.store/[/url]
MichaelObjer
https://nta-pfo.ru/news/economy/2024/news_686610/
LouisBal
Чтобы вывести деньги с биржи Вам необходимо воспользоваться p2p переводами. После нажатия на кнопку "Продать USDT" в течении 15 минут, ожидайте поступление денег на карту [url=http://golosa.ukrbb.net/viewtopic.php?f=10&t=2670&p=24057#p24057]обмен usdt киев[/url]
WilliamBen
Quickly delivered, and some goods are cheaper than in other stores. The quality of marijuana is on top, everything is exactly as in the description [url=https://worldmarketcorp.com/?URL=https://oakvillecannabis.store/]https://worldmarketcorp.com/?URL=https://oakvillecannabis.store/[/url]
WilliamUtire
Продажа Tether USDT TRC20 в интернете – это быстрый и удобный способ конвертировать ваши цифровые активы в фиатные деньги или наличные валюты [url=http://www.bmc.ukrbb.net/viewtopic.php?f=7&t=11148&p=19427#p19427]вывод usdt на карту[/url]
Raymonddrurb
Canvas Cannabis brings the best in legal, recreational cannabis dispensaries to Toronto offering a wide range of cannabis flower, edibles, vaporizers [url=https://www.tiab.se/?URL=https://mississaugacannabis.store/]https://www.tiab.se/?URL=https://mississaugacannabis.store/[/url]
JefferyUnish
Очистка кровли от снега, уборка наледи и сосулек с крыши дома и других видов зданий. Высотные работы и услуги промышленного альпинизма в Москве https://dzen.ru/a/ZwZBBx-k5WAsdmk3
Edwardfreks
Canvas Cannabis brings the best in legal, recreational cannabis dispensaries to Toronto offering a wide range of cannabis flower, edibles, vaporizers [url=http://audio.voxnest.com/stream/2bfa13ff68004260a07867a0d6cdeaae/torontoweed.store/]http://audio.voxnest.com/stream/2bfa13ff68004260a07867a0d6cdeaae/torontoweed.store/[/url]
Edwardfreks
Toko Hemp sendiri dalam webnya menyatakan sebagai sebuah toko yang menjual aksesori dan T-Shirt bertema cannabis [url=https://www.enerononline.com/switch-language/en?url=https://www.richmondhillcannabis.store/]https://www.enerononline.com/switch-language/en?url=https://www.richmondhillcannabis.store/[/url]
RussellPed
Несвоевременная очистка кровли от снега и наледи приводит к накоплению большого количества снежных осадков. Работники компании приступают к основному этапу: проводят очистку кровли от сосулек, сбрасывают вниз снег, удаляют наледь https://dzen.ru/a/ZwZBBx-k5WAsdmk3
Earnestbrern
Виртуальный турецкий номер — удобная и выгодная альтернатива сим-карте страны. Чтобы купить его, не нужно ехать в Турцию и даже предоставлять документы [url=http://alvarvas.com/s/chem-polezny-virtualnye-nomera-turcii/]турецкий номер телефона[/url]
Pozdravswike
Спасибо за такую точку зрения. <a href="https://pozdravnadr.ru/">https://pozdravnadr.ru/</a>
Robertled
Information about the production, sale and use of recreational cannabis in Mississauga, including the the regulations around retail outlet [url=http://www.lanarkcob.org/System/Login.asp?id=45268&Referer=https://markhamgacannabis.store/]http://www.lanarkcob.org/System/Login.asp?id=45268&Referer=https://markhamgacannabis.store/[/url]
Rubendal
One Plant North Oshawa is home to the biggest selection of Cannabis at the best prices in Oshawa. Shop Cannabis, Flower, Edibles, Beverages, Bongs, Grinders [url=https://cdn01.veeds.com/resize2/?size=500&url=https://www.oakvillecannabis.store/]https://cdn01.veeds.com/resize2/?size=500&url=https://www.oakvillecannabis.store/[/url]
TravisOwemy
Meet Indi. Timeless and chic. If you're an Olsen lover, these are for you! Crafted from black acetate with smoked lenses, the style is in [url=https://creditotitan.co/visit-partner?partner_id=seo-7&partner_url=https://rental-car.company/&channel=seo]https://creditotitan.co/visit-partner?partner_id=seo-7&partner_url=https://rental-car.company/&channel=seo[/url]
JaredAgill
A Turkish virtual number is a phone number that allows businesses to establish a local presence in Turkey without needing a physical office. It enables seamless communication with Turkish customers, enhancing trust and accessibility [url=https://compsch.com/news/kak-kupit-virtualnyj-nomer-v-turcii-u-hottelecom.html]номер телефона Турции[/url]
RichardPraph
Мы предоставляем широкий спектр услуг, включая оценку, коррекцию лечения, "второе" мнение, назначение препаратов и проведение терапии, наблюдение за динамикой вашего состояния [url=https://seminet.blogspot.com/2023/10/blog-post_21.html]https://seminet.blogspot.com/2023/10/blog-post_21.html[/url]
MichaelFaump
Beli produk Hemp Custom Wear online, produk terlengkap dan harga terbaik. Dapatkan berbagai promo menarik. Belanja aman dan nyaman hanya di Tokopedia [url=][/url]
ThomasGunse
Furniture of any shape and style looks very attractive and modern in ULTRA fabric [url=https://app.safeteamacademy.com/switch/en?url=https://rental-car.company/]https://app.safeteamacademy.com/switch/en?url=https://rental-car.company/[/url]
AndrewEvase
Одной из дополнительных мотиваций для приобретения временного виртуального номера в Турции является экономия средств [url=https://blogua.org/nemnogo-pro-virtualnye-nomera/]https://blogua.org/nemnogo-pro-virtualnye-nomera/[/url]
Arthurmuh
Dapatkan berbagai promo menarik. Belanja aman dan nyaman hanya di Tokopedia. Beli produk Hemp Custom Wear online, produk terlengkap dan harga terbaik [url=http://info-igor.org/Igorsearch/search.pl?Match=1&Realm=Igor2019&Terms=https://ngatiranana.org.uk/]http://info-igor.org/Igorsearch/search.pl?Match=1&Realm=Igor2019&Terms=https://ngatiranana.org.uk/[/url]
JeffreyHop
Smoking in India is one of the oldest industries and provides employment to more than five million people directly and indirectly [url=https://palletgo.vn/change_language.aspx?lid=2&returnUrl=https://www.indiesmoke.co.in/]https://palletgo.vn/change_language.aspx?lid=2&returnUrl=https://www.indiesmoke.co.in/[/url]
AndrewEvase
Наша виртуальная телефонная система, ориентированная на Турцию, позволяет вам перенаправлять входящие звонки конкретным агентам службы поддержки клиентов [url=https://drimtim.ru/dlya-chego-mozhet-potrebovatsya-virtualnyj-nomer-turcii.html]https://drimtim.ru/dlya-chego-mozhet-potrebovatsya-virtualnyj-nomer-turcii.html[/url]
MichaelImage
Металлопрокат чёрный, цветной, нержавеющий и оцинкованный. Производство, работа с заводами производителями. Поставка от 1 штуки [url=http://lsp-metall.ru/]прокат металл[/url]
Angelbindy
Крупнейший трейдер продажи металлопроката. 24/7. Скидка на опт. Доставка за 2 часа [url=http://samarmatura.ru/]цена арматуры за тонну в москве[/url]
MichaelScaxy
DankBros Cannabis is your go-to source for same-day marijuana delivery! Our collection of products keeps growing, with all your favorite strains and edibles [url=http://mugidensetsu.com/st-manager/click/track?id=10450&type=banner&url=https://takizo.shop/&source_url=https://cutepix.info/]http://mugidensetsu.com/st-manager/click/track?id=10450&type=banner&url=https://takizo.shop/&source_url=https://cutepix.info/[/url]
Roberthaw
В современном мире интернет-торговли платформа Авито стала одним из самых популярных мест для покупки и продажи различных товаров и услуг. Каждый день миллионы пользователей взаимодействуют друг с другом, обмениваются сообщениями, предлагают свои товары и, конечно же, успешно завершают сделки [url=https://warezspace.ru/preimuundefinedestva-ispol-zovaniya-odnorazovogo-nomera-telefona-ot-kompanii-did-virtual-numbers]https://warezspace.ru/preimuundefinedestva-ispol-zovaniya-odnorazovogo-nomera-telefona-ot-kompanii-did-virtual-numbers[/url]
Nathandeany
Are you looking to purchase cannabis in Canada? Your search ends here! We stand out as the premier online cannabis Toronto dispensary, specializing in convenient mail-order cannabis delivery [url=https://in.tempus.no/AbpLocalization/ChangeCulture?cultureName=se&returnUrl=https://www.radiocentre.ca/]https://in.tempus.no/AbpLocalization/ChangeCulture?cultureName=se&returnUrl=https://www.radiocentre.ca/[/url]
LamarAlems
Discover our BDSM category, where we offer a wide range of products to enhance your sensual exploration and play. From restraints and blindfolds to whips and paddles, our carefully curated selection ensures you find the perfect tools to fulfill your desires safely and consensually [url=http://www.talad-pra.com/goto.php?url=https://simbasportsclub.co.tz/]http://www.talad-pra.com/goto.php?url=https://simbasportsclub.co.tz/[/url]
Floydoriem
Виртуальный номер представляет собой телефонный номер, который работает через интернет, а не через традиционные телефонные сети. Этот номер можно использовать для приема и отправки звонков и сообщений, как обычный телефон, но с множеством дополнительных преимуществ [url=https://sovetok.com/news/virtualnyj_nomer_navsegda_zachem_ego_pokupajut_i_kak_ispolzujut/2024-09-23-19979]https://sovetok.com/news/virtualnyj_nomer_navsegda_zachem_ego_pokupajut_i_kak_ispolzujut/2024-09-23-19979[/url]
Calvingen
Пистолет для вязки арматуры это современный инструмент, предназначенный для быстрого и надежного соединения арматурных стержней. В отличие от ручного метода, использование такого устройства позволяет значительно сократить время на выполнение строительных работ [url=http://wiki.serialkiller.adele.im/doku.php?id=%20%D0%93%D0%9E%D0%A1%D0%A2%20%D0%B0%D1%80%D0%BC%D0%B0%D1%82%D1%83%D1%80%D0%B0:%20%D1%81%D0%BE%D0%B2%D0%B5%D1%82%D1%8B%20%D0%BF%D0%BE%20%D1%83%D1%81%D1%82%D0%B0%D0%BD%D0%BE%D0%B2%D0%BA%D0%B5%20%D0%B8%20%D0%BC%D0%BE%D0%BD%D1%82%D0%B0%D0%B6%D1%83]http://wiki.serialkiller.adele.im/doku.php?id=%20%D0%93%D0%9E%D0%A1%D0%A2%20%D0%B0%D1%80%D0%BC%D0%B0%D1%82%D1%83%D1%80%D0%B0:%20%D1%81%D0%BE%D0%B2%D0%B5%D1%82%D1%8B%20%D0%BF%D0%BE%20%D1%83%D1%81%D1%82%D0%B0%D0%BD%D0%BE%D0%B2%D0%BA%D0%B5%20%D0%B8%20%D0%BC%D0%BE%D0%BD%D1%82%D0%B0%D0%B6%D1%83[/url]
RalphSwalm
Mint Mobile re-imagined the wireless shopping experience and made it easy and online-only. No stores. No salespeople. Just huge direct to you savings on [url=https://www.himirror.com/member/checkConnection?r=https://www.diversdeluxe.co.za/&s=/]https://www.himirror.com/member/checkConnection?r=https://www.diversdeluxe.co.za/&s=/[/url]
Mariodiolf
Когда нужно создать что-то надежное, важны не только материалы, но и их правильный выбор. Это касается как масштабных проектов, так и небольших объектов [url=http://vyvoj.barvinek.net/doku.php?id=%20%D0%9F%D1%80%D0%BE%D1%84%D0%B8%D0%BB%D1%8C%D0%BD%D0%B0%D1%8F%20%D1%82%D1%80%D1%83%D0%B1%D0%B0%2040%D1%8540%20%D0%B2%20%D0%BC%D0%B5%D0%B1%D0%B5%D0%BB%D0%B8:%20%D0%BA%D0%B0%D0%BA%20%D1%81%D0%B4%D0%B5%D0%BB%D0%B0%D1%82%D1%8C%20%D0%BF%D1%80%D0%B0%D0%B2%D0%B8%D0%BB%D1%8C%D0%BD%D1%8B%D0%B9%20%D0%B2%D1%8B%D0%B1%D0%BE%D1%80]http://vyvoj.barvinek.net/doku.php?id=%20%D0%9F%D1%80%D0%BE%D1%84%D0%B8%D0%BB%D1%8C%D0%BD%D0%B0%D1%8F%20%D1%82%D1%80%D1%83%D0%B1%D0%B0%2040%D1%8540%20%D0%B2%20%D0%BC%D0%B5%D0%B1%D0%B5%D0%BB%D0%B8:%20%D0%BA%D0%B0%D0%BA%20%D1%81%D0%B4%D0%B5%D0%BB%D0%B0%D1%82%D1%8C%20%D0%BF%D1%80%D0%B0%D0%B2%D0%B8%D0%BB%D1%8C%D0%BD%D1%8B%D0%B9%20%D0%B2%D1%8B%D0%B1%D0%BE%D1%80[/url]
RalphSwalm
Looking for a new sex toy to use with your partner? Tease and explore each other with our exciting range of [url=http://www.acetaxandrealty1.com/frame.asp?frameurl=https://radiocentre.ca/]http://www.acetaxandrealty1.com/frame.asp?frameurl=https://radiocentre.ca/[/url]
https://lvivforum.pp.ua/
It's really very difficult in thjs full of activity life to listen news on Television, so I simply use internet for that purpose, and take the newest news. https://lvivforum.pp.ua/
BrianCiz
Обмен криптовалюты в Киеве Лучший курс Безопасно купить/продать, обменять крипту на наличные в городе Киев (Украина) через Онлайн криптообменник [url=https://www.0552.ua/list/484936]Обмен USDT TRC20 на Приват24[/url]
PerryCet
Dankbros is one of Canada's most reputable online marijuana dispensaries. We guarantee that you'll receive the best strains, concentrates, and accessories [url=https://www.ark-forum.de/proxy.php?link=https://dankbros.net/]https://www.ark-forum.de/proxy.php?link=https://dankbros.net/[/url]
Richardnoima
DANKBROS LTD - Free company information from Companies House including registered office address, filing history, accounts, annual return, officers [url=http://www.parmentier.de/cgi-bin/link.cgi?https://www.dankbros.net/]http://www.parmentier.de/cgi-bin/link.cgi?https://www.dankbros.net/[/url]
AdrianAdubs
Мы продаем устройства для систем водоснабжения, отопления, канализации и мебель под сантехнику. Поможем создать пространство с комфортными для жизни условиями [url=https://www.ozon.ru/product/1416176280]Шланговое подключение Aquatek AQ2454CR Хром[/url]
Michelle
Wonderful goods from you, man. I have understand your stuff previous to and you are just too wonderful. I reawlly like what you have acquired here, really like what you're saying and the way iin which you say it. You make it entertaining and you still take care oof to keep it smart. I can not wait to read far more from you. This is really a tremendous site. https://lvivforum.pp.ua/
WalterRumma
Luka Doncic and Boban Marjanovic have been seen together frequently off the court, and their friendship has been well-documented through social [url=http://otido.ua/ox/www/delivery/ck.php?ct=1&oaparams=2__bannerid=576__zoneid=1__cb=e99c429137__oadest=https://www.lukafriend.com/]http://otido.ua/ox/www/delivery/ck.php?ct=1&oaparams=2__bannerid=576__zoneid=1__cb=e99c429137__oadest=https://www.lukafriend.com/[/url]
Robertmef
Заказывая окно и установку в одной компании, Вы можете сэкономить время и силы на контроль работы разных подрядчиков. Комплексный подход к услуге обеспечивает более точный монтаж конструкции с учетом всех особенностей системы остекления. Наши мастера не только аккуратно установят окна, но и проследят за качеством работы фурнитуры. Как производители, мы контролируем поставки сырья и следим за качеством продукта на всех этапах, предлагая впечатляющую гарантию на профили — 25 лет [url=https://vaokno.ru/]заказать окно москва[/url]
PhilipKeS
Разработка проекта СЗЗ (санитарно защитная зона) для объектов негативного воздействия в Москве и Московской области. Оценка источников загрязнения на производстве, согласование проекта в Роспотребнадзоре https://telegra.ph/15-ponyatnyh-otvetov-o-proekte-SZZ-sanitarno-zashchitnaya-zona-10-17
Dennisviz
This kit comes in a zippered pouch and includes 2 specially developed Scuba Wrenches, high quality crescent wrench, Phillips head and flat head screw drivers [url=http://reg.kost.ru/cgi-bin/go?https://boikhuco.co.za/]http://reg.kost.ru/cgi-bin/go?https://boikhuco.co.za/[/url]
AllenJat
Your go-to Filipino technology forum for discussions on mobile networks, internet, phones, media, computers, gaming, news, and a variety of topics related to [url=http://www.triciclo.se/Mailer/Click.asp?cid=b0210795-525e-482f-9435-165934b01877&goto=https://www.phforums.co.za/]http://www.triciclo.se/Mailer/Click.asp?cid=b0210795-525e-482f-9435-165934b01877&goto=https://www.phforums.co.za/[/url]
RichardStods
Разработка ПНООЛР — проект нормативов образования отходов и лимитов на их размещение. Экологическая отчетность для предприятий в Москве и Московской области https://vc.ru/u/3791103-studiya-zr/1506729-pnoolr-chto-nuzhno-znat-pri-razrabotke-proekta-normativov-obrazovaniya-i-razmesheniya-othodov
Elijahcef
There are many benefits to using a Taiwan virtual number to receive text messages . First, it provides users with a temporary and secure phone number without having to buy a new SIM card. Second, it is suitable for a variety of scenarios, including social media registration, online shopping, and two-factor authentication [url=http://www.stgrrc.cn/20241017/34108116.html]http://www.stgrrc.cn/20241017/34108116.html[/url]
RobertWhodo
Telegram virtual phone number is a virtual phone number designed for registering Telegram accounts. Unlike physical SIM cards, virtual numbers are generated online and users can use them without having to buy a new SIM card [url=http://www.qbwfn.cn/20241017/29638611.html]http://www.qbwfn.cn/20241017/29638611.html[/url]
Josephfopay
Данная служба предоставляет услуги круглосуточного вскрытия замков и дверей в Москве. Мастера во всех районах города http://vskrytie-zamkov.su
TimothyCob
Сериал «Друзья» — это тот случай, когда даже спустя десятилетия после его выхода невозможно представить свою жизнь без этих уютных вечеров перед экраном, где всё кажется понятным и близким [url=http://mro.or.kr/?document_srl=114433]http://mro.or.kr/?document_srl=114433[/url]
JefferyRup
Грамотно организованный процесс подготовки сотрудников позволяет не только повысить их квалификацию, но и открыть новые возможности для роста [url=http://beer.waltermourao.com.br/index.php?title=%20%D0%A1%D0%BE%D0%B2%D1%80%D0%B5%D0%BC%D0%B5%D0%BD%D0%BD%D1%8B%D0%B5%20%D1%82%D1%80%D0%B5%D0%BD%D0%B4%D1%8B%20%D0%B2%20%D0%BE%D0%BD%D0%BB%D0%B0%D0%B9%D0%BD-%D0%BE%D0%B1%D1%83%D1%87%D0%B5%D0%BD%D0%B8%D0%B8%20%D1%81%D0%BE%D1%82%D1%80%D1%83%D0%B4%D0%BD%D0%B8%D0%BA%D0%BE%D0%B2]http://beer.waltermourao.com.br/index.php?title=%20%D0%A1%D0%BE%D0%B2%D1%80%D0%B5%D0%BC%D0%B5%D0%BD%D0%BD%D1%8B%D0%B5%20%D1%82%D1%80%D0%B5%D0%BD%D0%B4%D1%8B%20%D0%B2%20%D0%BE%D0%BD%D0%BB%D0%B0%D0%B9%D0%BD-%D0%BE%D0%B1%D1%83%D1%87%D0%B5%D0%BD%D0%B8%D0%B8%20%D1%81%D0%BE%D1%82%D1%80%D1%83%D0%B4%D0%BD%D0%B8%D0%BA%D0%BE%D0%B2[/url]
RichardBub
Данная студия предоставляет услуги по продвижению сайтов и интернет-магазинов в Москве. Используется комплексный подход. Различные доработки сайта http://prodvizhenie-saytov-moskva.ru
JosephDeace
Территория строгих правил и высоких налогов — Западная Европа манит iGaming-операторов, обещая богатство и успех. И не удивительно — на эту часть света приходится почти половина объема всего мирового рынка онлайн-гемблинга [url=https://mellstroybonus.com]на какой площадке стримит мелстрой[/url]
CurtisDwecy
В одном месте можно купить все необходимое оптом: упаковочное, весовое, обвязочное оборудование, аксессуары для фасовки [url=http://amplituda74.ru/]лабораторное оборудование пищевой промышленности[/url]
Jamesvew
Пищевое оборудование и станки из Китая под ключ. Закупка, проверка, доставка, таможенное оформление [url=http://msmservice.ru/]рынок оборудования для пищевой промышленности в россии[/url]
WillieArike
Современные системы управления помогают контролировать каждый этап, от первичной обработки до упаковки. Это не только снижает риск ошибок, но и экономит ресурсы [url=https://xn--80aeccht8cge.xn--p1ai/content/uspehi-rossiyskih-kompaniy-na-mezhdunarodnoy-arene-pishchevogo-oborudovaniya]https://xn--80aeccht8cge.xn--p1ai/content/uspehi-rossiyskih-kompaniy-na-mezhdunarodnoy-arene-pishchevogo-oborudovaniya[/url]
Stephenguart
Рынок предлагает широкий спектр решений, от простых ручных устройств до сложных автоматизированных систем. Выбор подходящей техники может оказаться непростой задачей, особенно учитывая разнообразие предложений и технологии, доступные на сегодняшний день [url=http://masyasha.ru/index.php?option=com_k2&view=itemlist&task=user&id=84130]http://masyasha.ru/index.php?option=com_k2&view=itemlist&task=user&id=84130[/url]
Stephenguart
Если разбирать термин с позиции экономики, то конкуренцией является процесс взаимосвязи, взаимодействия и борьбы между предприятиями на рынке с целью обеспечить себе лучшие возможности реализации товаров и услуг для удовлетворения потребностей покупателей [url=http://shooting-russia.ru/forum/?PAGE_NAME=message&FID=11&TID=16291&TITLE_SEO=16291-raznoobrazie-tekhnologiy-pererabotki-ovoshchey_-oborudovanie-dlya-kazhdogo-sluchaya.&MID=16566&result=new#message16566]http://shooting-russia.ru/forum/?PAGE_NAME=message&FID=11&TID=16291&TITLE_SEO=16291-raznoobrazie-tekhnologiy-pererabotki-ovoshchey_-oborudovanie-dlya-kazhdogo-sluchaya.&MID=16566&result=new#message16566[/url]
ThomasCitle
Игровой азартный клуб Gama casino работает по лицензии Кюрасао и принимает денежные ставки у игроков из большинства стран мира [url=https://modelistov.ru/]скачать игровые автоматы на андроид[/url]
Brianideok
Откройте успешный бизнес в сфере ремонта вместе с нами - https://expertremonta.kz/franchise
Lloydlak
Ваш уют — наша задача: ремонт под ключ с заботой о каждом клиенте - https://expertremonta.kz/ уже 12 лет предоставляет услуги по ремонту квартир
CharlesWal
Профессия QA-инженера: задачи на разных этапах разработки, навыки и необходимые знания для работы в сфере тестирования качества программного продукта https://dzen.ru/a/ZvqB94uwl1C-1ivx?share_to=link
MichaelFek
Что важно знать о видах тестирования программ, сайтов и приложений, чтобы пройти собеседование на позицию тестировщика или QA-инженера в IT-компанию https://vc.ru/u/3791103-studiya-zr/1427036-voprosy-pro-vidy-testirovaniya-na-sobesedovanii-v-qa-kak-k-nim-otnositsya
Joshuaepits
Kraken гарантирует постоянный и стабильный доступ к своему ресурсу через официальные ссылки. У вас под рукой всегда будет актуальная информация по поводу ресурса https://kra12.ca
DanielWrite
Профессиональная служба эвакуации автомобилей, предоставляющая круглосуточную помощь эвакуаторов в любой непредвиденной ситуации — будь то поломка, авария или необходимость перевозки вашего авто [url=https://www.km.ru/avto/2021/05/01/887648-manipulirovat-bez-manipulyatsii-ili-chto-takoe-evakuator-manipulyator]https://www.km.ru/avto/2021/05/01/887648-manipulirovat-bez-manipulyatsii-ili-chto-takoe-evakuator-manipulyator[/url]
DanielWrite
Мы эвакуируем легковые и грузовые автомобили, мотоциклы и другие виды техники. Услуги эвакуации оказывают профессиональные водители, которые выезжают в любой непредвиденной ситуации — будь то поломка, авария или необходимость перевозки вашего авто [url=http://kkl5124.blog85.fc2.com/blog-entry-88.html]http://kkl5124.blog85.fc2.com/blog-entry-88.html[/url]
Jameskah
Онлайн магазин игр. Купить лицензионные ключи для компьютерных игр, ключи и аккаунты Steam, Origin, Uplay, Minecraft [url=https://amelie-style.ru/gde-vygodno-kupit-klyuchi-ot-igr-steam.html]аккаунты стим[/url]
StevenVam
Технически это просто звонки через интернет. Достаточно давно некоторые мессенджеры предлагали подобное. Но в большинстве случаемв там работали только исходящие звонки [url=https://kinook.by/interesnoe/optimizacziya-effektivnosti-biznesa-s-pomoshhyu-virtualnyh-nomerov.html]https://kinook.by/interesnoe/optimizacziya-effektivnosti-biznesa-s-pomoshhyu-virtualnyh-nomerov.html[/url]
DonaldNig
Виртуальный номер — это обычный номер телефона с такими дополнительными преимуществами, как многоканальность и отсутствие географической привязки [url=https://pro-smartfon.ru/virtualnye-nomera-ssha-dlya-biznesa]https://pro-smartfon.ru/virtualnye-nomera-ssha-dlya-biznesa[/url]
DonaldNig
Наша компания https://sveller2buy.ru/ профессионально занимается поставкой сортового металлопроката оптом и в розницу
MichaelNuh
Виртуальный номер телефона — это номер без SIM-карты. С Numero вы можете получить виртуальные телефонные номера в более чем 80 странах [url=https://systemreq.ru/sekrety-uspeshnogo]Виртуальный номер навсегда[/url]
EugeneWek
Аренда виртуальных телефонных номеров для 75 городов России и 38 стран мира. Звонки онлайн на городские и мобильные (сотовые) номера, бесплатный прием [url=https://zyryanovsk.kz/news/virtualnye-nomera-strategicheskaya-vozmozhnost-postroit-nadezhnyj-biznes.html]Виртуальные номера[/url]
Dennisveivy
Купить металлическую профильную трубу в розницу. Стальные профильные трубы по ГОСТ и ТУ, продажа профтрубы по низкой цене за метр с доставкой [url=http://meffert-yar.ru/]труба профильная стоимость[/url]
JamesMUg
Независимо от того, являетесь ли вы опытным пользователем или только начинаете познавать блокчейн, MetaMask помогает вам подключиться к децентрализованной сети: новому интернету <a href="https://www.pgyer.com/apk/apk/io.metamask">metmamsk wallet</a>
Dennisveivy
Труба стальная профильная – длинное пустотелое тело различного сечения, произведенное из углеродистой или низколегированной стали, используемое в качестве элемента металлоконструкции <a href="http://meffert-yar.ru/">купить трубу профильную в москве цена</a>
JamesMUg
Надежный поставщик недорогой строительной арматуры. Качественная арматурная сталь а500с по выгодной цене с доставкой <a href="http://vodoley66.ru">стоимость арматуры</a>
AndrewCoecy
Купить онлайн металл в нашем интернет магазине достаточно просто. Для этого вам необходимо перейти в интересующий вас раздел из нашего каталога <a href="http://metal-lesnoy.ru/">металлом купить</a>
AndrewKef
Арматура — это металлический прут, используемый для армирования железобетонных конструкций. Стержни арматуры изготавливаются из углеродистой <a href="https://a4-tech.ru/">строительная арматура оптом</a>
Richardvop
Профильные трубы – категория металлопроката, которая включает в себя изделия с сечением, отличным от круглого. Ассортимент профильных труб <a href="http://ivmetall37.ru">купить металл профильная труба</a>
PhillipAling
Цены на травматические пистолеты различаются в зависимости от производителя, мощности оружия и других показателей <a href="https://telegra.ph/KUPIT-TRAVMATICHESKOE-BOEVOE-ORUZHIE-11-06-2">Купить лицензию на оружие</a>
StephenRoarm
Онлайн магазин игр. Купить лицензионные ключи для компьютерных игр, ключи и аккаунты Steam, Origin, Uplay, Minecraft <a href="https://pg11.ru/igry-kompiuternye">ссылка</a>
RickeyGig
Эффективные методы и средства для уничтожения жука короеда в доме. Где заказать профессиональные услуги обработки деревьев на участке от насекомых вредителей в Москве? https://dzen.ru/a/Zrm0OQRatQiCoOgh
Robertbal
Бюстгальтеры с октрытой спиной с бесплатной доставкой в интернет-магазине, актуальные цены, в наличии большой ассортимент моделей <a href="https://www.ozon.ru/seller/caitline-242390">размер чашки бюстгальтера</a>
WesleyNot
Преимущества покупки алкоголя в Ароматном Мире · широкий ассортимент алкогольных и безалкогольных напитков высокого качества; · индивидуальная система скидок <a href="https://telegra.ph/Dostavka-alkogolya-Moskva-11-08">доставка алкоголя на дом москва</a>
Robertbycle
Как получить, переоформить и продлить лицензию на газовое оружие. Кто может приобрести газовое оружие. Необходимые документы для лицензии на приобретение <a href="https://telegra.ph/KUPIT-TRAVMATICHESKOE-BOEVOE-ORUZHIE-11-08">купить травмат лидер</a>
RodneyAgola
Размытость симптоматики большинства заболеваний нервной системы требует особого подхода к диагностике. Опытные специалисты центра неврологии больницы Ассута в Израиле разрабатывают индивидуальные планы диагностических мероприятий для пациентов <a href="https://moscow.service-med.com/neurology/">https://moscow.service-med.com/neurology/</a>
Davidacike
Бесплатные виртуальные номера страны Белоруссия с кодом +375 для приема СМС, получения активации сервисов и аренды мобильного телефона <a href="https://club60.org/internet/10749-preimushhestva-virtualnyx-nomerov.html">купить одноразовый номер для смс</a>
StephenRoarm
Ни одно застолье невозможно представить себе без освежающих безалкогольных напитков. Сейчас вам не придется тратить свое время и силы на то, чтобы ездить в магазины и покупать соки, минеральную воду <a href="https://telegra.ph/EHSKORT-MOSKVA--RED-ROOM-11-08">доставка алкоголя на дом круглосуточно москва недорого</a>
ScottCap
В настоящее время одной из ключевых современных информационных угроз для общества в сфере медиабезопасности становится вовлечение детей и подростков в деструктивные Интернет-сообщества <a href="https://telegra.ph/Sliv-shkolnic-18-11-06">слив молодых школьниц тг</a>
ManuelTub
Melbet - начинай играть на реальные деньги на официальном сайте онлайн казино Мелбет и выигрывай крупные суммы в популярных игровых автоматах <a href="https://telegra.ph/Kometa-Kazino-11-06">kometa casino зеркало сайта online 7kcasino919 com</a>
BruceDeeta
Ведь есть же десятки сервисов для номеров из других стран. А беларусские форумы огорожены, им подавай только их собственный картофель типа +375 <a href="https://stroymaster-base.ru/hozyayushka/sovety-hozyayke/virtualnyj-nomer-telefona-indonezii-preimushhestva-i-vozmozhnosti.html">купить виртуальный номер Индонезии</a>
JohnnyNip
Веб агентство в Москве выполняет разработку сайтов на платформе Битрикс под ключ. Дополнительные услуги - продвижение в поисковых системах Яндекс и Гугл, техническая поддержка, обслуживание, аудит, тестирование, наполнение контентом, контекстная реклама и маркетинг <a href="https://webstudiya-razrabotki.ru/">https://webstudiya-razrabotki.ru/</a>
AaronHeicy
Создание лендингов под ключ в студии в Москве включает проектирование, дизайн и программирование, обеспечивающее эффективность и удобство использования. Также предоставляются услуги: оптимизация для Яндекс и Google, настройка рекламных кампаний, поддержка, обслуживание и ведение маркетинга <a href="https://studiya-poddergki.ru/">разработка лендинга</a>
Geraldmot
Разработка лендингов в студии в Москве осуществляется с учетом современных маркетинговых стратегий и требований рынка. К основным услугам добавляются: аудит и анализ конверсии, продвижение в поисковых системах, контентное наполнение, настройка CRM и профессиональная техническая поддержка <a href="https://webstudiya-landing.ru/">https://Webstudiya-Landing.ru/</a>
Phillipexoge
Разработка сайтов на платформе 1С-Битрикс в студии в Москве включает полный цикл: от проектирования до запуска и дальнейшего сопровождения. Также предлагаются услуги: оптимизация сайта для поисковых систем, интеграция с хостингом, контентное наполнение, анализ данных и маркетинговые стратегии <a href="https://webstudiya-moscow.ru/">https://Webstudiya-Moscow.ru/</a>
PhilliptuB
Хочешь добавить остроты в свою интимную жизнь и не знаешь, с чего начать? У нас есть то, что тебе нужно! В нашем магазине можно купить секс игрушки по самым разным вкусам: от классических вибраторов и фаллоимитаторов до инновационных игрушек для взрослых, которые подарят новые ощущения. Мы предлагаем заказать секс игрушки онлайн — это просто и удобно, ведь интим игрушки станут идеальным дополнением для разнообразных сексуальных приключений. У нас только самые качественные секс товары, созданные, чтобы доставлять максимум удовольствия. Хотите попробовать что-то новое? Стимуляторы, БДСМ аксессуары и игрушки для секса уже ждут вас. Дешево? Конечно, у нас всегда есть предложения, чтобы сделать стоимость покупки более приятной. Будь то эротические игрушки для себя или для партнера — мы знаем, как сделать вашу ночную жизнь по-настоящему яркой <a href="https://topsexshop3.co.ua/">https://topsexshop3.co.ua/</a>
CharlieStemy
Апартаменты Napa Gem в пешей доступности от одного из самых красивых пляжей Кипра, а также бурного веселья на шумном летнем курорте Айя-Напа <a href="http://nedvizhimostrussa.ru/">у моря недорого кипр недвижимость</a>
EddieHense
Продажа недвижимости на Кипре: 10 674 предложения с ценами и фото. Tranio поможет подобрать и купить жилье на Кипре стоимостью от 54 000€ <a href="http://redstoneestate.ru">купить дом на кипре на берегу</a>
EddieEsoRi
В нейрохирургических отделениях израильских клиник сегодня производятся самые революционные операции на спинном и головном мозге, которые максимально результативны и безопасны <a href="https://neurosurgeryisrael.wordpress.com">https://neurosurgeryisrael.wordpress.com</a>
Thomasgaile
Мы печатаем развороты фотокниг на высококачественной профессиональной фотобумаге Fujicolor Crystal Archive Digital тип DP II (матовая или тиснёная) на современной машине Noritsu QSS 3704HD <a href="http://basova-photo.ru/">напечатать фотокнигу онлайн</a>
RobertRirty
Откройте мир вождения с нашей автошколой, обучающей безопасным навыкам управления автомобилем. Мы предлагаем высококачественное обучение вождению, которое поможет вам уверенно управлять автомобилем в любых условиях <a href="https://avtoschoolavtoritet22.ru/">москва автошкола цена</a>
Patrickpek
Фотосфера – это долгожданный момент творчества, вдохновение, радость, уникальные дизайны и невероятно красивые решения. Это творческая лаборатория, где люди на основе снимков и изображений создают шедевры для себя, родных и друзей <a href="https://fotooks.ru/">фотосалон рядом</a>
Robertwouch
Для успешного использования платформы необходимо иметь доступ к личному кабинету. Этот процесс включает несколько простых шагов, которые помогут вам зайти в аккаунт и использовать все его возможности. Независимо от устройства, важен правильный подход, чтобы избежать возможных ошибок <a href="http://wiki.hightgames.ru/index.php?title=%20%D0%9A%D0%B0%D0%BA%20%D0%B2%D1%81%D0%B5%D0%B3%D0%B4%D0%B0%20%D0%BE%D1%81%D1%82%D0%B0%D0%B2%D0%B0%D1%82%D1%8C%D1%81%D1%8F%20%D0%BD%D0%B0%20%D1%81%D0%B2%D1%8F%D0%B7%D0%B8%20%D1%81%201win">http://wiki.hightgames.ru/index.php?title=%20%D0%9A%D0%B0%D0%BA%20%D0%B2%D1%81%D0%B5%D0%B3%D0%B4%D0%B0%20%D0%BE%D1%81%D1%82%D0%B0%D0%B2%D0%B0%D1%82%D1%8C%D1%81%D1%8F%20%D0%BD%D0%B0%20%D1%81%D0%B2%D1%8F%D0%B7%D0%B8%20%D1%81%201win</a>
шлюхи город москва
[url=https://telegra.ph/EHSKORT-MOSKVA--RED-ROOM-11-08]шлюхи москва киевская[/url]
EnriqueScesK
Мы – это интернациональная команда с большим опытом работы в сфере микрофинансирования, кредитования и банковского дела. Наши сотрудники ежедневно вносят свой вклад в микрофинансирование, помогая клиентам и партнерам выбрать лучшее решение для развития бизнеса <a href="http://otrafin.ru/">кредит ооо без залога и поручителей</a>
Ernesttus
Предложения для открытия бизнеса ИП с нуля — редкость. Для получения займа предприниматель уже должен работать на рынке. Обычно не меньше 6 месяцев <a href="https://oaocentrinvest.ru/">льготный кредит на развитие бизнеса</a>
Eugenebeape
Мы предлагаем разнообразные курсы, чтобы соответствовать вашим потребностям в обучении вождению. Начните свою карьеру на дороге прямо сейчас вместе с нами <a href="https://donavtodor.ru/">онлайн обучение автошкола москва</a>
рекламные товары за отзывы на ВБ
[url=https://tenchat.ru/media/2728961-razdacha-tovarov-za-otzyvy-gayd-po-vykupam]раздачи товаров за отзывы на Ozon[/url]
FreddieHaddy
Использование разнообразных источников финансирования помогает компаниям достигать устойчивого развития, минимизируя риски и максимизируя эффективность инвестиций в проекты и инновации <a href="http://www.ilmarhit.it/component/kunena/11-business-professional-associations/427583?Itemid=0#427583">http://www.ilmarhit.it/component/kunena/11-business-professional-associations/427583?Itemid=0#427583</a>
GradyLiept
Лизинг — услуга для компаний и ИП, снижающая затраты на покупку транспортных средств для коммерческих и личных целей. Выберите автомобиль, подпишите договор <a href="https://car-yaroslavl.ru/">лизинг легкового автотранспорта</a>
Richardtob
Подскажите, где в Москве можно купить качественную строительную технику, такую как башенные краны или мачтовые подъемники? Интересуют надежные компании с хорошей репутацией <a href="http://www.delishis.ru/forum/?Subdiv_ID=11&Topic_ID=10854">http://www.delishis.ru/forum/?Subdiv_ID=11&Topic_ID=10854</a>
товары за отзыв Ozon
[url=https://t.me/tovaryzaotzivkeshbek]как найти товар за отзыв на Вайлдберриз[/url]
Davidmeava
Расчет и покупка спецтехники в лизинг для юр. лиц и ИП. Лучшие предложения лизинга на строительную технику и быстрое оформление <a href="http://spectehnikaleasing.ru/">лизинг москва спецтехники</a>
LamarVal
Приобретение нового оборудования в лизинг для бизнеса на выгодных условиях. Длительные сроки финансирования. Специальные программы от поставщиков <a href="https://ptleasing.ru/">лизинг оборудования для юридических лиц условия</a>
CharlesKaf
Какую спецтехнику можно взять в лизинг? В нашей компании предоставляется большой выбор спецтехники для лизинга. Вам доступны экскаваторы, погрузчики, бульдозер <a href="https://welcome-leasing.ru/">лизинг для юридических лиц на спецтехнику</a>
выкупы товаров за отзывы на Ozon
[url=https://tenchat.ru/media/2750073-tovary-za-otzyv-razdachi-s-keshbekom-ili-bally-za-otzyv]выкупы товаров за отзыв WB[/url]
Davidmed
Друзья, мне нужен совет знающих. Можете ли Вы мне подсказать каким образом можно вывести на гривну криптовалюту? Какие обменники есть их хороших <a href="https://service-core.com.ua/forum/post8375.html#p8375">http://www.vladimir.ru/forum/forum/thread/45769</a>
Georgeram
На приеме гинеколог проводит осмотр воспалений, новообразований и других гинекологических патологий, проводит диагностику заболеваний женских половых органов и выявляет их на ранних стадиях <a href="https://www.renderosity.com/users/id:1588592">https://www.renderosity.com/users/id:1588592</a>
MichaelBow
Как выбрать гирлянды для новогоднего оформления фасада дома? Виды подсветки, лучшие материалы, обзор разных моделей гирлянд и советы по монтажу: https://dzen.ru/a/Zy5D8pM8zzfwUtJ0
RichardRip
Обмен криптовалют на USDT (Tether) является обычной практикой в мире цифровых активов, предлагая стабильную альтернативу более волатильным криптовалютам <a href="http://dexanet.ukrbb.net/viewtopic.php?f=8&t=18763">http://wisdomtarot.tforums.org/viewtopic.php?f=8&t=8925&p=18681#p18681</a>
WilliamVom
Платформа уникальная и отличная в плане удобств (начиная от ввода и вывода средств, заканчивая инструментами для торговли). Постоянные улучшения. Куча графиков <a href="https://www.mayaschool.ru/assets/">покет опшн</a>
Davidoralm
Купить виртуальный сервер VPS/VDS от 169 р/месяц, с возможностью самостоятельного администрирования. Аренда хостинга VPS или VDS <a href="https://optima-k.ru/">аренда серверов</a>
DavidJot
Когда речь идет о комфортной организации пространства, на помощь приходят инновационные подходы. Элементы, которые можно комбинировать и адаптировать, открывают множество возможностей для создания идеального хранилища <a href="http://serverknowledgebase.co.uk/index.php?title=%20%C2%AB%D0%9A%D0%B0%D0%BA%20%D0%BC%D0%BE%D0%B4%D1%83%D0%BB%D1%8C%D0%BD%D1%8B%D0%B5%20%D1%81%D0%B8%D1%81%D1%82%D0%B5%D0%BC%D1%8B%20%D0%BF%D0%BE%D0%BC%D0%BE%D0%B3%D0%B0%D1%8E%D1%82%20%D0%BF%D0%BE%D0%B4%D0%B4%D0%B5%D1%80%D0%B6%D0%B8%D0%B2%D0%B0%D1%82%D1%8C%20%D0%BF%D0%BE%D1%80%D1%8F%D0%B4%D0%BE%D0%BA%20%D0%B2%20%D0%B3%D0%B0%D1%80%D0%B4%D0%B5%D1%80%D0%BE%D0%B1%D0%BD%D0%BE%D0%B9?%C2%BB">металлические гардеробные системы</a>
Thomasdom
Разнообразие предложений на рынке позволяет легко подобрать удобные варианты для хранения личных вещей. Предметы могут быть адаптированы под любые размеры и потребности, что делает процесс организации не только полезным, но и приятным <a href="http://www.icmms.co.kr/bbs/board.php?bo_table=free&wr_id=808324">заказать систему хранения в гардеробную</a>
Williamwed
With BlueWallet, you maintain ownership of your private keys. This Bitcoin wallet is crafted by Bitcoin enthusiasts for the community <a href="https://bluewallet-bitcoin-wallet.en.uptodown.com/android">BlueWallet apk</a>
Manueltub
In the heart of a city renowned for romance, elegance, and sophistication, there lies a world dedicated to offering unforgettable, high-class companionship <a href="http://wiki.motorclass.com.au/index.php?title=_The_Art_of_Seduction:_Why_Paris_is_the_Ultimate_Escort_Destination">http://wiki.motorclass.com.au/index.php?title=_The_Art_of_Seduction:_Why_Paris_is_the_Ultimate_Escort_Destination</a>
Richardger
VPS на Windows — это виртуальный выделенный сервер, развёрнутый в облачном кластере, с предустановленной лицензионной ОС Windows Server. Виртуализация KVM <a href="https://siteboom.ru/">что такое хостинг сайта</a>
Manueltub
Представьте себе: Вы гуляете по улицам Москвы, а вокруг Вас оживают легендарные злодеи и аферисты! Здесь исторические личности сплетаются с киношными персонажами, а за каждым поворотом скрывается тайна <a href="https://captour.ru/subjects/ekskursii-po-moskve-na-tureckom-yazyke/">https://captour.ru/subjects/ekskursii-po-moskve-na-tureckom-yazyke/</a>
Thomasanosy
They might include special diets, herbal supplements, chiropractic care, animal therapy, arts therapy, mindfulness, or relaxation therapies <a href="https://www.reddit.com/user/autismmmccom/">https://www.reddit.com/user/autismmmccom/</a>
CarlosEvole
Интерфейс таких платформ обычно прост и доступен, что делает их привлекательными для новичков и профессионалов. Основные функции ориентированы на то, чтобы дать трейдерам возможность анализировать рыночные тенденции, а также быстро и безошибочно выполнять сделки <a href="http://place-e.ru/index.php?title=%20Pocket%20Option:%20%D0%BE%D1%81%D0%BE%D0%B1%D0%B5%D0%BD%D0%BD%D0%BE%D1%81%D1%82%D0%B8%20%D1%82%D0%BE%D1%80%D0%B3%D0%BE%D0%B2%D0%BB%D0%B8%20%D0%B1%D0%B8%D0%BD%D0%B0%D1%80%D0%BD%D1%8B%D0%BC%D0%B8%20%D0%BE%D0%BF%D1%86%D0%B8%D0%BE%D0%BD%D0%B0%D0%BC%D0%B8">http://place-e.ru/index.php?title=%20Pocket%20Option:%20%D0%BE%D1%81%D0%BE%D0%B1%D0%B5%D0%BD%D0%BD%D0%BE%D1%81%D1%82%D0%B8%20%D1%82%D0%BE%D1%80%D0%B3%D0%BE%D0%B2%D0%BB%D0%B8%20%D0%B1%D0%B8%D0%BD%D0%B0%D1%80%D0%BD%D1%8B%D0%BC%D0%B8%20%D0%BE%D0%BF%D1%86%D0%B8%D0%BE%D0%BD%D0%B0%D0%BC%D0%B8</a>
HenrySex
Sex videos online watch for free from anywhere in the world without subscription and registration <a href="https://1win-official.com/">kids porn</a>
Richardben
A Bitcoin wallet that allows you to store, send Bitcoin, receive Bitcoin and buy Bitcoin with focus on security and simplicity <a href="https://bluewallet-bitcoin-wallet.en.uptodown.com/android">BlueWallet 7.0.5</a>
Kennethjet
Dynamic platform that aggregates live adult entertainment, constantly refreshed with streams from the leading adult webcam platforms like <a href="https://webcamsexpin.com/">live gay porn</a>
Richardstuby
Find the hottest sexwebcam videos and clips, realy hight quality <a href="https://worldsexwebcam.com/">kids porn</a>
Jimmyobjes
Watch and admire beautiful girls getting naked on live cam. The site features cam girls of all types, from petite blonde camgirls to leggy redheads <a href="https://www.webcamsheat.com/">live cam free porn</a>
Jamesrhift
Лессе-Пассе или Теудат Маавар - это oдин из возможных паспортов Израиля, который выдается гражданам этой страны https://xn----7sbbzecaihj2bkbelhgv2p.com/
ThomasRor
Official Starhotels website: book directly on the website at the best available rates for 4 and 5 star hotels in Italy, New York, Paris and London <a href="https://www.hotel-details.com/hotels/category/5-star-hotel-scotland">5 Star Hotel Scotland</a>
CharlesRor
Одним из важнейших экологичных решений в дорожном строительстве является использование переработанных материалов. Это не только помогает сократить количество отходов, но и уменьшает потребность в новых материалах, что снижает негативное воздействие на окружающую среду <a href="https://tigergrp.org/cn/blog/your-guide-to-the-best-luxury-travel-itineraries-in-geneva">A guide to the best itineraries for luxury travel in Geneva</a>
ZacharyPop
Имплантация зубов в Вoлгoграде: 84 клиники с aдресами и ценами от 600 до 500000 рублей, запись. При выборе клиники можно ознакомиться с отзывами других <a href="https://stomvolga.ru">безметалловые коронки на зубы Волгоград</a>
HaroldEvite
Sех videos online watch for free from anywhere in the world without subscription and registration <a href="https://1wins.bj/">extasy</a>
купить оружие без лицензии
[url=https://taplink.cc/ystgk]купить травмат без документов[/url]
Andrekeype
Логопед онлайн проведет диагностику, поможет поставить звуки, проработать дислексию и дисграфию, устранить задержки речевого развития и обогатить словарный запас <a href="https://logoped-online1.ru/">хороший логопед онлайн</a>
MichaelIrott
Начало собственного дела в сфере здравоохранения может быть выгодным и стабильным решением. Этот рынок всегда будет востребован, поскольку потребность в медицинских товарах и услугах не исчезает. Однако для успешного старта важно выбрать правильную модель, которая позволит использовать уже проверенные решения и избежать множества сложностей, характерных для создания бизнеса с нуля <a href="http://www.nfgroup.it/forum/lotta/954">http://www.nfgroup.it/forum/lotta/954</a>
WallacePes
Профессиональная установка камина и дымохода качественно и выгодно с доставкой и установкой под ключ в Москве и Московской области <a href="https://gdekupitdom.ru/news/detail/ustanovka-kamina-s-oblitsovkoy/">Установка камина с облицовкой</a>
DavidRon
GasDank is your go-to for ordering weed online in Canada. We are a safe and discreet marijuana mail order service based in Toronto, Ontario, also offering same-day delivery throughout the GTA <a href="http://www.oppuz.com/redirect?application=avon&track[action]=rclk&track[info][action_src]=sm&track[info][etag]=d6208572-262b-4b34-834e-abc9575159b7&url=https://uberweedshop.co/maps/">http://www.oppuz.com/redirect?application=avon&track[action]=rclk&track[info][action_src]=sm&track[info][etag]=d6208572-262b-4b34-834e-abc9575159b7&url=https://uberweedshop.co/maps/</a>
DonaldMop
На сегодняшний день самым эстетичным методом протезирования считаются безметалловые коронки. При этом под словом «керамика» подразумеваются самые разные химические соединения <a href="https://studiaulybki.ru">имплантация зубов в волгограде цены под ключ</a>
Kevinhaure
Виртуальные номера могут быть очень полезны для бизнеса. Они позволяют компаниям улучшать связь с клиентами, увеличивать продажи и улучшать общую эффективность <a href="https://1st-digital.ru/pochemu-ne-prihodit-kod-podtverzhdeniya-v-instagram-uznaj-vse-nyuansy/">почему не приходит код подтверждения Инстаграм</a>
Anthonycef
Бесплатные виртуальные номера для СМС — это возможность быстро и безопасно проходить верификацию на различных сайтах без регистрации <a href="https://sayt-sozdat.ru/zachem-nuzhen-turetskiy-virtualnyy-nomer/">купить турецкий номер для СМС</a>
Dustinrof
Эвакуатор с манипулятором - универсальное решение для перевозки автомобилей. Он сочетает функции обычного эвакуатора и крана-манипулятора. Это позволяет решать сложные задачи по эвакуации. Манипулятор может поднимать и перемещать грузы в труднодоступных местах <a href="https://tvoiaromat.ru/articles/280504">https://tvoiaromat.ru/articles/280504</a>
AnthonyFUG
Вы можете купить справки в Москве в нашей клинике https://aleksandriya-med.ru/.
TerryAneks
На данный момент антигравийная пленка считается материалом, который отлично защищает кузов авто от различных повреждений. Так, она поможет избежать царапин, потертостей, а также предохраняет машину во время небольших ДТП, и в результате на поверхности авто не появляется ржавчина <a href="https://www.drive2.ru/o/b/720303/">https://www.drive2.ru/o/b/720303/</a>
MichealZes
Вы можете купить справку в медцентре https://smails-clinic.ru/ с доставкой по Москве.
AllenAnync
Множество профессий, связанных с интернетом, становится доступными даже тем, кто ещё не закончил учебу. Знания, полученные в процессе освоения таких специальностей, открывают перспективы и дают шанс на независимость в финансовом плане <a href="http://torgteh-rzn.ru/index.php?option=com_k2&view=itemlist&task=user&id=13829">http://torgteh-rzn.ru/index.php?option=com_k2&view=itemlist&task=user&id=13829</a>
Richarddrubs
Вы можете купить медсправку в нашем мед центре https://med-bez-boli.ru/ в Москве без медкомиссий.
Gregoryseirm
Цифровые технологии в нынешнее время проникают во все сферы жизни, виртуальный номер проявляет себя как неотъемлемым инструментом для эффективного и безопасного общения <a href="https://forum.i.ua/topic/3255">https://forum.i.ua/topic/3255</a>
Richarddrubs
Yazdorova.com – это сайт для женщин, стремящихся к здоровью, красоте и гармонии. Здесь вы найдете полезные советы по похудению, уходу за собой и вдохновение для создания лучшей версии себя https://yazdorova.com/
CarltonVed
С развитием технологий виртуальные номера стали все более персонализированными и настраиваемыми. С помощью специальных сервисов можно выбирать желаемый номер из предложенного списка, настраивать перенаправление звонков, устанавливать голосовое приветствие и даже анализировать статистику звонков <a href="https://gazeta-pravo.ru/virtualnyj-nomer-telefona-preimushhestva-i-vozmozhnosti/">https://gazeta-pravo.ru/virtualnyj-nomer-telefona-preimushhestva-i-vozmozhnosti/</a>
FestivalStarp
Теперь вижу ситуацию иначе. <a href="https://samaravsem.ru/">festivalguru.ru</a>
Trevorrip
In recent years, digital platforms have revolutionized how individuals and businesses handle their finances <a href="https://funsilo.date/index.php?title=_How_to_Backup_Your_Tg_Wallet_for_Safety">https://funsilo.date/index.php?title=_How_to_Backup_Your_Tg_Wallet_for_Safety</a>
Gordonneari
Это проверенный обменник, которым я пользуюсь уже не первый раз. Здесь курс всегда выгодный, обмен происходит быстро, а скрытых комиссий нет. Очень удобно и безопасно для тех, кто хочет обменять криптовалюту на честных условиях <a href="https://tvoyaodessa.mybb.od.ua/viewtopic.php?id=113#p220">https://tvoyaodessa.mybb.od.ua/viewtopic.php?id=113#p220</a>
Walteranolf
Вы можете купить медицинскую справку в мед центре https://hearth-health.ru/ в Москве без прохождения врачей.
Robertsab
Задачи и роль QA-инженера: путь к успешной карьере в области тестирования программных продуктов. Узнайте, какие навыки и знания необходимы специалисту для качественного выполнения задач на всех этапах разработки: https://dzen.ru/a/ZvqB94uwl1C-1ivx
MauriceLOG
Dom Boutique Hotel, boutique hotel: addresses with entrances on the map, reviews, photos, phone numbers, opening hours and how to get there. Accommodation from http://cyprus-apartment.com/
Walteranolf
Вы можете купить справку в клинике https://medikwest.ru/ по Москве с бесплатной доставкой до любой станции метро.
Domingolok
Камеры видеонаблюдения выполняют различные задачи: они помогают отпугивать нарушителей, фиксируют события на охраняемой территории и контролируют действия сотрудников <a href="https://videonabludenie35.ru/">Монтаж видеонаблюдения в Вологде</a>
Williamgob
Вы можете купить справку в поликлинике https://dobromedic.ru/ по Москве с доставкой до станции метро.
PatricksmooF
1xBet Promo Code 2024 - 1XBIG24: enter this code when creating your account to receive up to $100 as a 100% match on your first deposit. The bonus amount must be used in the sports section by placing bets with odds of 1.4 or higher and a 5x wagering requirement within 30 day <a href="https://www.bigcatalliance.org/news/bonus_d_inscription_au_casino_1xbet.html">https://www.bigcatalliance.org/news/bonus_d_inscription_au_casino_1xbet.html</a>
Davidmub
Узнавая все больше о Кипре, вы только убедитесь в привлекательности острова. Лимасол, Пафос, Ларнака, Айя-Напа и Протарас привлекают инвесторов удачным географическим положением, развитой инфраструктурой и тем, что это самые «русскоязычные» города республики <a href="http://holidayhomesplus.co.nz/">small apartment cyprus</a>
TerryGef
Игровая платформа 1хбет щедро вознаграждает новичков приветственным поощрением в разделе “Казино” в размере до 1500 долларов плюс 210 фриспинов <a href="http://monetoss.ru/news/promokod-1xbet-bonus.html">http://monetoss.ru/news/promokod-1xbet-bonus.html</a>
Lindseybip
Вы можете купить справку в медицинском центре https://kristall-med.ru/ в Москве без прохождения врачей.
Waynenat
Средиземноморье привлекает людей со всего мира своей уникальной атмосферой, богатой историей и неповторимыми природными условиями <a href="http://www.nfgroup.it/forum/lotta/911">http://www.nfgroup.it/forum/lotta/911</a>
Lindseybip
Вы можете купить справки в Москве в нашей клинике https://medic-dpo.ru/.
TerryGef
Букмекерская контора 1хБет приготовила для своих клиентов разнообразную систему бонусов и акций, которая привлекает новых участников и поддерживает интерес у постоянных клиентов. Ниже рассмотрим основные бонусы и акции букмекера 1xbet <a href="https://renctas.org.br/pag/1xbet_promo_code_registration_nigeria.html">https://renctas.org.br/pag/1xbet_promo_code_registration_nigeria.html</a>
Waynenat
Выбор места для проживания или отдыха имеет огромное значение для качества жизни. Важно тщательно подойти к вопросу выбора недвижимости, которая будет не только комфортной, но и обеспечит высокий уровень жизни в течение долгого времени <a href="http://ec2-18-222-226-231.us-east-2.compute.amazonaws.com/mediawiki/index.php?title=%20%D0%9A%D0%B0%D0%BA%20%D0%B8%D0%B7%D0%B1%D0%B5%D0%B6%D0%B0%D1%82%D1%8C%20%D0%BE%D1%88%D0%B8%D0%B1%D0%BE%D0%BA%20%D0%BF%D1%80%D0%B8%20%D0%BF%D0%BE%D0%BA%D1%83%D0%BF%D0%BA%D0%B5%20%D0%BA%D0%B2%D0%B0%D1%80%D1%82%D0%B8%D1%80%D1%8B%20%D0%BD%D0%B0%20%D0%9A%D0%B8%D0%BF%D1%80%D0%B5">http://ec2-18-222-226-231.us-east-2.compute.amazonaws.com/mediawiki/index.php?title=%20%D0%9A%D0%B0%D0%BA%20%D0%B8%D0%B7%D0%B1%D0%B5%D0%B6%D0%B0%D1%82%D1%8C%20%D0%BE%D1%88%D0%B8%D0%B1%D0%BE%D0%BA%20%D0%BF%D1%80%D0%B8%20%D0%BF%D0%BE%D0%BA%D1%83%D0%BF%D0%BA%D0%B5%20%D0%BA%D0%B2%D0%B0%D1%80%D1%82%D0%B8%D1%80%D1%8B%20%D0%BD%D0%B0%20%D0%9A%D0%B8%D0%BF%D1%80%D0%B5</a>
EdgarRon
Купить круглую стальную трубу оптом и в розницу. Круглые металлические и оцинкованные трубы по низкой цене. Прайс на металлопрокат <a href="http://mosmettorg10.ru/">заглушка для профильной трубы</a>
Juliomed
У нас собственное производство металлических профилей для кровли, фасадов, заборов, поэтому цена на порядок ниже, чем у конкурентов <a href="http://ms-svai.ru/">профильная труба 100х100</a>
StevenAborb
https://medic-dpo.ru/
AndreaJax
Вы можете купить справку в медцентре https://munclinic.ru/ с доставкой по Москве.
TaylorPow
Более 20 лет опыта переводов c немецкого и английский медицинской документации: эпикриз, исследование МРТ, КТ, УЗИ, протокол операции, лабораторные анализы, гистология, молекулярная патология – по всем разделам и специализациям медицины – онкология, урология, гинекология, ортопедия, хирургия и др. Квалифицированный медицинский перевод документов на немецкий язык для лечения за границей и с немецкого после лечения https://medicaltranslate.ru
ThomasGot
Виртуальные номера, телефонные номера, которые напрямую не связаны с телефонной линией или физической SIM-картой, становятся все более популярными среди людей во всем мире. Одной из областей, где их использование приобрело значительный импульс, является приложение для обмена сообщениями, такое как Telegram <a href="https://www.0382.ua/list/480622">одноразовый номер для телеграм</a>
Zacharybem
Построенные дома по индивидуальным проектам – это результат работы наших архитекторов, инженеров – строителей, смежных специалистов и, конечно, наших Заказчиков. Мы всегда стараемся сделать наши дома функциональными, простыми и удобными, чтобы во время эксплуатации наши заказчики вспоминали нас добрым словом <a href="https://www.vbesedki.ru/stati/stroitelnyie_novosti_rossii_all/karkasno-panelnyjj-dom/">https://www.vbesedki.ru/stati/stroitelnyie_novosti_rossii_all/karkasno-panelnyjj-dom/</a>
Juliobam
Условия использования промокода 1xBet можно узнать после его проверки. Для этого в разделе «Витрина промокодов» находится специальное поле, куда следует вставить полученный набор из цифр и букв для получения подробных сведений. Чтобы проверить комбинацию, следует авторизоваться в личном кабинете <a href="https://www.bnbaccess.eu/news/code_promo_1xbet.html">https://www.bnbaccess.eu/news/code_promo_1xbet.html</a>
ArnoldTut
Вы можете купить медсправку в нашем мед центре https://doktora-gerasenko-med.ru/ в Москве без медкомиссий.
JamesEMile
Виртуальные номера телефона стали популярным решением для многих пользователей, особенно в связи с развитием мессенджеров и социальных сетей. В контексте Телеграма, виртуальные номера телефона представляют собой уникальное и удобное решение для обеспечения безопасности и конфиденциальности коммуникации <a href="http://forum.anime.org.ua/bbs/showthread.php?p=117762">временные номера для тг</a>
Williamkaw
Вы можете купить медицинскую справку в мед центре http://cmc-clinic.ru/ в Москве без прохождения врачей.
Michaelmab
В последние десятилетия наблюдается значительный прогресс в области технологий, используемых для создания высококачественных медикаментов. Эти достижения влияют на множество аспектов, включая эффективность процессов, безопасность продуктов и экономическую целесообразность <a href="http://letmefix.lt/index.php?title=%20%D0%92%D0%BB%D0%B8%D1%8F%D0%BD%D0%B8%D0%B5%20%D0%B3%D0%BE%D1%81%D1%83%D0%B4%D0%B0%D1%80%D1%81%D1%82%D0%B2%D0%B5%D0%BD%D0%BD%D1%8B%D1%85%20%D0%BF%D1%80%D0%BE%D0%B3%D1%80%D0%B0%D0%BC%D0%BC%20%D0%BD%D0%B0%20%D1%80%D0%B0%D0%B7%D0%B2%D0%B8%D1%82%D0%B8%D0%B5%20%D0%BF%D0%B8%D1%89%D0%B5%D0%B2%D0%BE%D0%B3%D0%BE%20%D0%BE%D0%B1%D0%BE%D1%80%D1%83%D0%B4%D0%BE%D0%B2%D0%B0%D0%BD%D0%B8%D1%8F%20%D0%B2%20%D0%A0%D0%BE%D1%81%D1%81%D0%B8%D0%B8">http://letmefix.lt/index.php?title=%20%D0%92%D0%BB%D0%B8%D1%8F%D0%BD%D0%B8%D0%B5%20%D0%B3%D0%BE%D1%81%D1%83%D0%B4%D0%B0%D1%80%D1%81%D1%82%D0%B2%D0%B5%D0%BD%D0%BD%D1%8B%D1%85%20%D0%BF%D1%80%D0%BE%D0%B3%D1%80%D0%B0%D0%BC%D0%BC%20%D0%BD%D0%B0%20%D1%80%D0%B0%D0%B7%D0%B2%D0%B8%D1%82%D0%B8%D0%B5%20%D0%BF%D0%B8%D1%89%D0%B5%D0%B2%D0%BE%D0%B3%D0%BE%20%D0%BE%D0%B1%D0%BE%D1%80%D1%83%D0%B4%D0%BE%D0%B2%D0%B0%D0%BD%D0%B8%D1%8F%20%D0%B2%20%D0%A0%D0%BE%D1%81%D1%81%D0%B8%D0%B8</a>
Jamestruri
Технологические инновации в производстве оборудования Современные достижения в области технологий значительно изменили процесс создания сложных систем для медицинской и биологической отраслей <a href="http://jkmulti.vip/bbs/board.php?bo_table=free&wr_id=5738289">http://jkmulti.vip/bbs/board.php?bo_table=free&wr_id=5738289</a>
LarryDaR
The official Melbet website offers a wide line of sports betting, high odds, fast payouts, bonuses for new and regular players <a href="https://dblmmbqwlb.gallery.ru/">https://dblmmbqwlb.gallery.ru/</a>
Stevenascem
Лабораторный компактный V-образный смеситель СФМ-11 подходит для смешивания различных материалов в областях фармацевтики, пищевой, химической, металлургии, керамики, электроники, аккумуляторов и т. д. и способен смешивать два или более сухих порошковых и/или гранулированных материалов <a href="http://amplituda74.ru/">грануляция порошков</a>
Michaellap
Интересная статья про мебель из массива дерева. Все, что нужно знать о мебели из сосны, березы, дуба или бука перед выбором и покупкой <a href="https://taxodrom.ru/ocharovanie-drevesiny-kak-vybrat-idealnyy-komod-iz-dereva-dlya-vashego-interera/">https://taxodrom.ru/ocharovanie-drevesiny-kak-vybrat-idealnyy-komod-iz-dereva-dlya-vashego-interera/</a>
Michaellap
Блистерная упаковка (контурные ячейки) - вид пластиковой упаковки для фармацевтической продукции. Данный тип упаковки имеет множество преимущество: гигиеничность, компактность, защищенность от подделок и механических повреждений, удобство использования и пр <a href="http://oborudpromo.ru/">блистерная машина</a>
Donaldpaicy
Термоформер Multivac R085 предназначен для упаковки непищевых, пищевых и медицинских продуктов в мягкую и в жёсткую плёнку и вакуумирования <a href="http://msmservice.ru/">капсулятор полуавтоматический купить</a>
Howardinged
Компания Ист-Пак приняла участие в выставке Pharmtech & Ingredients 2024 — крупнейшей в России и странах ближнего зарубежья международной выставке оборудования, сырья и технологий для фармацевтического производства <a href="http://oborudpromo.ru/">термоформеры для упаковки продуктов</a>
JuliowoW
В зависимости от размера, толщины листового металла, из которого изготовлены трубы, меняется степень выдерживаемой нагрузки. Больше информации о каждом виде изделия, включая технические характеристики, вы получите, перейдя в карточку товара <a href="http://svai-master78.ru/">металл оптом от производителя цены</a>
Willieadove
Труба профильная, выполненная таким методом, также отличается повышенной пластичностью. Поэтому она подходит для изготовления различных заготовок, применяемых в каркасном строительстве и мебельном производстве <a href="http://odintsovo-beton-zavod.ru">цены металлопрокат</a>
FestivalStarp
Вероятно, вы не ошибаетесь <a href="https://beburishvili-afisha.ru/">beburishvili-afisha.ru</a>
MarvinDat
В каждой игре существуют предметы, которые считаются особенно ценными и редкими. Эти артефакты зачастую становятся основным объектом стремлений игроков, так как могут существенно повлиять на их успех в игровом процессе. Их получение требует значительных усилий, времени или даже удачи, а их использование открывает новые возможности для развития персонажа <a href="http://www.icmms.co.kr/bbs/board.php?bo_table=free&wr_id=1139949">http://www.icmms.co.kr/bbs/board.php?bo_table=free&wr_id=1139949</a>
Patrickabits
Шины являются важной частью любой специальной техники, обеспечивая её проходимость, устойчивость и безопасность на различных типах покрытия. Правильный выбор покрышек влияет на эффективность работы машины и её долговечность, а также помогает избежать возможных поломок и аварийных ситуаций <a href="https://king-wifi.win/index.php?title=%20%D0%A2%D0%B5%D1%85%D0%BD%D0%BE%D0%BB%D0%BE%D0%B3%D0%B8%D0%B8%20%D0%B8%20%D0%B8%D0%BD%D0%BD%D0%BE%D0%B2%D0%B0%D1%86%D0%B8%D0%B8%20%D0%B2%20%D0%BF%D1%80%D0%BE%D0%B8%D0%B7%D0%B2%D0%BE%D0%B4%D1%81%D1%82%D0%B2%D0%B5%20%D0%B3%D1%80%D1%83%D0%B7%D0%BE%D0%B2%D1%8B%D1%85%20%D0%BA%D0%BE%D0%BB%D0%B5%D1%81">https://king-wifi.win/index.php?title=%20%D0%A2%D0%B5%D1%85%D0%BD%D0%BE%D0%BB%D0%BE%D0%B3%D0%B8%D0%B8%20%D0%B8%20%D0%B8%D0%BD%D0%BD%D0%BE%D0%B2%D0%B0%D1%86%D0%B8%D0%B8%20%D0%B2%20%D0%BF%D1%80%D0%BE%D0%B8%D0%B7%D0%B2%D0%BE%D0%B4%D1%81%D1%82%D0%B2%D0%B5%20%D0%B3%D1%80%D1%83%D0%B7%D0%BE%D0%B2%D1%8B%D1%85%20%D0%BA%D0%BE%D0%BB%D0%B5%D1%81</a>
ThomasMoock
Обратите внимание на гинеколога в Варшаве, Анастасию Юрьевну. Это врач с огромным опытом, которая помогает пациенткам в самых разных ситуациях. Она занимается гинекологическими осмотрами, ультразвуковой диагностикой, лечением воспалительных процессов и консультациями по вопросам планирования семьи <a href="http://xmariox.webd.pl/viewtopic.php?f=120&t=219144&sid=8d937e43b0c85a8eb450ea761353eb6b">http://xmariox.webd.pl/viewtopic.php?f=120&t=219144&sid=8d937e43b0c85a8eb450ea761353eb6b</a>
JimmyAcawl
Mostbet, Turkiye'deki kullan?c?lar icin genis bir bahis ve casino oyunlar? secenegi sunan populer bir platformdur https://hurifo.org/
crypto7Jax
Dogecoin may have started as a joke, but it’s a real investment for many now. [url=https://t.me/cryptonetlake]https://t.me/cryptonetlake[/url]
CurtisAvaix
https://mayaschool.ru
EdwardNargy
Оптимизируйте работу своего бизнеса с надежным и мощным VPS-хостингом. Аренда выделенных виртуальных серверов с гарантированной производительностью и надежностью <a href="https://1linesoft.ru/">аренда windows vps сервера</a>
crypto7Jax
Learning about crypto security is so important for new investors. [url=https://t.me/cryptonetlake]https://t.me/cryptonetlake[/url]
Ralphgooli
Инверторы играют ключевую роль в системах солнечной энергетики, позволяя преобразовывать постоянный ток, генерируемый солнечными панелями, в переменный, который может быть использован для питания бытовых приборов, освещения и других потребностей дома, офиса или производственного объекта. Это делает их незаменимым компонентом для создания эффективных и автономных систем электроснабжения <a href="https://solar.biz.ua/invertory-ibp/gibridnyj-invertor-ibp-3000vt-24v-mppt-na-3-kvt-ismppt-bf-3000-axioma-energy.html">https://solar.biz.ua/invertory-ibp/gibridnyj-invertor-ibp-3000vt-24v-mppt-na-3-kvt-ismppt-bf-3000-axioma-energy.html</a>
AgustinNub
Для веб-проектов, работающих на VPS, обеспечивается высокая скорость загрузки страниц, что является ключевым фактором для улучшения пользовательского опыта и SEO-показателей сайта <a href="https://netfaq.ru/">купить доменное имя для сайта</a>
KevinTug
Инверторы играют ключевую роль в системах солнечной энергетики, позволяя преобразовывать постоянный ток, генерируемый солнечными панелями, в переменный <a href="https://solar.biz.ua/invertory-ibp/">https://solar.biz.ua/invertory-ibp/</a>
crypto7Jax
It’s fascinating how different each cryptocurrency’s purpose can be. [url=https://t.me/cryptonetlake]https://t.me/cryptonetlake[/url]
JamesGlaks
Гимнастика для спины, занятия Красивая осанка, Здоровая спина, Йога, Гамаки, Стретчинг, Шпагат, Пилатес, Zumba, Восточные танцы, массаж в Студии <a href="https://dusash-omsk.ru/">фитнес клуб метро беляево</a>
Zacharycip
Просторный тренажерный зал. Fitness Беляево оборудован 150+ единицами современных тренажеров. Самые популярные из них представлены в нескольких экземплярах, чтобы вы не тратили время на ожидание в очереди <a href="https://fitness-lubercy.ru/">фитнес зал беляево</a>
FedukStarp
Спасибо за такую точку зрения. <a href="https://fakel-nsk-afisha.ru/">fakel-nsk-afisha.ru</a>
IrwinPep
Высокотехнологичные видеостойки от производителя. На нашем сайте представлен широкий ассортимент различных моделей и с разными размерами экрана <a href="https://vk.com/biznareklama">Рекламная видеостойка</a>
Charlesnum
Кто может порекомендовать обменник с хорошими условиями для обмена криптовалюты? Хочу, чтобы курс был честный и не было скрытых комиссий <a href="https://zoo-help.at.ua/forum/12-5427-1">https://zoo-help.at.ua/forum/12-5427-1</a>
Davidtax
Наша компания предоставляет услуги эвакуации автомобилей в Москве и Московской области круглосуточно. Мы гарантируем оперативную помощь, доступные цены и профессиональный подход. Вызвать эвакуатор вы можете по телефону или оформить заявку на нашем сайте в любой момент <a href="https://autoru24.ru/">эвакуатор цена</a>
Frankvef
Используйте бесплатные шаблоны резюме для устройства на работу. Пустые бланки резюме для устройства на работу представлены в 35 вариантах оформления. Шаблоны представлены в формате PDF, используйте для работы с файлами PDF-редакторы <a href="https://vkyrse.com/kak-sostavit-rezyume-i-ustroitsya-na-rabotu-poshagovoe-rukovodstvo">https://vkyrse.com/kak-sostavit-rezyume-i-ustroitsya-na-rabotu-poshagovoe-rukovodstvo</a>
PhilipKip
Каждая площадка предлагает уникальный набор функций, которые могут включать разнообразные форматы, бонусные программы и техническую поддержку. Однако не все из них способны соответствовать высоким стандартам пользователей <a href="http://www.thedreammate.com/home/bbs/board.php?bo_table=free&wr_id=2022670">http://www.thedreammate.com/home/bbs/board.php?bo_table=free&wr_id=2022670</a>
Davideleva
Babu88: Online casino and bookmaker for sports betting in Bangladesh <a href="https://mayaiswithyou.com/">babu88 app login</a>
SamuelFaw
Отслеживание курсов валют — это важный инструмент для грамотного управления финансами как в личной жизни, так и в бизнесе. Знание актуального курса позволяет выбрать наиболее выгодное время для обмена валюты, что особенно полезно при подготовке к поездкам за границу или международным переводам <a href="http://my-smsfinance.ru/">втб курс доллара</a>
PhilipKip
Мы не просто предоставляем цифры. На сайте вы найдете аналитические материалы, которые помогут лучше понять динамику валютного рынка, выявить тренды и спланировать свои финансовые шаги <a href="http://new-yoomoney.ru/">камкомбанк курс валют на сегодня</a>
Richardsew
Передвижной компрессор — это универсальное решение для сжатия воздуха в разных условиях. Мобильные компрессоры, включая электрические модели, используются в самых разных сферах: от строительства до производства. Для удобства эксплуатации существуют передвижные компрессорные установки, воздушные компрессоры передвижные и даже воздушные компрессоры на прицепе. Эти устройства бывают как поршневыми, так и более мощными промышленными вариантами. Важно, что передвижной компрессор бывает с различными характеристиками, включая мощность, тип привода и производительность, что позволяет подобрать модель для любых нужд <a href="http://stroy-compressor.ru/">мощность компрессора передвижного</a>
DanielMoome
Винтовой компрессор – это эффективное оборудование для сжатия воздуха, который применяется в различных сферах, от гаража до промышленности. Существует множество вариантов, включая бюджетные винтовые компрессоры, винтовые компрессоры для пневмоинструментов, а также специализированные модели для покраски автомобилей и бытового использования. Винтовые компрессоры бывают воздушного типа, сжатого воздуха и электрические, а также могут быть как автономными, так и без двигателя. В поисках винтового компрессора, будь то для дома, гаража или производственного процесса, можно найти как недорогие, так и более дорогие модели в магазинах, таких как винтовые компрессоры в Москве, Екатеринбурге, Барнауле и других городах. Важно помнить, что выбор зависит от задач: для больших производств подойдут высокопроизводительные воздушные винтовые компрессоры, а для дома – компактные и недорогие винтовые модели <a href="http://compressprom.ru/">компрессор винтовой екатеринбург</a>
Haywoodforce
Наш сайт для мониторинга курсов валют — это ваш надежный помощник в финансовом планировании. Каждый день предоставляем точную и актуальную информацию о курсах валют, позволяя пользователям принимать обоснованные решения <a href="http://card2money.ru/">курс валют банки</a>
PhillipRit
MyTonWallet is the ultimate wallet for managing your TON (The Open Network) assets, offering a comprehensive range of features that set it apart from other wallets in the crypto space. Whether you're new to cryptocurrencies or an experienced user, MyTonWallet provides all the tools you need to securely store, manage, and interact with your TON tokens, NFTs, and decentralized applications (dApps) <a href="https://mytonwallet.en.uptodown.com/android">MyTonWallet wallet</a>
KennethGesug
<a href="https://t.me/vladislavkocherizhkin/37">https://t.me/vladislavkocherizhkin/37</a>
WilburVaf
Спиральный компрессор — это эффективное устройство, которое используется для сжатия воздуха в различных системах. Герметичный спиральный компрессор часто используется в промышленных приложениях, где необходимы компактность и надежность. Такие компрессоры обеспечивают отличную герметичность и минимальный уровень утечек, что делает их идеальными для использования в самых разных условиях <a href="http://compressor-tomsk.ru/">спиральный безмасляный компрессор</a>
Josephnam
Mobile applications have become an integral part of our daily lives, offering a wide range of tools to simplify tasks, entertain, and enhance productivity. As technology continues to evolve, more apps are being designed to cater to different needs, from gaming to communication and beyond. These applications offer convenience, and with the right features, they can become indispensable on our smartphones babu88 download <a href="http://edengardenbarandgrill.com/forum/in-neque-arcu-vulputate-vitae/7483-downloading-and-using-bluewallet-apk-for-fast-bitcoin-payments#7484">http://edengardenbarandgrill.com/forum/in-neque-arcu-vulputate-vitae/7483-downloading-and-using-bluewallet-apk-for-fast-bitcoin-payments#7484</a>
WilliamCon
Цилиндрическая камера видеонаблюдения является одним из наиболее эффективных решений для наружного мониторинга и обеспечения безопасности <a href="https://ego-yuriie.ru/videoregistrator/">https://ego-yuriie.ru/videoregistrator/</a>
ChesterSap
Межкомнатные раздвижные перегородки на заказ. Купить с доставкой по России. Действуют акции, системы скидок и специальных предложений <a href="http://loft-zonirovanie.ru">гардеробная система на заказ недорого</a>
Jaimecaw
Микрозаймы выдают МФО – микрофинансовые организации. Их преимущество для бизнеса – в более простом порядке получения денег и быстром сроке рассмотрения заявки <a href="https://polytech-business.ru/">займы с ип</a>
RobertJal
Чаще всего стеклянные перегородки можно увидеть в деловых помещениях – пространствах лаконичных, функциональных и, прежде всего, с рабочей атмосферой <a href="http://loftwood-design.ru/">гардеробная система стекло</a>
Davidlet
Труба профильная — это вид современного строительного металлопроката, получаемый профилированием. Они имеют сечение, отличное от круглого. Наиболее распространены квадратные и прямоугольные <a href="http://allshveller.ru/">поставщики профильной трубы москва</a>
Bernardtog
Самые востребованные среди них – прямоугольные и квадратные изделия. Профильные трубы 40х40 широко используются во всех сферах: тяжелой и легкой промышленности <a href="http://odintsovo-beton-zavod.ru">трубы профильные стальные</a>
JordanWrami
To avoid such ridiculous situations and not get into trouble, we recommend that you consider buying a smoking cap in our online store. Here you can find thimbles of various shapes and designs, made of the best materials <a href="http://www.bisound.com/forum/showthread.php?p=1085830">https://napas420.com/ru/bong-dlya-kureniya/</a>
JulianEress
Homemade bubblers from plastic bottles are an incredibly simple and versatile solution to relax and enjoy a head-scratching potion <a href="https://kamianets.com/ru/article/110460-zachem-nuzhny-napasy-dlya-kureniya">https://napas420.com/ru/naperstki-dlya-kureniya/</a>
Titusbot
Pegasus check-in closes 45 minutes before departure for flights within Turkey and 60 minutes before departure for international flights <a href="https://pegasus-avia1.ru/">Pegasus Airlines</a>
BruceeFfed
The first thing you need to know. Fonbet promo codes are coded access through which bonuses become available to players. Visually, a bonus code is a combination or combination of symbols, which is the very same access code to some advantage <a href="https://tj-service.ru/news/?fonbet___besplatnuy_promokod_pri_registracii.html">https://tj-service.ru/news/?fonbet___besplatnuy_promokod_pri_registracii.html</a>
Jamessumew
Актуальное зеркало Vavada casino 2025. К сожалению, законы в некоторых регионах могут привести к блокировке даже официальных и популярных международных казино <a href="https://quotedapps.com/">вавада зеркало</a>
Harrytug
http://lordfilm-e.net
AltonMig
СЗЗ (санитарно защитная зона) для промышленных предприятий в Москве и Московской области. Что нужно учесть при разработке проекта СЗЗ и на этапе согласования в органах надзора для обеспечения законной деятельности объекта НВОС https://vc.ru/u/3791103-infa-v-dele/1719864-chto-takoe-szz-i-kak-razrabotat-proekt-sanitarnoi-zony
Eugenenop
The 1xBet promo code 2025: 1XNEW25. Use to register a new member, get a sports bonus 100% up to €130 and casino bonus €1950 + 150 free spins. Use the bonus code when registering and you are guaranteed to receive a 2025 welcome bonus from 1xBet. The 1xBet bookmaker has proven itself to be time-tested, it has high odds for sports betting, and a huge number of slots in the cauldron section, there are also roulette, poker, and fast online games like Aviator <a href="https://cascadeclimbers.com/content/pgs/1xbet-promo-code_112.html">1xbet welcome bonus promo code</a>
ThomasZes
Преимущества Arkada Казино. Щедрые бонусы: До 500% на первый депозит и сотни бесплатных фриспинов. Огромный выбор игр: Слоты, настольные игры, live-казино <a href="https://t.me/s/arkada_casino_online">casino аркада</a>
Phillipknoca
Promo codes are a useful tool to get enhanced bonuses and privileges for free bets. 1xBet is one of the platforms that actively uses codes to attract new players and provide them with bonuses this way <a href="https://fondrgs.ru/wp-includes/pages/promokodu_dlya_19.html">https://justinekeptcalmandwentvegan.com/wp-content/pages/code_promo_melbet-bonus_de_bienvenue.html</a>
RodneyTek
Enfrente adversarios epicos e conquiste a gloria na Arena dos Campeoes <a href="https://lusa-gaming.pt/contato/">www.lusa-gaming.pt</a>
Raymonddrolo
Во все времена на рынке сантехники чугунные ванны пользовались особой актуальностью. Данный важный элемент ванной комнаты имеет огромное количество преимуществ <a href="http://stroybud.com/kak-vyibrat-dushevuyu-kabinu-v-malenkuyu-vannuyu/">http://stroybud.com/kak-vyibrat-dushevuyu-kabinu-v-malenkuyu-vannuyu/</a>
Michaelzes
Tell the world about your experience to help others make the right buying decision. We publish authentic reviews to ensure everyone can access valuable information on a definite company <a href="https://vodkakazino.pro">бонус за регистрацию водка казино</a>
CharlesSor
Ik vond het geweldig om te lezen over de mogelijkheid om Telegram didvirtualnumbers.com/nl/how-to-register-in-telegram/ te gebruiken zonder een simkaart. Ik had geen toegang tot een simkaart en wilde Telegram toch gebruiken. Dankzij DID Virtual Numbers kreeg ik snel een virtueel nummer en was het registratieproces erg eenvoudig <a href="https://www.pomsinadelaide.com/topic/47739-stapsgewijze-gids-voor-het-registreren-in-telegram/">https://www.pomsinadelaide.com/topic/47739-stapsgewijze-gids-voor-het-registreren-in-telegram/</a>
RussellMOUME
Имплантация – современный метод протезирования зубов, при котором возможно полноценное восстановление целостности зубного ряда. При дентальной имплантации <a href="https://smiledenta.ru">имплантация верхних зубов</a>
BrandonEvace
Преимущества современных цифровых решений Технологические платформы становятся важной частью повседневной жизни, предлагая пользователям удобство и широкий функционал <a href="http://longlive.com/node/4011">http://longlive.com/node/4011</a>
HermanVox
Dit artikel gaf me precies de informatie die ik nodig had. Dankzij DID Virtual Numbers kon ik een virtueel nummer verkrijgen en me registreren op mijn computer. Het proces was snel en het voelde veilig, omdat ik mijn persoonlijke gegevens niet hoefde in te voeren <a href="https://www.ftt2.com/forum?mingleforumaction=viewtopic&t=1333#postid-2331">https://www.ftt2.com/forum?mingleforumaction=viewtopic&t=1333#postid-2331</a>
DesmondGeopy
Новая песня для тех, кто привык добиваться своего! Не смотри на других, забудь оправдания — это твой путь, и он начинается с <a href="https://band.link/IsPbO">Projektx_Punk</a>
DanielFeavy
The cryptocurrency market is fraught with scams, hacks, and fraudulent schemes. By performing an AML check, you can identify potentially risky assets and avoid falling victim to scams <a href="https://crystalcompliance.hashnode.dev/how-to-conduct-a-free-aml-check-on-your-avalanche-assets">AVAX AML check</a>
FrankKew
<a href="https://sms-man.com/cn">https://sms-man.com/cn</a>
BlakeOreni
https://forum.azs-lukoil.ru/threads/kraken-ssylki-2024-kak-zajti-na-kraken-v-2024-kraken-aktualnye-ssylki-zerkala-i-ispolzovanie-tor.1182/
BryancevStarp
Возможно, вы правы <a href="https://butirkaconcert.ru/">butirkaconcert.ru</a>
Timothybug
In the fast-paced world of blockchain development, integrating reliable APIs is crucial for building efficient decentralized applications (dApps) <a href="https://vocal.media/trader/using-arbitrum-api-in-development">https://vocal.media/trader/using-arbitrum-api-in-development</a>
RichardMat
Steam aauthenticator is a option of two-step authentication on steam. It provides additional step privacy your nicknames and passwords. If this option is enabled, Steam Aauthenticator asks you for one-time passcode every time , when you login to Steam on a unfamiliar device <a href="https://steamdesktopauthenticator.me/">steam mobile authenticator</a>
Stevennob
This page is dedicated for ASF configuration. It serves as a complete documentation of config directory, allowing you to tune ASF to your needs <a href="https://steamauthenticator.ru/">steam guard authenticator скачать</a>
JefferyFum
Somebody was posting that setting up the authenticator works on 1.0.11, and then upgrade to 1.0.13 for confirmations to work. Idk, something like that, haven't tried it <a href="https://steamdesktopauthenticator.io/">как включить steam mobile authenticator</a>
CharlesJailt
The Steam Guard Mobile Authenticator is a feature of the Steam Mobile App that provides an additional level of security to your Steam аccount <a href="https://steamauthenticatordesktop.com/">steam mobile authenticator</a>
FrankmibiA
Instantly connects you to random people worldwide, similar to the Omegle experience. You could meet someone from across the globe or right around the <a href="https://rt.totalchat.ru">видео чат секс</a>
JeremyLomma
IF you lost your maFiles OR lost your encryption key, go here and click "Remove Authenticator" then enter your revocation code that you wrote down when you first added your account to SDA <a href="https://authenticatorsteam.com/">скачать sda steam</a>
http://Boyarka-inform.com/
After I initially commented I seem to have clicked the -Notify me when new comments are added- checkbox and from now on every time a comment is added I receive four emails with the same comment. Perhaps tyere is ann easy method you can remove me from that service? Thank you! http://Boyarka-inform.com/
RamiroDeext
After logging into Mostbet, you can take advantage of welcome bonuses, deposit bonuses, and special promotions to boost your chances of winning <a href="https://mostbetapk.com/">mostbet download</a>
Davidwah
Your Steam Mobile app can be used to authenticate multiple Steam accounts. From the blue drop down on the Steam Guard tab, select an account or add a new one <a href="https://steamauthenticator.ru/">steam move authenticator</a>
Eddieboova
A command line utility for setting up and using Steam Mobile Authenticator (AKA Steam 2FA). It can also be used to respond to trade, market, and any other <a href="https://steamdesktopauthenticator.me/">steam move authenticator</a>
CharlesNeoms
Главное отличие автоматизированного тестирования от ручного состоит в способе выполнения: в первом случае тесты запускаются с помощью инструментов автоматизации, во втором — все действия выполняются тестировщиком вручную https://vc.ru/u/3791103-infa-v-dele/1733597-avtotesty-instrumenty-vidy-i-smysl-avtomatizacii-qa
CurtisPoepe
The Steam Guard Mobile Authenticator is a feature of the Steam Mobile App that provides an additional level of security to your Steam account <a href="https://steamdesktopauthenticator.io/">steam desktop authenticator как пользоваться</a>
KevinLes
Run Steam Desktop Authenticator.exe and click the button to set up a new account. Login to Steam and follow the instructions to set it up. Note: you still <a href="https://steamauthenticatordesktop.com/">steam guard mobile authenticator как включить</a>
JerryAcund
SDA and maFile are related to account management on the Steam platform. SDA allows you to generate Steam Guard security codes on your computer <a href="https://authenticatorsteam.com/">sda steam</a>
JerryAcund
SDA allows you to generate Steam Guard security codes on your computer. SDA and maFile are related to account management on the Steam platform <a href="https://authenticatorsteam.com/">add steam authenticator</a>
FrancisTig
Бесплатный доступ к онлайн курсам, тренингам и книгам. Большой выбор образовательных курсов. Скачивайте бесплатно уже сейчас https://piratehub.site
KevinNuh
1XBET promo code 2025: 1XMAX25 - Use bonus code get for VIP bonuses - up to €19502 + 150 free spins on casino and 100% up to €130 on sportsbook! To get your Free Bet, new customers can register with 1xbet for free, and enter the promo code 1x. Take a look at our site banners for the latest 1xBet promo codes and information about the brand’s 100% first deposit bonus where you live. New players can enjoy an exclusive deposit bonus when they sign up at 1xBet. See our site banners for the latest welcome deals at 1xBet for your region <a href="https://manorhousedentalpractice.co.uk/articles/1xbet_new_account_promo_code.html">promo code for 1xbet pakistan today</a>
AntoineSmepe
Existe una competencia muy alta en la industria de los juegos de azar virtuales y las apuestas deportivas interactivas en la actualidad <a href="https://entrenasalud.es/pag/?1xbet_registration_code.html">https://entrenasalud.es/pag/?1xbet_registration_code.html</a>
AntoineSmepe
La linea entre videojuego y juego de apuestas es realmente muy delgada <a href="https://aprenderlinguagem.org.br/wp-content/pgs/1xbet_codigo_promocional_ao_registrar.html">https://aprenderlinguagem.org.br/wp-content/pgs/1xbet_codigo_promocional_ao_registrar.html</a>
AntoineSmepe
Melbet bookmaker offers new customers bonuses: for registration with a promo code, for the first account replenishment (first deposit bonus), freebet bonus for free bet, welcome bonus for new players <a href="https://metchelstroy.ru/img/pgs/1melbet_promokod_bonus_za_registraciu.html">https://metchelstroy.ru/img/pgs/1melbet_promokod_bonus_za_registraciu.html</a>
Brandonenuck
Pour profiter de ce bonus exceptionnel, il vous suffit d’effectuer votre premier depot. Celui-ci vous donne droit a un bonus de 100% du montant depose, jusqu’a un maximum de $130, ou l’equivalent dans votre devise <a href="https://depannage-serrurerie-annecy.fr/pags/code_de_promotion_1xbet.html">1xbet apk sn</a>
Julianskawl
Sleep disorders in autism are a common symptom that significantly impact the quality of life for both the child and their family. The causes of insomnia in autistic children are based on the peculiarities of how their nervous system functions <a href="https://www.autism-mmc.com/publications/answer/">https://www.autism-mmc.com/publications/answer/</a>
KennethElabe
Nowadays, international communication is of great importance in both personal and business life. Especially in a country like South Korea, which is important in terms of technology and trade <a href="https://pantheonuk.org/optimize-your-connectivity-with-a-virtual-number-solution/">rent SMS virtual number</a>
KennethElabe
While Telegram requires you to sign up with a phone number, this number does not have to be personal. By purchasing a number for Telegram, you can provide a great advantage, especially for users who are concerned about privacy <a href="https://tfipost.com/2024/09/virtual-numbers-in-the-uae-a-convenient-solution-for-secure-communication/">UAE virtual SMS number</a>
JudithErype
We offer to your attention huge range of quality used autos, checked by our specialists. For more information, follow the link [url=https://auto-permyak.ru/]купить машину [/url] Our goal is to help you find the perfect auto at a attractive price.
JamesMetty
В нашем Центре техосмотра на Московском шоссе, 13 в Санкт-Петербурге вы можете пройти техосмотр вашего автомобиля с гарантией качества и быстроты обслуживания. Мы предлагаем полный спектр услуг, чтобы обеспечить безопасность и соответствие вашего транспортного средства всем необходимым стандартам <a href="https://yandex.ru/search?text=%D0%A2%D0%B5%D1%85%D0%BE%D1%81%D0%BC%D0%BE%D1%82%D1%80&oid=b%3A11324347330&lr=11209">быстрое получение диагностической карты</a>
MichaelIsoto
When it comes to active recreation near the water, many people pay attention to the little things that make this process more convenient and enjoyable <a href="https://meblevozka.in.ua/grindery-dlya-izmelcheniya-travy-i-tabachnyx-smesej-v-napas420/">https://meblevozka.in.ua/grindery-dlya-izmelcheniya-travy-i-tabachnyx-smesej-v-napas420/</a>
Rogersmuct
We encourage you to explore our handpicked selection of the finest online casino sites, catering to players from every corner of the globe <a href="https://danludangambler.com/">данлудан</a>
RachelEa
We specialize in producing high-quality packaging for all industries: from cosmetic to industrial. For more information, follow the link [url=https://pack-inn.ru/]лента двухсторонняя [/url] Our products include plastic containers, films and more.
Alfredcotte
Если вы только планируете поездку в Таиланд и на Пхукет, загляните на <a href="http://gazelperm.ru/content/pages/natsional-nyj-park-ko-chang.html">phuketescape.com</a> — там собрана базовая информация для начинающих путешественников что посмотреть, куда съездить.
MatthewFeeta
Нашёл недавно интересный путеводитель по Парижу и Франции – <a href="http://afandi-shop.ru/wp-content/pgs/parizhskoe-metro-insajderskij-gid.html">parisgid.ru</a>. Там есть готовые маршруты, идеи, обзоры достопримечательностей и советы где поесть.
Richardknilt
Бесплатные фриспины за регистрацию в казино - подборка актуальных предложений. Новые фриспины без депозита 2025 года на <a href="https://droptopsite1.ru/">https://droptopsite1.ru/</a>
MatthewCorge
Займ на карту без отказа — это быстрое и удобное решение для тех, кто нуждается в финансовой помощи: простая онлайн-заявка, минимальные требования к заемщику и мгновенное одобрение, что позволяет получить необходимую сумму практически незамедлительно, а также возможность быстро погасить задолженность, делая процесс максимально комфортным и прозрачным для каждого <a href="https://vc.ru/money/1745222-kak-poluchit-zaim-na-kartu-bez-otkaza-top-17-mfo-v-2025-godu">займ 100 одобрение</a>
SheriSr
Welcome to our resource, where you will find everything you need for successful mining! More detailed information at the link [url=https://mini-miner.ru/]майнинг оборудование что это такое [/url] We offer huge range of high-quality equipment, which will help you mine digital assets as efficiently as possible.
Robertunush
Заказать изготовление по индивидуальному дизайну или купть памятник по выгодной цене Вы можете в нашей Гранитной мастерской <a href="https://nisp.ru">Бесплатный памятник для каждого</a>
Williamkib
Гранитная мастерская памятников – это предприятие по изготовлению памятников на могилу из натурального камня. <a href="https://talkingstone.ru">слушать онлайн бесплатно</a>
Julieot
Welcome to our resource, where you will find a widest range of gabions for any needs! For more information, follow the link [url=https://gabi-one.ru/]производство габионов [/url] We offer to your attention high-quality gabions that are ideal for slope reinforcement and erosion protection.
WilliamDaugh
На сайте в вашем распоряжении бесплатные фильмы в онлайне. Вам не придется переживать, если вы не успели познакомиться с недавно вышедшими фильмом-новинкой. Для тех, кто не может оставаться в стороне от жизни кинематографа, должен быть на острие всех его событий, предлагаются смотреть фильмы в HD 1080 <a href="https://lordfilms-2.com/">фильмы 2025</a>
ClydeWof
Букмекерская контора 1Win – самая популярная платформа для онлайн ставок на спорт и казино в России. 1Вин – это легальный официальный сайт с лицензией, которые всегда выводит выигрыши. Чтобы начать делать ставки и играть на деньги, необходимо зарегистрироваться <a href="http://edengardenbarandgrill.com/forum/welcome-mat/7527-1#7528">http://edengardenbarandgrill.com/forum/welcome-mat/7527-1#7528</a>
JoshuaAnolf
Игроки могут осуществлять ставки в 1вин на самые различные события, на десятки видов спорта а также киберспорт и многое другое. Инфраструктура проекта развита <a href="https://valetinowiki.racing/index.php?title=%20%D0%9F%D1%80%D0%BE%D0%B1%D0%BB%D0%B5%D0%BC%D1%8B%20%D1%81%20%D0%B2%D1%85%D0%BE%D0%B4%D0%BE%D0%BC%20%D0%B2%201win:%20%D0%BA%D0%B0%D0%BA%20%D0%B8%D1%85%20%D1%80%D0%B5%D1%88%D0%B8%D1%82%D1%8C">https://valetinowiki.racing/index.php?title=%20%D0%9F%D1%80%D0%BE%D0%B1%D0%BB%D0%B5%D0%BC%D1%8B%20%D1%81%20%D0%B2%D1%85%D0%BE%D0%B4%D0%BE%D0%BC%20%D0%B2%201win:%20%D0%BA%D0%B0%D0%BA%20%D0%B8%D1%85%20%D1%80%D0%B5%D1%88%D0%B8%D1%82%D1%8C</a>
Jameswrach
Авторитетный журнал для современных женщин о трендах моды, красоте, заботе о себе, путешествиях, культуре и интерьерных решениях от экспертов <a href="https://prostitutki-kalugi.ru/">вызвать проститутку калуга</a>
Kennethreowl
Виниловый пол – это современное напольное покрытие, которое стремительно набирает популярность благодаря своим уникальным свойствам и широким возможностям дизайна <a href="https://gp.by/novosti/kaleidoscope/news292747.html">https://gp.by/novosti/kaleidoscope/news292747.html</a>
WilliamZesia
All of our shelves are handcrafted and make in Deer Park, NY. The process of making your shelf starts from the moment you place an order You can create your own shelf Shop now <a href="https://mymomsbookshelf.com/">designer wall shelf</a>
Robertref
Оригинальные детали от проверенных производителей обеспечивают максимальную точность и стабильность работы. Кроме того, они обычно проходят строгий контроль качества, что снижает вероятность неисправностей <a href="https://funsilo.date/index.php?title=%20%D0%9E%D0%B1%D0%B7%D0%BE%D1%80%20%D1%80%D1%8B%D0%BD%D0%BA%D0%B0%20%D0%B7%D0%B0%D0%BF%D1%87%D0%B0%D1%81%D1%82%D0%B5%D0%B9%20%D0%B4%D0%BB%D1%8F%20%D1%81%D1%82%D0%B0%D0%BD%D0%BA%D0%BE%D0%B2%20%D0%BF%D0%BE%20%D0%BC%D0%B5%D1%82%D0%B0%D0%BB%D0%BB%D0%BE%D0%BE%D0%B1%D1%80%D0%B0%D0%B1%D0%BE%D1%82%D0%BA%D0%B5">https://funsilo.date/index.php?title=%20%D0%9E%D0%B1%D0%B7%D0%BE%D1%80%20%D1%80%D1%8B%D0%BD%D0%BA%D0%B0%20%D0%B7%D0%B0%D0%BF%D1%87%D0%B0%D1%81%D1%82%D0%B5%D0%B9%20%D0%B4%D0%BB%D1%8F%20%D1%81%D1%82%D0%B0%D0%BD%D0%BA%D0%BE%D0%B2%20%D0%BF%D0%BE%20%D0%BC%D0%B5%D1%82%D0%B0%D0%BB%D0%BB%D0%BE%D0%BE%D0%B1%D1%80%D0%B0%D0%B1%D0%BE%D1%82%D0%BA%D0%B5</a>
DarrenLon
Польский виртуальный номер – это телефонный номер, который не привязан к физической SIM-карте или мобильному устройству. Вместо этого, он работает через интернет, что делает его доступным практически из любой точки мира <a href="https://avtoping.ru/kak-kupit-virtualnyj-nomer-dlya-whatsapp/">виртуальный номер для ватсап</a>
Michaellaura
Играем в Трикс казино официальный сайт онлайн на деньги! Регистрация и вход в Trix казино через рабочее зеркало. Бонусы и акции для новых и постоянных <a href="https://trix-66.fun">трикс казино</a>
Scottgom
Виртуальный номер телефона даёт возможность подключать любое количество номеров и разговаривать с любого устройства, принимать звонки в офисе или дома <a href="https://www.c-inform.info/news/id/110929">виртуальный номер для тг</a>
Ronalddem
Дома из бревна вообще выглядят очень круто! Я лично давно мечтаю о чем-то подобном, но, к сожалению, пока что даже участка под такой дом у меня нет <a href="https://ru.gorodwiki.ru/peterburg/izba-776157-otzyvy">https://ru.gorodwiki.ru/peterburg/izba-776157-otzyvy</a>
Michaelspodo
Portugal has long been a country known for producing exceptional talent in the world of sports. With a rich history in football, many athletes from this nation have achieved international fame through their incredible skills and accomplishments <a href="https://king-wifi.win/index.php?title=%20The%20Secret%20to%20The%20PT%20Gamers%E2%80%99%20Success%20in%20Esports">https://king-wifi.win/index.php?title=%20The%20Secret%20to%20The%20PT%20Gamers%E2%80%99%20Success%20in%20Esports</a>
BobbyBrups
Продажа табака для кальяна. На сайте вы можете зарезервировать выбранный табак и забрать в магазине <a href="https://shyker.com.ua/yak-vibrati-idealnij-kovpak-dlya-kurinnya-poradi-novachkam/">https://shyker.com.ua/yak-vibrati-idealnij-kovpak-dlya-kurinnya-poradi-novachkam/</a>
GregoryEmome
Широкий ассортимент пиломатериалов собственного производства. В каталоге представлено все необходимое для строительства, ремонта и отделки <a href="https://prof-parket43.ru/">пиломатериалы в москве</a>
Jasonbit
Когда я зашёл на этот мир, впечатление было таким, будто я переступил грань реальности. Здесь каждый спин — это не просто шанс, а эмоция, которую ты проживаешь с каждым кликом. Дизайн интуитивен, словно легкое прикосновение направляет тебя от момента к моменту. Транзакции, будь то пополнения или выплаты, проходят быстро, как поток воды, и это удивляет. А служба помощи всегда рядом, как верный помощник, который никогда не разочарует. Для меня [url=https://selector-casino-igrat.tech/]Селектор онлайн[/url] стал пространством, где азарт и искусство сплетаются. Здесь каждый момент — это часть пути, которую хочется переживать снова и снова.
LeroyHab
https://odnazhdyvskazke-tv.ru
MichealWef
1Win является лучшим букмекером и казино в 2024 году. В интернете множество площадок, в которых есть ставки на спорт, но лидирующую позицию занимает 1Вин. Для пользователей гарантированы честные условия, высокие коэффициенты и качественное обслуживание. На официальном сайте 1Вин доступны быстрые выплаты, кэшбек до 30% и супер бонус в размере 500% <a href="http://www.ehion.com/~ameba/dokuwiki/doku.php?id=%20%D0%9E%D0%B1%D0%B7%D0%BE%D1%80%20live-%D0%BA%D0%B0%D0%B7%D0%B8%D0%BD%D0%BE%201%D0%92%D0%B8%D0%BD:%20%D0%98%D0%B3%D1%80%D1%8B%20%D1%81%20%D1%80%D0%B5%D0%B0%D0%BB%D1%8C%D0%BD%D1%8B%D0%BC%D0%B8%20%D0%BA%D1%80%D1%83%D0%BF%D1%8C%D0%B5">http://www.ehion.com/~ameba/dokuwiki/doku.php?id=%20%D0%9E%D0%B1%D0%B7%D0%BE%D1%80%20live-%D0%BA%D0%B0%D0%B7%D0%B8%D0%BD%D0%BE%201%D0%92%D0%B8%D0%BD:%20%D0%98%D0%B3%D1%80%D1%8B%20%D1%81%20%D1%80%D0%B5%D0%B0%D0%BB%D1%8C%D0%BD%D1%8B%D0%BC%D0%B8%20%D0%BA%D1%80%D1%83%D0%BF%D1%8C%D0%B5</a>
Haroldlayen
В основе сюжета лежит необычная концепция двух миров — сказочного и реального. Всё начинается в волшебной стране, где Злая Королева, устав от счастья и благополучия своих соседей, накладывает страшное проклятие, вырвав героев из их привычных сказочных миров и закинув их в место, о котором они и не мечтали https://odnazhdyvskazke-tv.ru
WalterTaf
Как спилить дерево на участке в нужном направлении падения с помощью бензопилы, топора и веревки (по естественному наклону и против него) и чего ни в коем случае нельзя делать? Техника безопасности в процессе валки деревьев: https://dzen.ru/a/Z4qBIK-a_ERTqyYy
CharlesNax
Entdecken Sie die Deutsche Online Casinos fur ein faires Spielerlebnis. Finden Sie heraus, welche deutschen Online Casinos die besten Bonusangebote <a href="https://de-onlinecasinos.com/casino-zahlungsmethoden/paysafecard-casinos/">PaySafeCard Casinos</a>
RomanKaf
Начинайте в покерной в интернете: найдите для себя вас измерение волнения и призов! Стремитесь оценить завораживающие впечатления от настоящей партии за покере, ни уходя из дома? Значит играть за сети – представляет собой ваше идеальный выход! Неисчислимое количество людей в прошлом признали выгоду а также распространенность сетевого покера, сейчас теперь пришла ваша очередь войти в данном этому волнующему галактике. В данной публикации авторы поведаем как пробовать в сети с покер – станет выгодно удобно с исключительно интригующе. Преимущества участия за <a href="https://t.me/s/Official_poker_online"> покер онлайн </a>: Доступность 24/7: Запускайте за каждое минуту времени суток с темноты, как только пользователю соответствует. Отсутствуют запретов на периодов с локации – только лишь ваш личный телефон телефон а также планшет и надежное соединение с сетью. Большой сортимент игр плюс минимумов: Среди известного Техасского Холдема Холдема до самого Омахи плюс многочисленных других вариантов – выберите раздачу, что совершенно схожа точно тебе Вам. Выбирайте пределы ставки, подходящие вашему личному резервам и еще умениям. Приятность с практичность: Избавьтесь из неудобных дорогах в направлении игорного дома и еще многолюдье рядом местами за игрой. Запускайте в приятной среде личного квартиры, в рамках практичной обмундировании а также любимым коктейлем. Случай тренинга с практики: Онлайн-ресурсы предлагают массу учебных ресурсов, способствующих поднять игровую стиль игры. Игрок имеете возможность оттачивать свои навыки забесплатно, оттачивая свои опыт, перед тем пока переключаться к игре занятию на живые резервы. Премии а также акции: Очень многие интернет-румов предоставляют крупные вступительные подарки, ежедневные события а также заезды содержащие огромными денежными резервами. Данное чудесный вероятность увеличить ваш запасы плюс приобрести дополняющее наслаждение от состязания. Безопасность плюс защита: Имя популярных онлайн-площадок утверждается строгими и суровыми законами игры в покер плюс стабильными механизмами конфиденциальности, предоставляющими чистоту и предохранение личных информации. Как заняться <a href="https://t.me/s/Official_poker_online"> Играть онлайн </a> в покер покер онлайн: Определите безопасную виртуальный зал. Уделяйте внимание внимательность наличие на лицензию, рецензии людей в интернете плюс существование многочисленных турниров. Зарегистрируйся на и завершите верификацию аккаунта. Это значит простой и быстрый и простой процесс, ключевой ради усиления сохранности. Дополните ваш баланс комфортным для вашего комфорта игрока приемом. Немало румов осуществляют различные средства пополнения счета. Начните с помощью безвозмездных игр и турниров в пределах низких ограничениях, с целью отточить ваши умения и еще увидеть клиента хорошо. Понемногу приумножайте ставки в игре по мере процессу развития личного опыта и уверенности. Не потеряйте вероятность! Запускайте участвовать в игре онлайн покер сегодня и обнаружите для вас игрока измерение азарта, выигрышей и интересных знакомств! Подберите собственную любимую игру развлечение с любуйтесь замечательными ощущениями! Пробовать онлайн – есть просто и удобно комфортно и рентабельно!
RichardHaf
Для игроков важно понимать, какие факторы влияют на безопасность и надежность таких сервисов. От удобства интерфейса до наличия лицензий и поддержки пользователей <a href="http://1.235.32.108/doku.php?id=%20%D0%9C%D0%BE%D0%B1%D0%B8%D0%BB%D1%8C%D0%BD%D0%B0%D1%8F%20%D0%B2%D0%B5%D1%80%D1%81%D0%B8%D1%8F%201%D0%B2%D0%B8%D0%BD%20%D0%BA%D0%B0%D0%B7%D0%B8%D0%BD%D0%BE:%20%D0%B8%D0%B3%D1%80%D0%B0%20%D0%BD%D0%B0%20%D1%85%D0%BE%D0%B4%D1%83">http://1.235.32.108/doku.php?id=%20%D0%9C%D0%BE%D0%B1%D0%B8%D0%BB%D1%8C%D0%BD%D0%B0%D1%8F%20%D0%B2%D0%B5%D1%80%D1%81%D0%B8%D1%8F%201%D0%B2%D0%B8%D0%BD%20%D0%BA%D0%B0%D0%B7%D0%B8%D0%BD%D0%BE:%20%D0%B8%D0%B3%D1%80%D0%B0%20%D0%BD%D0%B0%20%D1%85%D0%BE%D0%B4%D1%83</a>
Carlotreds
Одноразовый номер телефона — это временный номер, который можно использовать для получения SMS-сообщений или звонков. Эти номера могут быть полезны, когда вам нужно зарегистрироваться на сайте, не желая раскрывать свой персональный номер. Также многие используют такие номера для подтверждения аккаунтов на различных сервисах или для того, чтобы избежать спама и нежелательных звонков <a href="https://volgograd-news.net/other/2024/09/21/341917.html">купить виртуальный номер навсегда</a>
Janicedot
We specialize in creating the perfect connection between talented models and the leading platforms in the fashion industry. For more information, follow the link [url=https://camcharm.ru/model-manager/]администратор в студию вебкам [/url] Our stylists help models reach their potential by providing promotion advice and support at every stage. We also offer services for agencies looking to find the best talent for their projects.
Michaelsok
Виртуальные номера становятся все более популярными как среди частных пользователей, так и в бизнес-среде. Эти номера позволяют принимать звонки и SMS, а также использовать их для регистрации в различных сервисах без необходимости привязываться к физическому номеру телефона. Технология основывается на использовании IP-телефонии, что дает пользователю массу преимуществ по сравнению с традиционными номерами <a href="https://mama-creative.com/chto-delat-esli-ne-prihodit-kod-telegram-prichiny-i-resheniya/">почему не приходит код из инстаграма</a>
OscarIceno
2025 year jogo do tigrinho ofical site 777 <a href="https://tigrinho-fortune-tiger777.pro/">tigrinho</a>
Michaelsok
Грузоперевозки Минск по лучшей цене. Мы оказываем услугу грузоперевозок и грузового такси в Минске. График работы 24/7. Делаем квартирные, офисные и дачные переезды в Минске, по Беларуси, в Россию, и страны СНГ <a href="https://perevozimgruz.by/yslugi-gruzchikov/">Услуги грузчиков</a>
AmandaStoli
Discover the world of enjoyment with our pools! We offer a huge selection of pools, their installation and maintenance. More detailed information on the link [url=https://pools-vsem.ru/filtry/]крипсол фильтр для бассейна [/url] Create an oasis at home with high-quality solutions. Individual approach and guarantees for all work.
RickyFab
Удобный интерфейс позволяет быстро находить нужные данные, а дополнительные функции, такие как сравнение курсов в разных банках и отображение исторических графиков, делают использование сервиса максимально комфортным <a href="http://fondfinance.ru/">курс валюты сегодня</a>
MichaelChops
Имплантация — популярная процедура замещения зубов искусственными аналогами. Стоматологическая имплантология является одним из важнейших разделов современной стоматологии, предусматривающий восстановление нарушений целостности зубочелюстной системы благодаря качественным аллопластическим материалам и достижениям в области современной стоматологии <a href="https://www.dentalaesthetics.ru">костная имплантация зубов</a>
JosephDeM
Северный Кипр – это место, где восточная культура встречается с европейским комфортом, создавая идеальные условия для жизни, отдыха и инвестиций. Прекрасный климат, доступные цены на недвижимость и простые условия покупки привлекают сюда покупателей со всего мира. Но прежде чем сделать первый шаг к приобретению собственного жилья у моря, важно разобраться во всех нюансах <a href="https://iberiaproperty.ru/">кирения кипр недвижимость</a>
Nicolefug
We offer a huge range of packaging materials for any need: from film to eco-friendly solutions. Our products are ideal for moving and personal needs. For more information, click here [url=https://pack-inn.ru/upakovka-dlya-korobok/]купить коробки оптом спб [/url] We guarantee reliability and competitive prices. Packaging that protects your goods and makes them attractive - choose us for your packaging solutions!
DavidGof
https://film005.buzz
melbet линия ставок
melbet: Твой Маршрут до Победе в Свете ставок на спорт онлайн! Мечтаешь о волнующих чувствах, азартных опытах и шансе конвертировать свои знания про физкультуре в реальный прибыль? Тогда рады приветствовать в мир melbet – тотализаторной конторы, где ставки на спорт преобразуются не просто развлечением, но подлинным искусством! Мы предлагаем обширный диапазон возможностей для тех людей, кто дорожит скорость онлайн-ставок и стремится до высоким коэффициентам. Независимо из того, являешься ли ты искушенным беттором либо лишь начинаешь ваш путь, melbet – твой надежный компаньон в свете увлечения. Почему melbet – это ваш отличный подбор? Богатство Спортивных Ивентов: Наслаждайся огромным выбором дисциплин: от традиционных футбола, хоккея, тенниса и баскетбола до скоростного киберспорта, ufc, бокса, мма, волейбола, гандбола, бейсбола, крикета, дартса, регби и снукера. melbet удовлетворит любой предпочтение! Ставки на Любой Вкус: Подбирай между ставками live в способе подлинного времени, вставляя остроты переживаниям, или же делай взвешенные ставки прематч, полагаясь на свои логические способности. Выгодные Коэффициенты: Мы предлагаем одни из наиболее высоких множителей на рынке, что даст возможность вам увеличить ваш возможный приз. Комфорт и Открытость: Совершайте ставки с телефона в любое время и в всяком точке, благодаря нашему интуитивно переносному программе. Многообразие Видов Ставок: От классических ординаров к рискованных экспрессов – в нашей компании ты отыщите все виды ставок, пригодные под твой стиль игры. Применяй тотал, фору и иные опции чтобы более подвижной политики ставок. Многообразие Линии: Наша широкая черта событий включает в себе как основные чемпионаты, так и не столь популярные турниры. Актуальные Результаты: Всегда будьте в извещении последних итогов матчей, чтобы оперативно корректировать свои стратегии. Как делать ставки на melbet? Регистрация: Пройди легкую и быструю операцию записи на нашем ресурсе либо в приложении. Пополнение Счета: Подберите комфортный метод пополнения счета и внеси депозит. Выбор События: Ознакомься с линией, выбери интересующий вас поединок и разновидность спорта. Оформление Ставки: Определись со видом ставки (ординар, экспресс и т.д.), введи сумму и подтверди ваш выбор. Наслаждайся Поединком: Наблюдайте за движением ивентов и получай удовольствие от увлечения. Разнообразие ставок: больше, чем просто спорт На melbet вы можете совершать ставки не лишь на спортивные события. Мы предлагаем вдобавок линию на шоу-бизнес, давая возможность тебе прогнозировать итоги востребованных конкурсов и церемоний. Стратегии Ставок: Состязайтесь со Разумом Удача в ставках не основывается лишь из везенья. Важно разрабатывать свои собственные стратегии ставок и анализировать статистику. Melbet предоставляется каждые требуемые средства чтобы того, чтобы ты мог выполнять взвешенные решения. <a href="https://t.me/s/MELBET_RUS_OFFICIAL"> Melbet </a> – это не просто букмекерская фирма, это твой проводник в мир физкультурного азарта! Вступайте к нам непосредственно сейчас и откройте для себя свет больших возможностей. Ощутите вкус победы совместно со melbet!
Carlossob
Official website of the gaming club Gizbo Casino . Slots from famous providers. Bonuses and exclusive new products are waiting for you at Gizbo Casino <a href="https://ltcled-m.ru/">Gizbo Casino</a>
RalphToolo
Ищете способ быстро получить деньги, минуя долгие проверки и формальности? Займы онлайн на карту без отказа без проверки — это решение, которое позволит вам моментально решить финансовые вопросы. Не нужно тратить время на посещение банков или собирать многочисленные справки <a href="https://vc.ru/niksolovov/1174783-gde-vzyat-zaim-esli-uzhe-est-zaimy-top-17-mfo-v-reiting-zaimy-onlain-2025">Где взять займ если уже есть займы</a>
melbet ставки на теннис онлайн
Melbet Ставки: Твой Гид в Мир Онлайн Ставок на Спорт Ищешь гарантированного партнера для ставок на спорт? Хочешь превратить твою любовь к игре в настоящие выигрыши? Тогда тебе точно стоит уделить внимание на <a href="https://t.me/s/MELBET_RUS_OFFICIAL"> melbet ставки </a>. Melbet – является популярная букмекерская компания, обеспечивающая широкий спектр возможностей для ставок в онлайн режиме. Тут каждый, от новичка до профессионального беттера, отыщет что-то для себя. Melbet: Обзор Платформы Сайт Melbet выделяется комфортным и интуитивно понятным интерфейсом, который дает возможность просто ориентироваться даже новичку. Ты можешь смотреть прямые трансляции матчей, отслеживать результаты в режиме live, а также делать ставки как в прематч, так и в режиме лайв. На сайте ты найдешь подробный обзор всех имеющихся спортивных событий, который позволяет сделать обдуманный выбор. Что предлагает Melbet сегодня? В настоящее время Melbet предлагает лучшие условия для ставок на многообразные виды спорта. Футбол, хоккей (в том числе КХЛ и НХЛ), теннис, баскетбол (с НБА и Евролигой) – это лишь небольшая часть того, что доступно. Вас ждут турниры и чемпионаты со всего мира. Кроме того, на сайте можно найти разделы киберспорта, с играми dota, csgo, а также ставки на UFC, бои, бокс и мма. Не забываем про волейбол, гандбол, бейсбол (mlb), крикет, дартс, регби, снукер и многие другие виды спорта. Как играть и делать ставки на Melbet? Как начать играть на Melbet? Это просто! Пошагово мы покажем вам, что нужно сделать: Зарегистрируйся на сайте или в мобильном приложении (доступно для андроид и айфон). Пополни свой счет. Выбери интересующий тебя вид спорта и матч. Ознакомься с доступными коэффициентами (кф). Сделайте свой выбор и выберите тип ставки (ординар, экспресс или система). Подтверди ставку. Live ставки: ощутите азарт в реальном времени Лайв ставки на Melbet дают возможность делать ставки прямо во время матча. Вы можешь отслеживать ход игры, анализировать происходящее и быстро реагировать на изменения, что значительно повышает твои шансы на выигрыш. Трансляция матчей прямо на сайте даст возможность тебе смотреть игру и делать обдуманные ставки. Аналитика и прогнозы на Melbet Melbet не только предлагает большой выбор ставок, но и обеспечивает инструменты для анализа и прогноза. Ты можешь ознакомиться с аналитикой от экспертов, смотреть примеры прошлых матчей и использовать эту информацию для того, чтобы правильно рассчитать ваши ставки. Стратегии ставок, советы и детальный гайд для новичков дадут возможность тебе разобраться в тонкостях беттинга. Виды ставок на Melbet: от ординара до системы Melbet предлагает все виды ставок: ординар, экспресс, системы. Ты можешь сделать ставку на тотал, фору (обычную или азиатскую), а также другие виды ставок. Узнай разницу между ними, изучи правила и пример каждой из них. Melbet на телефоне: ставки в любое время и в любом месте С мобильной версией сайта и специальным приложением ты сможете делать ставки с телефона, где бы ты ни находился. Приложение для андроид и айфон – это оптимальное решение для любителей ставок в движении. Не необходимо сидеть у компьютера, чтобы участвовать в игре, просто возьмите свой гаджет. Безопасность и политику Melbet Melbet придерживается строгую политику конфиденциальности и обеспечивает безопасность ваших данных. Ты сможете быть уверены в честности и надежности платформы. Melbet: больше чем просто ставки Melbet – это не только ставки на спорт. Ты можешь найти здесь разделы со ставками на политику, выборы, шоу-бизнес и даже премии. Это делает сайт еще более интересным и разнообразным. Melbet ставки – это твой шанс окунуться в захватывающий мир беттинга. Присоединяйся к сообществу Melbet сегодня, изучите линию, выбирай высокие коэффициенты и увеличивай ваши шансы на победу! Используй полную информацию, проводи анализ, применяй стратегии и пусть тебе сопутствует удача! Где найти лучшие условия для ставок? – Безусловно же, на Melbet!
Henrytweft
On the official website of Gizbo Casino you will find everything you need for an exciting gameplay: safe transactions, a wide range of entertainment, as well as profitable bonuses. Discover a new level of gambling with Gizbo Casino <a href="https://tvorogoff.ru/">Гизбо Казино</a>
LindaMeext
We offer a huge range of accessories for numismatics, including magnifiers and specialized tools for the care of your collectibles. More detailed information on the links [url=https://monetizatoriya.ru/accessory/]альбом для банкнот [/url] and [/url] [url=https://monetizatoriya.ru/accessory/]купить альбомы для монет [/url] In addition, you will find high-quality copies of historical coins here, which will be an excellent addition to your collection.
OrlandoPelry
Гизбо Казино представляет обширный каталог игр: слоты, настольные игры, видеопокер и живые дилеры. Доступны щедрые бонусы и акции для новых и постоянных игроков <a href="https://ahservice.ru/">казино Gizbo</a>
Andreasag
We offer a wide range of high-quality equipment for mining cryptocurrencies, including graphics cards and accessories. More detailed information on the link [url=https://mini-miner.ru/asic-store/]асик на водяном охлаждении купить [/url] and [url=https://mini-miner.ru/asic-store/]купить машинки для майнинга [/url] Our company's products are ideal for both novice miners and experienced professionals seeking to optimize their operations.
Anthonytrice
Детальный разбор официального сайта Водка Казино и вход на него через актуальное и рабочее зеркало <a href="https://teremok24.su/">казино Vodka</a>
Derekcix
Казино привлекает игроков своей впечатляющей подборкой азартных игр. Хотя количество предложенных развлечений здесь не самое обширное, по стандартам качества и разнообразия оно сопоставимо с ведущими брендами игорной индустрии <a href="https://makefashion.ru/">Gizbo Casino</a>
Kevinlof
Казино Водка это новое онлайн казино, основанное в 2023 году. Оно стремительно завоевало внимание даже самых искушённых игроков в России и других странах СНГ. Водка Казино предлагает своим игрокам внушительную библиотеку игровых автоматов - свыше 2000 слотов обеспечивающимися более чем 45 провайдерами игр, где каждый игрок найдет игру по душе <a href="https://xn--c1aihrbiet.su/">казино Vodka</a>
Kevinereno
Лечение зубов — непростой процесс, который требует терпения, времени, а главное — помощи профессионала. Только консультация стоматолога и систематическая диагностика зубов могут предупредить развитие кариеса, образование зубного камня, пульпит и другие заболевания, наносящие урон как здоровью всего организма, так и вашему внешнему виду <a href="https://www.sbnation.com/users/stomvolga.ru">имплантация зубов верхней челюсти</a>
Georgebresy
В 2023 году была основана новая компания, которая на данный момент является одним из самых надежных поставщиков азартного софта. Поклонниками бренда Водка Казино являются истинные ценители классических развлечений клубов Лас-Вегаса <a href="https://master-key.su/">Водка Казино</a>
Williamkes
Компания, основанная в 2023 году, стремительно завоевала доверие как один из ведущих поставщиков азартного софта. Vodka Casino привлекает игроков, которые ценят классические развлечения в духе Лас-Вегаса <a href="https://master-key.su/">Водка Казино</a>
Larrylorry
Ищете, где купить минитрактор? Узнайте о лучших моделях и выгодных предложениях для вашего хозяйства <a href="https://traktor2025.ru/">минитрактор скаут</a>
StrobfKics
Stromectol est un mГ©dicament fiable contre les parasites. DГ©couvrez-en plus sur <a href="https://achat-stromectol.fr/">stromectol</a>.
Thomasfuevy
Что входит в стоимость имплантации 1 зуба под ключ? Анестезия, рентген, операция по установке титановых стержней, снятие слепков, наложение швов (затем снятие) <a href="https://www.mmafighting.com/users/stomvolgaru">имплантация зубов какие</a>
Randytug
Как правильно организовать подготовку к ЕГЭ? Советы преподавателей <a href="https://stroymaster-base.ru/raznoe/chto-budet-esli-ne-sdat-ege-ves-spektr-vozmozhnostej-i-posledstvij.html">https://stroymaster-base.ru/raznoe/chto-budet-esli-ne-sdat-ege-ves-spektr-vozmozhnostej-i-posledstvij.html</a>
DebraimMip
On our website you will find complete information about proposed routes, as well as important tips on preparing for a trip. Join us to discover the world from a new perspective and create memories that will stay with you forever. More detailed information on the link [url=https://morskie-otkrytiya.ru/]под парусами [/url] and [url=https://morskie-otkrytiya.ru/]под парусом [/url] Travel with us — your dream of circumnavigating the globe begins here!
StrobfKics
Les effets secondaires du Zithromax sont rares. En savoir plus sur <a href="https://achat-zithromax.fr/">zithromax effets secondaires</a>.
StrobfKics
Le <a href="https://acheter-lasix.fr/">lasix gГ©nГ©rique</a> est une option Г©conomique et efficace.
StrobfKics
Le <a href="https://acheter-priligy.fr/">priligy pharmacie</a> en ligne propose des conseils professionnels pour les clients.
JosephhoK
Стоило мне только зарегистрироваться, чувство было таким, словно перешагнул грань реальности. Эта игровая платформа будто разработано для тех, кто любит прогресс. Оформление выглядит как панель управления звездолёта: всё чётко, моментальный отклик. Финансовые операции — как мгновенный телепорт, получение выигрышей на высоком уровне. Но самое интересное — игры, каждый раунд здесь оставляет след в реальности. [url=https://kakdeti.ru/ru/]зеркало 7К казино[/url] — это не просто казино, это портал в мир чистого адреналина.
WilliamRat
Доменная почта — корпоративный почтовый сервис email для организаций 2025 <a href="https://email4domain.ru">почта со своим доменом</a>
StrobfKics
Le dosage de Ventolin est important. Plus d'infos sur <a href="https://acheter-ventolin.fr/">ventolin dosage</a>.
DouglasRiz
Функциональное тестирование программного обеспечения: как мобильные приложения, сайты и веб-сервисы проверяют на соответствие требованиям бизнеса и пользователей? Виды, задачи, этапы и примеры сценариев тестов, которые позволяют исправить ошибки разработчиков: https://vc.ru/u/3791103-infa-v-dele/1777821-funkcionalnoe-testirovanie-na-primerah-celi-vidy-instrumenty-i-trudnosti
StrobfKics
Buy Viagra in Pakistan at medicalmartpk.com. Viagra 100mg 4 Tablets. Zoom Image. cosmetics and eatables at affordable prices. Founded by CEO Mr. Jamal <a href="https://ivermectin-12mg.com/">ivermectin-12mg.com</a> Hims offers generic Viagra starting at $3 per pill, and branded Viagra starting at $139 per pill. To start with Hims, people must fill in an online questionnaire.
самые лучшие покер румы
Действуй на Настоящие Средства со Комфортом! <a href="https://t.me/s/Official_online_poker2"> Онлайн покер </a> – является ни только игра, данное вся вселенная волнения, стратегии и возможности выиграть реальные деньги, не выходя из квартиры. Когда вы пытаетесь где поиграть на покер в интернете, на русском языке а с выводом денег прямо на карту, значит вы оказались по месту. Эта статья – твой гид в мир онлайн покера в россии. Отчего Онлайн Покер настолько Популярен? Покер – это традиционная карточная игра, что целые столетия привлекала миллионы людей. Онлайн формат принес этой новую жизнь, сделав игры открытыми для каждого жаждущих. Здесь лишь несколько причин популярности онлайн покера: Удобство а открытость: Играть возможно в любое время и в каком угодно месте, обладая лишь подключение к браузере или мобильному устройству. Широкий выбор: Покеррумы предлагают разнообразные виды покера, варианты турниров а уровни ставок. Играть с реальными людьми: Ты можете бороться с реальными соперниками со целого мира, а не с компьютерными ботами. Шанс выигрывать реальные деньги: Играть на деньги – это ни просто волнение, но и возможность пополнить свой бумажник. Социальный аспект: Можно играть с друзьями или заводить новые знакомства с людьми, разделяющими твой интерес. Где Играть в Онлайн Покер в россии на Реальные Деньги? В россии есть множество сайты и покеррумы, предлагающих игры в онлайн покер. Однако как выбрать оптимальный среди них? Мы окажем помощь тебе разобраться: Популярные Покеррумы для Русских Игроков: Мы организовали рейтинг лучших покеррумов для русском языке игроков, беря во внимание такие критерии: Наличие русского языка: Интерфейс а поддержка должны быть на русском языке. Возможность играть на рубли: Депозиты и вывод средств обязаны быть доступны в рублях. Разнообразие игр и турниров: Большой выбор столов и турниров для всевозможных уровней игроков. Наличие мобильного приложения: Возможность скачать приложение для андроид и играть с мобильного устройства. Наличие прибыльных бонусов: Бездепозитным бонусом за регистрацию, начальным капиталом, бонусы на депозит и другие акции. Надежность а авторитет: Безопасность транзакций а честность игры. Топ румов регулярно обновляется, поэтому советуем наблюдать за актуальными обзорами а отзывами игроков. Особое Внимание на Минимальный Депозит: Когда ты новичок, то следует обратить внимание на покеррумы с минимальным депозитом. Это позволит вам начать играть на реальные деньги без крупных финансовых вложений. Разрешенные Покеррумы: Убедитесь, чтобы выбранный вами рум является допущенным в россии, для того чтобы не допустить возможных проблем с доступом и выводом средств. Онлайн Покер с Выводом Денег на Карту: Как Это Работает? После того, как ты решили с покеррумом а подобрали игру, ты можете положить свой баланс а начать играть на деньги. Большинство сайтов дают различные способы пополнения и вывода средств, в том числе: Банковские карты (Visa, Mastercard) Электронные кошельки Другие платежные системы Вывод денег на карту обычно требует от нескольких часов до нескольких дней, в зависимости от рума и подобранного способа вывода. Как Играть в Онлайн Покер с Друзьями? Многие покеррумы предлагают возможность играть с друзьями за приватными столами. Данное отличный способ провести время с людьми, с которыми вы знакомы, и побороться за титул оптимального игрока в вашей компании. Бесплатный Покер: Возможность Попробовать Свои Силы Если ты новичок и желаешь вначале привыкнуть с правилами, многие сайты предлагают шанс играть в бесплатный покер. Это отличный метод поупражняться а набраться опыта перед тем, как начать играть на реальные деньги. Покер на пк: Комфорт и Удобство Когда вы предпочитаете играть на пк, то большая часть покеррумов дают программы для компьютеров, которые обеспечивают более удобный а стабильный игровой процесс. Заключение: Приступайте Твой Путь в Мир Онлайн Покера Сегодня! Онлайн покер – есть захватывающая игра, что может принести тебе не просто наслаждение, но и реальные деньги. Подбирайте проверенные сайты и румы, участвуйте в турнирах, играйте с друзьями и людьми со всего мира, и знайте, что главное – это получать удовольствие от игры! Ни откладывайте на потом, приступайте твою игру в онлайн покер непосредственно сейчас! Окунитесь в мир стратегии, азарта а шансов! Везенья за столами!
Robertcex
Когда включаешь «Однажды в сказке 1 сезон», попадаешь в удивительный мир, где реальность сплетается с фантазией так тесно, что невозможно сразу понять, где заканчивается одно и начинается другое. Сюжет первой главы этой истории строится вокруг Эммы Свон, обычной на первый взгляд женщины с непростым прошлым <a href="https://odnazhdy-v-skazke-1-sezon.ru/">https://odnazhdy-v-skazke-1-sezon.ru/</a>
SolomonAvapy
Продажа русских сувениров — наш основной бизнес. Интернет-магазин «Ай, Матрешки» собрал одну из крупнейших и интереснейших в стране коллекций <a href="https://imatreshki.ru">магазин подарков в москве</a>
Robertcex
Первый сезон — это не просто история о противостоянии добра и зла, это настоящий квест, полный загадок, неожиданных поворотов и встреч с героями сказок, которые предстали в совершенно новом свете <a href="https://odnazhdy-v-skazke-1-sezon.ru/">однажды в сказке 1 сезон</a>
Matthewdaf
Интернет-магазин русских сувениров и подарков по низким ценам в Москве. Более 20 лет на рынке оптом и в розницу приходите выбирайте покупайте ждем вас <a href="https://imatreshki.ru/magazin/folder/shkatulki-lakovaya-miniatyura">купить матрешку</a>
Kevingaw
Немцы настаивают на том, что это единственный автомобиль на рынке с третьим уровнем автономности. Если вы оказались в пробке на шоссе, просто нажмите кнопку и достаньте книгу для чтения. Компьютер останавливается и запускается, сохраняя вам самые раздражающие части вождения <a href="https://www.12info.ru/oda-deshevomu-avtomobilyu-skolko-stoili-znamenitye-nemczy-snachala.html">12info.ru</a>
RicardoTralf
Наши массажистки посвятят Вам максимальное время и удивят профессиональными навыками. Все наши девушки овладели различными техниками массажа и готовы удовлетворить любого гостя, исполняя любую программу в нашем салоне «Оазис» <a href="https://sochi-eromassage.ru/">Эротический массаж в Сочи</a>
Jerold
Greetings from Los angeles! I'm bored at work so I decided to browse your website on my iphone during lunch break. I really like the information you provide here and can't wait to take a look when I get home. I'm surprised at how fast your blog loaded on my cell phone .. I'm not even using WIFI, just 3G .. Anyhow, awesome site! betflix
Kennethquign
7К казино представляет собой новый уникальный проект, запущенный в 2023 году. На его официальном сайте пользователей ожидает более двух сотен лицензионных игр, выгодные бонусы и несколько проверенных платежных сервисов для проведения денежных переводов <a href="https://bolgarfest.ru/">7K Casino</a>
MichaelPracy
7к casino – это новое онлайн казино, которая работает на игровом рынке с 2023 года. Игровой оператор предлагает развитую бонусную систему, оперативный вывод выигрышей, широкое разнообразие слотов и бесперебойный доступ к своему ресурсу за счет развитой системы рабочих зеркал <a href="https://wsr.spb.ru/">7K Casino</a>
Kennethmop
Гизбо Казино ориентировано на игроков с различными предпочтениями и бюджетами. В казино представлены игры с различными ставками, что позволяет выбирать развлечения в соответствии с индивидуальными возможностями <a href="https://xn--50-6kci7eg.xn--p1ai/">казино Gizbo</a>
Shirleyvug
Welcome to our club - a place where dance becomes art! We offer all kinds of dance styles for skill levels. For more information, follow the link [url=https://go-tango.ru/argentinskoe-tango/]школа танго для начинающих взрослых [/url] Our team professional mentors will help you develop skills and love for dance.
Sadievus
Discover the world of enjoyment with our pools! We offer a wide selection of pools, their installation and maintenance. More detailed information on the link [url=https://pools-vsem.ru/stroitelstvo-bassejnov/]сайт строительство бассейнов [/url] Create an oasis at home with best solutions. Individual approach and guarantees for all work.
Jamesdiurl
Выбирайте эротический массаж в Сочи для уникального и расслабляющего опыта. Этот вид массажа помогает снять стресс и напряжение, даря удовольствие и новые ощущения <a href="http://www.phxwomenshealth.com/index.php?option=com_k2&view=itemlist&task=user&id=1142284">http://www.phxwomenshealth.com/index.php?option=com_k2&view=itemlist&task=user&id=1142284</a>
Andrewbek
Гизбо Казино — это платформа, которая привлекает внимание игроков широким ассортиментом азартных развлечений и выгодными бонусами. Здесь вы найдете слоты с прогрессивными джекпотами, настольные игры, а также турниры, которые проходят на регулярной основе <a href="https://xn--50-6kci7eg.xn--p1ai/">Gizbo Casino</a>
Calvinhep
Наслаждайтесь игрой в любое время и в любом месте – Olymp Casino адаптирован под мобильные устройства. Удобный интерфейс и высокая производительность позволяют комфортно играть как со смартфона, так и с планшета без потери качества <a href="https://shopster.kz/">https://shopster.kz/</a>
Aaronhiz
When it comes to gambling online, understanding the legality and security of platforms like Royal Reels Casino is crucial for players. Royal Reels operates under Australian regulations, ensuring compliance with local laws. Additionally, their advanced encryption technology safeguards your personal and financial information <a href="https://royalreels101.com/">https://royalreels101.com/</a>
Reva
бесплатные моды для популярных игр — это отличный способ получить новые возможности. Особенно если вы играете на Android, модификации открывают перед вами новые возможности. Я лично использую модифицированные версии игр, чтобы достигать большего. Модификации игр дают невероятную возможность настроить игру, что взаимодействие с игрой гораздо захватывающее. Играя с модификациями, я могу повысить уровень сложности, что добавляет виртуальные путешествия и делает игру более эксклюзивной. Это действительно невероятно, как такие изменения могут улучшить взаимодействие с игрой, а при этом не нарушая использовать такие взломанные версии можно без особых проблем, если быть внимательным и следить за обновлениями. Это делает каждый игровой процесс лучше контролируемым, а возможности практически неограниченные. Рекомендую попробовать такие игры с модами для Android — это может придаст новый смысл
Online Poker
?? Сайты о покере: Мини-справочник ?? Интернет-покер предлагает множество ресурсов чтобы улучшить игру и подобрать место. Ознакомимся с основными разновидностями покерных сайтов, пригодных и для начинающих, и для продвинутых игроков. Классификация покерных сайтов: Обзоры покер-румов: Помогают выбрать надежный рум учитывая игры, бонусы и мнения. Ресурсы для обучения: Предоставляют статьи, видеоматериалы и инструменты для изучения стратегий, от основ до продвинутых. Покерные комьюнити: Сервисы для общения игроков, обмена опытом и обсуждения вопросов. Свежие новости покера: Осведомляют о турнирах, правилах и новостях покера. Статистические сайты: Позволяют анализировать игру, отслеживать свой прогресс и находить недочеты. Советы по использованию покерных сайтов: Первым делом изучите основы: Новичкам стоит изучить основы на учебных порталах. Отслеживайте новости: Будьте в теме покерных событий. Участвуйте в форумах: Обращайтесь к форумам за советами и обменом опытом. Анализируйте игру: Применяйте сайты статистики для выявления ошибок. Систематически учитесь: Совершенствуйте навыки, используя доступные ресурсы. Выбирайте проверенные сайты: Остановите выбор на проверенных источниках. Поделитесь в комментариях: Какие покерные сайты вы считаете наиболее полезными? Взято с текста: <a href="https://t.me/room_poker_online/23"> Online Poker </a> ?? Краткий Руководство в Онлайн-Покер: Старт Игры ?? Хотите начать онлайн-покер, но в раздумьях с чего начать? Данный гид направит вам начать в азарт. Покажем ключевые моменты для первых шагов. Выбор Покер-Рума Для начала приступить к игре, стоит подобрать хороший покер-рум. Обратите внимание на: Доверие и лицензия: Посмотрите, что сайт имеет лицензию и имеет хорошие отзывы. Предлагаемые игры: Интересует Техасский Холдем, Омаху а может быть варианты покера? Узнайте, что понравившийся ресурс предлагает искомые игры, что вы хотите. Приветственные бонусы: Известные покер-румы предлагают промокоды стартовым игрокам. Легкость в использовании: Сайт или обязаны быть простыми и удобными в управлении. Служба поддержки: Качественная клиентская поддержка – необходимое условие. Регистрация и Верификация Процесс регистрации как правило проста и понятна. Вам придется открыть аккаунт, заполнив форму. После этого, очень вероятно, потребуется идентификация личности, ради установить вашу индивидуальность. Это ключевая процедура чтобы гарантировать безопасность ваших средств и выполнения правил. Основные Виды Покера Техасский (Холдем): Наиболее играемая форма покера. Участники получают две карты рубашкой вверх и пять общих карт в центре. Покер Омаха (Омаха Холдем): Схожа с Холдем, но игроки получают четыре личные карты, из которых потребуется использовать две в связке с тремя общими картами на игровой поверхности. Пополнение Счета и Вывод Выигрыша Платформы для покера чаще всего дают многочисленные пути внесения депозита и получения выплат. Выберите подходящий вам способ. Стоит убедиться относительно безопасности метода. Начало Игры Начните с игр на интерес либо с микролимитами, с целью тренировать навыки, до начала играть на собственные средства. Учите правила и стратегии, до начала рисковать средствами. Основные Советы для Начинающих Набирайтесь опыта: Игра – самый эффективный способ научиться. Начните с малого: Не рискуйте большие деньги на первых этапах. Управляйте банкроллом: Рискуйте только теми деньгами, потеря которых не критична. Нужно терпение: Успех в покере зависит от времени и практики. Взято с текста: <a href="https://t.me/s/room_poker_online/11"> Онлайн Покер </a>
RamonQuiex
Используя тепловизоры, вы получаете идеальное сочетание скорости и точности, что значительно упрощает мониторинг и диагностику в самых разных областях. Как выбрать тепловизор для строительного контроля <a href="http://yiseeyou.com/free/2325">http://yiseeyou.com/free/2325</a>
Patrickbof
Интернет - магазин керамический плитки и керамогранита, для любых поверхностей и помещений <a href="https://plitka-work.ru">https://plitka-work.ru</a>
GordonVof
https://long-living.ru/
Poker Online
?? Краткий Старт в Онлайн-Покер: Старт Игры ?? Хотите играть в онлайн-покер, но сомневаетесь с чего начать? Наш обзор подскажет вам стартовать в мир покера. Рассмотрим необходимые моменты для первых шагов. Выбор Покер-Рума Перед тем как вступить в игру, необходимо подобрать хороший покер-рум. Смотрите на: Доверие и лицензия: Проверьте, что сервис зарегистрирован и пользуется доверием игроков. Предлагаемые игры: Хотите играть в Техасский Холдем, Омаху либо виды покера? Проверьте, что этот платформа имеет в наличии именно эти игры, что вам нужно. Бонусы и акции: Известные покер-румы предоставляют бонусы новым игрокам. Удобство использования: Платформа и необходимо чтобы были легкими и интуитивными для пользователя. Служба поддержки: Эффективная служба поддержки – это важный фактор. Регистрация и Верификация Регистрация чаще всего легка и понятна. Вам необходимо пройти регистрацию, заполнив форму. После этого, возможно, понадобится подтверждение личности, для заверить вашу принадлежность. Это ключевая процедура для обеспечения безопасности ваших средств и выполнения правил. Основные Виды Покера Классический покер (Texas Hold’em): Наиболее играемая форма покера. Участники получают две карманные карты и пять карт в центре стола на игровой поверхности. Разновидность Омаха (Омаха): Похожа на Холдем, но игрокам выдаются четыре карты рубашкой вверх, из которых необходимо применить две в комплекте с тремя картами в центре стола в центре. Пополнение Счета и Вывод Выигрыша Площадки для покера обычно предоставляют множество методы пополнения счета и снятия выигрыша. Определите приемлемый способ. Стоит убедиться на предмет безопасности пути. Начало Игры Приступайте к игре с бесплатных игр либо с небольшими взносами, чтобы тренировать навыки, прежде чем играть всерьез. Анализируйте основы и тактики, прежде чем вкладывать деньги. Основные Советы для Начинающих Практикуйтесь: Игра – лучший способ обучиться. Начинайте с малых ставок: Не теряйте крупными деньгами в начале. Распределяйте банкролл: Тратьте только те средства, которые можете позволить себе потерять. Важно быть терпеливым: Становление успешным игроком не приходит сразу, нужны время и практика. Взято с текста: <a href="https://t.me/game_poker_online"> Poker Online </a>
Samuelnah
Комплекты видеонаблюдения – важный элемент системы безопасности дома, офиса, а также других помещений и уличных территорий <a href="https://videonabludenie35.ru/">Выгодные системы видеонаблюдения</a>
Dannyfuh
Use the 1xBet promo code: 1XGIFT130 to receive a welcome bonus in 2025. New players will be eligible for a VIP bonus of 100% up to $130. Once you have obtained the promo code, make sure to use it during the registration process <a href="https://rl-trade.ru/pgs/1xbet_promokod_pri_registracii_bonus.html">https://rl-trade.ru/pgs/1xbet_promokod_pri_registracii_bonus.html</a>
Gemmalot
We offer a huge range of stretch films, ideal for protecting and packaging goods of any size. More detailed information on the link [url=https://pack-inn.ru/strejch-plenka-optom/]стретч пленка оптом [/url] Our film has high strength, which ensures reliable protection of your goods from contamination.
Samuelkip
Промокод MelBet при Регистрации: FreeBonus777 укажите это код в поле во время регистрации и вы получите бонус до 19 500р, а также автоматически активируете все промо акции мелбет 2025. Зарабатывайте больше с melbet промокодом актуальным сегодня <a href="http://avtovelomoto.ru/news/pages/kak_pravilyno_uhaghivaty_za_svoimi_volosami.html">http://avtovelomoto.ru/news/pages/kak_pravilyno_uhaghivaty_za_svoimi_volosami.html</a>
Bobbymycle
"Официальный веб-сайт казино Рояль предлагает искусно оформленную обстановку для азартных игроков. С его элегантным дизайном и премиальным выбором игр, Рояль является превосходным местом для тех, кто ценит качественное азартное развлечение. Исследуйте многочисленные игровых автоматов и настольных игр на авторизованном веб-сайте [url=https://royalcasino-slots.com/kk/]https://royalcasino-slots.com/kk/[/url]. Казино Рояль защищает высокий уровень клиентов и поддержку. Внимательная команда поддержки в наличии круглосуточно, готова откликнуться на любые вопросы и исправить проблемы, обеспечивая безпрерывную игру и удовлетворение."
MiguelEffek
Пользуюсь казино [url=https://www.vstpodolsk.ru/]казино Вулкан[/url] несколько недель. Мне нравится богатый выбор казино-игр и интуитивно понятный интерфейс. Платежи проходят быстро, а поддержка всегда на связи. Также есть интересные бонусы и акции для новых пользователей. В общем, могу рекомендовать. Надежность тоже на высоком уровне.
BrianFrafe
Использую казино [url=https://tv.46info.ru/LB/KAT11/795.php]рабочие сайты Вулкан[/url] несколько недель. Мне нравится разнообразный выбор слотов и простой интерфейс. Платежи проходят быстро, а поддержка всегда на связи. Также есть отличные бонусы и акции для новых пользователей. В общем, могу рекомендовать. Безопасность тоже на высоком уровне.
DavidSmern
Использую казино [url=https://employment-center.ru/LB/KAT3/145.php]онлайн казино Vulkan Royal[/url] несколько недель. Мне нравится широкий выбор казино-игр и удобный интерфейс. Платежи проходят быстро, а поддержка всегда на связи. Также есть отличные бонусы и акции для новых пользователей. В общем, могу рекомендовать. Надежность тоже на высоком уровне.
GeraldKib
Промокоды - это специальные коды, которые предоставляются игрокам в качестве поощрения за их активность. Они позволяют увеличить стартовый выигрыш в два раза и получить дополнительные средства на игровой счет <a href="https://www.flotiliya.com/misc/inc/sovety_po_prohoghdeniyu_assassin_039s_creed_revelations_osnovnye_missii_005.html">https://www.flotiliya.com/misc/inc/sovety_po_prohoghdeniyu_assassin_039s_creed_revelations_osnovnye_missii_005.html</a>
Minda
Ищете, где опубликовать или найти объявления во Владивостоке и пригороде? Присоединяйтесь к Telegram группе Доска объявлений Владивосток! Здесь вы сможете легко и быстро публиковать свои предложения по Владивостоку и краю. Хотите что-то продать или купить? Нужна работа или услуги? Всё это у нас! #объявления #Владивосток #ПриморскийКрай #ОбъявленияВладивосток Будьте в курсе всех лучших объявлений в вашем регионе! Группы остальных городов России описаны здесь... Доски объявлений России
NormanLiere
1xBet provides a wide array of bonuses and promotions for its customers in 2025. These offerings include welcome bonuses, reload bonuses, cashback bonuses, and more. The welcome bonus is typically available to new customers making their first deposit, while reload bonuses cater to existing customers who make additional deposits <a href="https://clinika-alfa.ru/blog/?1win_promokod_pri_registracii_bonus_do_200_000_rub.html">https://clinika-alfa.ru/blog/?1win_promokod_pri_registracii_bonus_do_200_000_rub.html</a>
CharlesWraby
Интернет - магазин керамический плитки и керамогранита, для любых поверхностей и помещений <a href="https://plitka-work.ru">Керамогранит для пола</a>
BrianAnere
<a href="https://autodif.ru/">Jenna Jameson</a>
Игровые автоматы казино
Грезишь о выигранном СУПЕР ПРИЗЕ В КАЗИНО?! Телеграм Канал Топ Рейтинг Казино поможет забрать ДЖЕКПОТ КАЗИНО!. У нас вы получишь информацию о казино с джекпотами, поймешь, в каких казино максимальные джекпоты казино и как их получить!. Лишь актуальная информация про Джекпоты казино и лучшие предложения для охотников за крупными призами!. Не упусти возможность на крупный выигрыш – подписывайся на наш канал: <a href="https://t.me/s/official_reyting"> Какое казино лучшее </a> Джекпот Казино ждет тебя!.
Jamesrob
После того как вы получили виртуальный номер, откройте приложение Telegram и начните процесс регистрации. Введите ваш новый номер телефона, и вам придёт SMS с кодом подтверждения <a href="https://travellanka.ru/response202.html">https://travellanka.ru/response202.html</a>
Kevinjes
"Looking for top-quality online casino games? MasalBet is the place to find the best slots from leading brands. At [url=https://masalbet.casino/tr/]masalbet.casino/tr/[/url], you’ll find newbie gifts and simple gameplay. Sign up now and get exclusive offers. Play true excitement with MasalBet! "
Jamesspoox
"Looking for high-quality slots to play? Abe Bet Casino offers the best online slots for all players! At Abe Bet [url=https://abe.bet/tr/games/demo/pragmatic_play_mustang_gold]abe.bet/tr/games/demo/pragmatic_play_mustang_gold[/url], you'll find favorite games from renowned brands. Join now to get newbie gifts. Dive into an atmosphere of thrill with Abe Bet! "
Bobbymycle
"Официальный веб-сайт казино Рояль предлагает искусно оформленную обстановку для любителей казино. С его изящным дизайном и расширенным выбором игр, Рояль является великолепным местом для тех, кто полагается качественное азартное развлечение. Исследуйте широкий спектр игровых автоматов и настольных игр на основном веб-сайте [url=https://royalcasino-slots.com/ru/]https://royalcasino-slots.com/[/url]. Казино Рояль гарантирует первоклассное обслуживание клиентов и поддержку. Поддерживающая команда поддержки в наличии круглосуточно, оборудована реагировать на различные вопросы и разрешить проблемы, обеспечивая непрерывную игру и удовлетворение."
Robinecofs
Онлайн-казино 7k — это инновационная платформа для игр с ставками с большим выбором активностей. Здесь можно найти популяризированные слоты, игры с картами и игры в реальном времени с профессиональными дилерами. Интерфейс пространный и комфортный, что делает игру приятной и неповторимой. На [url=https://neva-spb.com/ru/]сайт казино[/url] предусмотрены классные бонусы для гемблеров. В целом, платформа предоставляет отличный опыт для каждого игрока.
Davidscold
"Твой выбор для азартных игр - казино Слотозал! Слотозал предлагает обширный выбор слот-машин, выгодные бонусные программы и высокий уровень безопасности. Интерфейс сайта интуитивно понятен, навигация удобна, что дает возможность скоро найти избранные игры. Служба поддержки непрерывно настроена помочь с различными вопросами. Запишитесь на законном веб-сайте [url=https://casinoslotozal.net/ru/]играть на сайте[/url] и начните выигрывать сегодня!"
EnriqueweAth
"Казино Вулкан - это захватывающий мир азарта, который завораживает с первого взгляда. Благодаря замечательному дизайну и понятному интерфейсу, пользователи быстро оказываются в этом игровом пространстве. Среди плюсов казино [url=https://vulkan-casinosite.com/]vulkan-casinosite.com/[/url] можно выделить обширный выбор игр, включая автоматы и настольные азартные игры, которые подойдут каждому игроку. Качество графики и анимационных эффектов делает игровой процесс дополнительно увлекательным и увлекательным. Однако больше всего поразил подход казино к безопасности игроков. Они используют новейшие технологии шифрования, чтобы обеспечить безопасность личных и финансовых данных пользователей. Это делает казино Вулкан лучшим выбором для онлайн-игры."
RalphlaucT
Для многих пользователей получение доступа к WhatsApp стало необходимостью, но не у всех есть возможность использовать свой номер телефона. На счастье, существует несколько способов, как можно зарегистрироваться в WhatsApp без номера <a href="https://ftimes.ru/551622-virtualnyj-tureczkij-nomer-telefona-zachem-nuzhen-i-gde-primenyaetsya.html">https://ftimes.ru/551622-virtualnyj-tureczkij-nomer-telefona-zachem-nuzhen-i-gde-primenyaetsya.html</a>
BradleyFum
Предоставляет анонимные/элитные, приватные и персональные прокси для работы с социальными сетями, сайтами, приложениями, программами и играми <a href="https://smartshop124.ru/the_articles/postavschik-proksi-serverov.html">https://smartshop124.ru/the_articles/postavschik-proksi-serverov.html</a>
Bobbymycle
Множество игроков предпочитают [url=https://da-a.ru/]официальный сайт[/url] за простую систему ставок и щедрые бонусы. Слоты действительно интересные, а поддержка работает без выходных. Рекомендую зарегистрироваться, потому что результатом я удовлетворен.
Robinecofs
Это казино предпочитают [url=https://pokerdom-one.com/]покердом казино[/url] за гибкую систему ставок и щедрые бонусы. Слоты действительно увлекательные, а поддержка работает в любое время. Рекомендую зарегистрироваться, потому что результатом я доволен.
EnriqueweAth
Это казино предпочитают [url=https://703002.ru/]онлайн казино[/url] за удобную систему ставок и регулярные бонусы. Слоты действительно увлекательные, а поддержка работает круглосуточно. Рекомендую внести депозит, потому что результатом я доволен.
HarryHat
Множество игроков предпочитают [url=https://space24.top/chto-delat-novichku/]максбет онлайн[/url] за простую систему ставок и регулярные бонусы. Слоты действительно разнообразные, а поддержка работает в любое время. Рекомендую внести депозит, потому что результатом я удовлетворен.
Lindaidiok
Our company specializes in manufacturing and sale of high-quality gabions, which are ideal for various construction projects. More detailed information on the links [url=https://gabi-one.ru/gabiony-matrac-reno/]сетка матрац рено [/url] и [url=https://gabi-one.ru/gabiony-matrac-reno/]матрас под габион [/url] Our products are made of durable galvanized steel and have a durable coating, which ensures their high resistance to corrosion and environmental influences.
NormanFer
Нашёл недавно интересный путеводитель по Калининграду. Там есть готовые маршруты, идеи, обзоры достопримечательностей и советы где поесть <a href="https://sezon5.ru/news1/desjat-kaliningradskih-zhemchuzhin-deljus.html">https://sezon5.ru/news1/desjat-kaliningradskih-zhemchuzhin-deljus.html</a>
MichaelFadly
UnlockTool активация лицензии и продление на 3, 6, 12 месяцев, official unlocktool license activation extension & renewal 3, 6, 12 months <a href="https://gsmforum.ru/threads/cellebrite-ufed-4pc.341176/">fed</a>
Anthonyseaps
Banda Casino – официальный сайт с лучшими играми и бонусами до 750% . Вход открыт! Наслаждайтесь лицензированными слотами и быстрыми выплатами <a href="https://www.dom-nam.ru/index.php/forum/stroitelnye-kompanii/162747-posovetujte-nadezhnoe-onlajn-kazino#200413">Сайт Банда Казино</a>
Lindaidiok
We specialize in in manufacturing and supply of high-quality gabions, which are ideal for various construction projects. More detailed information on the links [url=https://gabi-one.ru/gabiony-korobchatye/]конструкции габионные коробчатые [/url] и [url=https://gabi-one.ru/gabiony-korobchatye/]габион коробчатый цена [/url] Our gabions are manufactured are made of durable galvanized steel and have a durable coating, which ensures their high resistance to corrosion and environmental influences.
Jamestwity
Вы можете купить справки в Москве в нашей клинике https://volgamedconsalt.ru/.
JefferyAssog
Фабрика дверей «Браво» не первый год выпускает на рынок строительных материалов межкомнатные двери. За десятилетие фирма завоевала огромную популярность благодаря высокому качеству изделий <a href="https://169.ru/mezhkomnatnye-dveri/raspashnye/">двери межкомнатные распашные</a>
Jamestwity
Вы можете купить справку в медцентре https://biomed-slv.ru/ с доставкой по Москве.
MalissaShier
[url=https://vkus-msk.ru/naturalnyj/]ароматизатор
JamesDiamb
Arkada Casino – это новый проект в мире онлайн-гемблинга, запущенный в 2024 году. На официальном сайте вас ждёт более 200 лицензированных игр, привлекательные бонусы и проверенные платежные сервисы для удобных переводов. Регистрируйся, делай первый депозит и оцени сам все преимущества <a href="https://ideashunter.ru">Arkada Casino</a>
DavidBar
To give the people an example of the power of Ashur, my lord, I hung the heads of Sanduarri and Abdi-Milkutti round the necks of their most prominent citizens, whom, thus adorned, I made walk in procession along the streets of Nineveh, to the strains of singers accompanying themselves on harps <a href="https://tigergrp.org/cn/blog/event-planning-services-create-unforgettable-luxury-experiences-in-ibiza">伊维萨岛高端活动策划服务 | Tiger Group为您打造难忘庆典 | Tiger Group</a>
CharlesCaw
Вы можете купить медсправку в нашем мед центре https://inrosmed.ru/ в Москве без медкомиссий.
Russelspela
Вы можете купить медицинскую справку в мед центре https://klinika-almaz.ru/ в Москве без прохождения врачей.
Larrycrype
Если вам нужны обновленные версии приложений и игр, стоит выбирать только проверенные источники. В сети можно найти множество сайтов, но далеко не все из них предлагают качественные APK-файлы без вирусов. Например, на этом ресурсе можно найти популярные игры и программы, включая модификации с дополнительными возможностями https://androhack.ru/8246-android-1.html
JosephPlulk
Гизбо Казино ориентировано на игроков с различными предпочтениями и бюджетами. В казино представлены игры с различными ставками, что позволяет выбирать развлечения в соответствии с индивидуальными возможностями <a href="https://xn---74-5cdtz8afiwl4c8g.xn--p1ai/">казино Gizbo</a>
Donaldhergo
Вы можете купить справку в клинике https://med-analysis.ru/ по Москве с бесплатной доставкой до любой станции метро.
KennethSuith
Гизбо Казино — это платформа, которая привлекает внимание игроков широким ассортиментом азартных развлечений и выгодными бонусами. Здесь вы найдете слоты с прогрессивными джекпотами, настольные игры, а также турниры, которые проходят на регулярной основе <a href="https://xn---74-5cdtz8afiwl4c8g.xn--p1ai/">Гизбо Казино</a>
Donaldhergo
Вы можете купить справку в поликлинике https://medlady.ru/ по Москве с доставкой до станции метро.
EverettIropy
Вы можете купить справку в медицинском центре https://dentaleclinic.ru/ в Москве без прохождения врачей.
DavidLiete
Играть онлайн в Гизбо Казино. Каждый посетитель Гизбо Казино может воспользоваться системой поддержки, которая работает круглосуточно <a href="https://xn--23-6kcaaa7ag2bkmec4bd8bzo.xn--p1ai/">Гизбо Казино</a>
LewisWhatt
Вы можете купить справки в Москве в нашей клинике https://medcenterpenza.ru/.
Kevinjes
Онлайн-казино 7k — это новейшая платформа для игр с ставками с большим выбором развлечений. Здесь можно найти лучшие игровые автоматы, настольные игры и живое казино с профессиональными дилерами. Оформление сайта интуитивно понятный и легкий в использовании, что делает игру удобной и неповторимой. На [url=https://neva-spb.com/ru/]neva-spb.com[/url] предусмотрены бонусные предложения для любителей азартных игр. В целом, казино предоставляет уникальный опыт для каждого игрока.
Jamesspoox
"Ваш выбор для гемблинга - казино Слотозал! Слотозал предлагает обширный ассортимент слот-машин, привлекательные бонусы и надежный уровень безопасности. Интерфейс веб-сайта интуитивно понятен, навигация проста, что дает возможность быстро найти предпочтенные игры. Команда поддержки постоянно настроена ассистировать с всеми вопросами. Пройдите регистрацию на основном веб-сайте [url=https://casinoslotozal.net/ru/]https://casinoslotozal.net/ru/[/url] и приступите к завоевывать призы сегодня!"
Bobbymycle
"Официальный веб-сайт казино Рояль предлагает стильную обстановку для гемблеров. С его изысканным дизайном и расширенным выбором игр, Рояль является превосходным местом для тех, кто обожает качественное азартное развлечение. Исследуйте широкий спектр игровых автоматов и настольных игр на официальном веб-сайте [url=https://royalcasino-slots.com/ru/]https://royalcasino-slots.com/[/url]. Казино Рояль гарантирует высокий уровень клиентов и поддержку. Отзывчивая команда поддержки готова круглосуточно, подготовлена ответить на любые возникающие вопросы и урегулировать проблемы, предоставляя непрерывную игру и удовлетворение."
Robinecofs
"Looking for high-quality slots to play? Abe Bet Casino offers endless variety online slots for all players! At Abe Bet [url=https://abe.bet/tr/games/demo/jetx]https://abe.bet/tr/games/demo/jetx[/url], you'll find slot hits from top developers. Sign up now to get generous bonuses. Dive into real gameplay with AbeBet! "
Davidscold
"Looking for top-quality online casino games? MasalBet is the place to find new slot hits from leading brands. At [url=https://masalbet.casino/tr/]masalbet.casino[/url], you’ll find generous bonuses and easy navigation. Join now and get gifts for new players. Play true excitement with MasalBet! "
KennethCance
Вы можете купить справку в медцентре https://diagnoz-med.ru/ с доставкой по Москве.
CecileWeedy
Our company specializes in manufacturing and sale natural colors More detailed information on the link [url=https://vkus-msk.ru/naturalnyj/]натуральные ароматизаторы
Desmondbop
Напёрстки для курения — это уникальные приспособления, призванные сделать процесс курения удобнее, чище и безопаснее <a href="https://shyker.com.ua/yak-vibrati-idealnij-kovpak-dlya-kurinnya-poradi-novachkam/">https://shyker.com.ua/yak-vibrati-idealnij-kovpak-dlya-kurinnya-poradi-novachkam/</a>
GloriaPudge
Our company specializes in manufacturing and supply natural colors More detailed information on the link [url=https://vkus-msk.ru/naturalnyj/]ароматизаторы купить
SandraBor
Our company specializes in manufacturing and supply of high-quality gabions, which are ideal for various landscaping projects. More detailed information on the links [url=https://gabionn.ru/]купить сетку для габионов в новосибирске [/url] Our gabions are manufactured are made of durable galvanized steel and have a durable coating, which ensures their high resistance to corrosion and environmental influences.
CharlesVor
Чат Рулетка — самый популярный видеочат во всем мире. Наш чат не имеет аналогов и принципиально отличается от других видеочатов <a href="https://sexcam18.ru/">https://sexcam18.ru/</a>
Charlesplupt
Нормальное казино, платит. Сам играю в Joycasino и после выигрыша вывожу деньги и доходят довольно быстро. Всегда выводил через электронные кошельки, мне так <a href="https://pizzanyam.ru/">казино play fortuna</a>
Jasonsnack
Гизбо Казино — это платформа, которая привлекает внимание игроков широким ассортиментом азартных развлечений и выгодными бонусами. Здесь вы найдете слоты с прогрессивными джекпотами, настольные игры, а также турниры, которые проходят на регулярной основе <a href="https://xn----ftb7abdedvc.xn--p1acf/">Гизбо Казино</a>
Rachaelgon
Discover the world of enjoyment with our pools! We offer a widest selection of pools, their installation and maintenance. More detailed information on the link [url=https://pools-vsem.ru/stroitelstvo-bassejnov2/]строительство капитального бассейна [/url] Create an oasis at home with high-quality solutions. Professional installation and guarantees for all work.
LeonardHorie
Частенько Fonbet раздаёт эксклюзивные коды на фрибеты – бесплатная ставка, которая не требует, чтобы на балансе были деньги. Если выполните все условия букмекерской конторы и выиграете, тогда кеш зачислится уже в виде реальных денег. Их получится перевести на карточку или e-кошелёк <a href="https://www.inserrh.com/media/pgs/code_promotionnel_1xbet.html">https://www.inserrh.com/media/pgs/code_promotionnel_1xbet.html</a>
Davidlah
Обладает тонизирующим и антиоксидантным свойствами, лифтинг эффектом, улучшает упругость, предотвращает старение кожи, помогает избежать преждевременного появления большого количества морщин, уменьшает пигментацию, способствует уменьшению проявлений сосудистой сеточки на лице, способствует устранению воспалительных процессов на коже, эпителизации <a href="https://bioquant-garyaev.com/product/svechi-volnovye-vaginalnye-onda-v/">https://bioquant-garyaev.com/product/svechi-volnovye-vaginalnye-onda-v/</a>
GregoryGog
Зачем же нужна накрутка лайков? Прежде всего, это способ привлечь внимание к вашему контенту. У пользователей сложилось мнение, что видео с большим количеством лайков более качественное и интересное <a href="https://ttlaivc.ru">накрутка лайков на комментарии в Тик Ток</a>
KelvinNic
Существует множество способов накрутки лайков. Некоторые из них легитимны и позволяют вам получить настоящую аудиторию, а другие могут привести к бану аккаунта. Важно выбирать правильные методы, чтобы избежать негативных последствий <a href="https://ttlaikovc.ru">накрутка лайков в ТТ купить</a>
Vincentgam
Официальный сайт Vodka Casino: регистрация и вход в Водка Казино онлайн. Vodka Casino предлагает пользователям уникальные возможности для игры в онлайн-казино <a href="https://flashboom.su">Водка Казино промокод</a>
Terryunjus
Arkada Casino - это игровая платформа, предлагающая посетителям удобный доступ к азартным играм и высокую надежность. Здесь игроки со всего света смогут насладиться азартом в любое время и в любом месте <a href="https://forum.ssa.ru/cat-Novyiy-razdel/topic-37857.html">Arkada Casino официальный сайт</a>
BobbyKat
Если вы ищете волнение и азарт, предлагаем обратить внимание на Banda Casino. Онлайн-казино представляет большой перечень игр, среди которых каждый найдет что-то интересное. Благодаря безопасным транзакциям и современной мобильной версии, вы можете насладиться игрой в любом месте, где имеется интернет <a href="http://suhinfo.ru/index.php/%D0%9E%D0%BD%D0%BB%D0%B0%D0%B9%D0%BD-%D0%BA%D0%B0%D0%B7%D0%B8%D0%BD%D0%BE_%D0%BD%D0%BE%D0%B2%D0%BE%D0%B3%D0%BE_%D0%BF%D0%BE%D0%BA%D0%BE%D0%BB%D0%B5%D0%BD%D0%B8%D1%8F:_Banda_Casino">Казино Banda скачать</a>
Jameshax
Казино Раменбет - это прогрессивная онлайн-площадка для развлечений, которая очень быстро завоевала популярность благодаря щедрым бонусам, разнообразию игр и приятным условиям. Лицензированное казино обеспечивает комфорт и безопасность на каждом этапе взаимодействия <a href="https://kofeinia.org/viewtopic.php?f=151&t=38176">Раменбет Казино официальный сайт</a>
Willievom
Casino Starda предлагает доступ к сертифицированным игровым автоматам от популярных провайдеров, гарантируя честный игровой процесс. Для удобства посетителей создана надежная система. Казино обеспечивает полную защиту данных и выполнение обязательств перед клиентами <a href="http://ractis.ru/forums/index.php?autocom=gallery&req=si&img=3133">Сайт Казино Starda</a>
DavidAgora
Мы предоставляем аренду автомобилей для крупных компаний и частных лиц, а также для малого и среднего бизнеса. Наша компания предлагает широкий выбор автомобилей, включая эконом-класс, бизнес-класс, минивэны и коммерческие авто, чтобы каждый клиент мог подобрать машину, соответствующую его требованиям <a href="https://avtocar5.ru/">Бизнес-класс автомобилей в аренду</a>
Rachaelgon
Discover the world of comfort with our pools! We offer a widest selection of pools, their installation and maintenance. More detailed information on the link [url=https://pools-vsem.ru/stroitelstvo-bassejnov2/]построить частный бассейн [/url] Create an oasis at home with high-quality solutions. Individual approach and guarantees for all work.
Floydoptot
Если вас интересует официальный сайт Сукааа Казино - вся самая актуальная информация размещена на нашем портале. А мы рассмотрим главные преимущества, которые предлагает эта онлайн-площадка <a href="http://wiki.market-master.ru/index.php/Sykaaa_Casino_%D0%BE%D1%84%D0%B8%D1%86%D0%B8%D0%B0%D0%BB%D1%8C%D0%BD%D1%8B%D0%B9_%D1%81%D0%B0%D0%B9%D1%82">Sykaaa Casino игровые автоматы</a>
Micheallug
Trix is for four players and has four kingdoms, each of which has five games: King, Queens, Diamonds, Ltoosh and Trix <a href="https://trix.fit/">Анкоры: is it better to masturbate without porn</a>
HenryPed
Kometa casino – новое развлекательное развлекательное казино, предлагает вашему вниманию свыше 5 600 онлайн-игр от ведущих брендов, регулярные бонусы, промо <a href="https://kirillmeschc.ru">Kometa Casino официальный сайт</a>
Albertvoina
Kometa Casino – новое онлайн-казино, запущенное в России в 2024 году. Платформа работает по лицензии Кюрасао, обеспечивая безопасный игровой процесс <a href="https://uradres.su">Комета Казино промокод</a>
Elmermup
Казино Гама работает по лицензии Кюрасао, предоставляет большой выбор качественных игр и надежные способы платежей. Пользователям доступны счета в рублях <a href="https://xn--80aa5aiddcegy8c4ed.xn--p1ai">Гама Казино вход</a>
1xbet registration bd online
You commit an error. I suggest it to discuss. Write to me in PM.
GradyAwaiz
https://xnude.app/ революционная система ИИ. Раздеть девушку или мужчину сервис на основе deepnude может практически на любом фото. Стоимость: Практически бесплатная нейросеть ибо использует токены от проекта https://gpton.co/. Месячная оплата за сервис составляет 1000 рублей. Функционал: Управление интуитивно понятное, простое, есть минимальное количество кнопок: Раздевание, Генерация, Чат, Партнерка и Пополнение. Очень много дополнительных функций таких как замена лица смена пола смена рассы итд. ИИ отлично справляется с обнажением, при этом может создавать картинки с нуля или корректировать существующие. Система функционирует в режиме онлайн и сохраняет под каждого пользователя персональную базу картинок, ее невозможно вытащить третьим лицам из-за шифрования SHA512. Это топовая платформа на основе нейросети deepnude, которая способна генерировать реальные фото или в стиле аниме. Система отлично справляется с раздеванием загруженных фото. Это полный конкурентный вариант сервиса с множеством опций.
LarryCix
The official website of the online casino Pinko invites all new players to quickly register and start playing the most popular slots and gaming machines <a href="http://pinco-az2024.com">pinco</a>
GrantQuoma
В ассортименте качественные электронные сигареты многоразовые от ведущих производителей: Brusko, Voopoo, Elf, Smoant, Vaporesso, Pasito, Smok, GeekVape <a href="https://vse-sigarety.ru/">хороший магазин</a>
TerryLauff
1win Casino предлагает широкий выбор азартных игр, от классических слотов до живых дилеров <a href="https://lefortovopark.ru/threads/otvety-na-populjarnye-mify-o-1win-casino.2044/">https://lefortovopark.ru/threads/otvety-na-populjarnye-mify-o-1win-casino.2044/</a>
WilliamFligo
Многие фанаты Hacksaw Gaming с нетерпением ждали новой игры от провайдера, и Le Bandit полностью оправдало их ожидания <a href="https://respectrb.ru/files/u1/?vavada__bonusu__promokodu_i_registraciya_vavada.html">Vavada вход</a>
Dustinzense
Играйте в самые популярные слоты, блэкджек, рулетку и многое другое в 1Го Казино. Зарегистрируйтесь сейчас и получите доступ к бонусам для новых <a href="https://xn---1-24-3vex3ajr0bmd.xn--p1ai">1Го Казино бонусы</a>
MichaelVob
Are you looking for the best platform with the best bonuses for Argentina <a href="https://nostrabet.com/pe/1xbet-bonus-code-peru/">1xcasino er promo code</a>
MichaelNub
В темной комнате общаги студентка решилась на смелый поступок. Сначала она дрочит, предвкушая встречу, а одногруппник гордо показывает свою хуе. Вскоре они ебется, а другие ребята тихо дрочат, наблюдая за происходящим <a href="https://h-msk.ru/">мастурбируют</a>
Timothytam
В жаркий вечер общаги, смелая студентка решилась на рискованный эксперимент. Сначала она тихо дрочит, предвкушая необузданные ощущения, пока её одногруппник с вызывающей уверенностью выставляет свою хуе. Ночь накаляется, когда страсть достигает предела: он ебется с пылом, а в соседней комнате другие ребята, под впечатлением происходящего, дрочат, создавая атмосферу всеобщего эротического безумия <a href="https://trix16.casino/">ебется</a>
Tommywes
Casino 1xbet is available to players on the website of the famous bookmaker, founded in 1997. The section with video slots and other gambling games appeared several years ago, but quickly attracted users thanks to the established customer base <a href="https://nostrabet.com/cm/1xbet-bonus-code-cameroon/">Code promo 1xcasino Pakistan</a>
Herbertbiops
1xBet es una de las mejores casas de apuestas del mercado para los usuarios <a href="https://famousfossilwinery.com/bonuses/1xbet-promo-codes/">Código de bônus 1xcasino Marrocos</a>
JamesRaf
cross border pharmacy canada: <a href=" https://expresscanadapharm.shop/# ">Express Canada Pharm</a> - Express Canada Pharm
AndresHot
План эвакуации документ предназначенный для определения первичных средств пожаротушения и эвакуационных выходов. Поэтому, доверять разработку только профессионалом своего дела <a href="http://malahov-consultant.ru/plan-evakuatsii-partnery/">Купить план эвакуации</a>
Patrickacive
К возможностям онлайн-обучения в последнее время прибегает всё больше людей <a href="https://altaex.ru/mix/preimushhestva-polucheniya-professii-v-sfere-it-i-sovety-pri-vybore-onlajn-kursov/">https://altaex.ru/mix/preimushhestva-polucheniya-professii-v-sfere-it-i-sovety-pri-vybore-onlajn-kursov/</a>
Scottfaw
buy prescription drugs from canada cheap https://expresscanadapharm.com/# Express Canada Pharm canadian neighbor pharmacy
MichaelZic
http://biprof.ru/
Marcosloyap
DID предоставляет номера с кодами более чем 150 стран. Это позволяет выбрать номер, соответствующий вашему текущему местоположению или бизнес-целям <a href="https://mythreal.ru/novoe/virtualnye-nomera-telefonov-udobstvo-i-bezopasnost-kommunikaczij.html">виртуальный номер телефона</a>
TimothyPLoms
Виртуальный номер создаёт впечатление солидности и профессионализма. Клиенты и партнёры воспринимают компании с городскими или бесплатными номерами (например, формата 800) как надёжные и серьёзные организации <a href="https://clodoserver.ru/virtualnye-nomera-telefonov-sravnenie-s-traditsionnymi-nomerami/">купить номер телефона навсегда</a>
Keithgot
Это лучшие продукты и слоты, которые заслужили свое место в топе. Ссылки на вход с их официальных сайтов с телефона или компьютера — в нашем канале <a href="https://t.me/proverennye_onlajn_kazino_russia">лучшие казино с быстрым выводом денег</a>
Michaelvah
<a href=https://bitlygl.wordpress.com/2024/01/02/мир-роскоши-и-гостеприимства-отель-glory/>Glory Casino</a> [url=https://transferato.co.uk/Reviews/]MichaelSlirl[/url] 5938ac0
Donaldnen
Нужен по настоящему красивый номер, но нет большой суммы для разового платежа? Подключите номер и просто вносите ежемесячную плату за использование <a href="https://voronezh-news.net/other/2024/11/04/348708.html">купить виртуальный номер телефона</a>
Michaelbox
Boost your content revenue with Scrile Connect. Our white-label platform is an alternative to OnlyFans, offering custom onlyfans tools <a href="https://medium.com/scrile-connect/how-to-start-your-own-private-social-network-platform-8b920af8c5b7">private social network for business</a>
Rogertwisk
Le code promo 1xBet valide: BONUS1X200 – recevez un bonus de bienvenue de 100% jusqu'a 130€ en utilisant ce code code promo 1xbet abidjan lors de votre inscription sur le site 1xBet <a href="https://garrettyper76420.blogs-service.com/64499306/1xbet-promo-code-100-welcome-bonus-up-to-130">https://garrettyper76420.blogs-service.com/64499306/1xbet-promo-code-100-welcome-bonus-up-to-130</a>
melbet.com login
On mine the theme is rather interesting. I suggest all to take part in discussion more actively.
Ernestfab
This iconic hotel, renowned for its rich history, exquisite architecture, and world-class amenities, offers guests an unparalleled experience of comfort and elegance <a href="https://eddytreeserviceva.com/blog/emergency-tree-removal-what-to-do-after-a-storm">Emergency Tree Removal: What to Do After a Storm</a>
DavidNek
The story of the Hebrews, the descendants of Abraham, is a tapestry of miracles, trials, triumphs, and divine promises that have withstood the test of time <a href="https://maps.free-bible.com/blog/from-babylon-to-jerusalem-understanding-the-exile-through-maps">how to download a reddit video</a>
KennethPhase
Выбирайте платформер с разнообразием уровней и механик. Игры, предлагающие уникальные задачи и элементы, удерживают интерес. Обратите внимание на истории и персонажей – хорошая нарративная составляющая усиливает вовлеченность <a href="http://jamsun.net/doku.php?id=%20%D0%9A%D1%80%D0%BE%D1%81%D1%81-%D0%BF%D0%BB%D0%B0%D1%82%D1%84%D0%BE%D1%80%D0%BC%D0%B5%D0%BD%D0%BD%D1%8B%D0%B5%20JRPG:%20%D0%BA%D0%B0%D0%BA%20%D0%BF%D1%80%D0%B0%D0%B2%D0%B8%D0%BB%D1%8C%D0%BD%D0%BE%20%D0%B2%D1%8B%D0%B1%D1%80%D0%B0%D1%82%D1%8C%20%D0%B8%20%D0%BA%D1%83%D0%BF%D0%B8%D1%82%D1%8C?">http://jamsun.net/doku.php?id=%20%D0%9A%D1%80%D0%BE%D1%81%D1%81-%D0%BF%D0%BB%D0%B0%D1%82%D1%84%D0%BE%D1%80%D0%BC%D0%B5%D0%BD%D0%BD%D1%8B%D0%B5%20JRPG:%20%D0%BA%D0%B0%D0%BA%20%D0%BF%D1%80%D0%B0%D0%B2%D0%B8%D0%BB%D1%8C%D0%BD%D0%BE%20%D0%B2%D1%8B%D0%B1%D1%80%D0%B0%D1%82%D1%8C%20%D0%B8%20%D0%BA%D1%83%D0%BF%D0%B8%D1%82%D1%8C?</a>
WalterErync
В нашем салоне можно продать новые модели швейцарских часов, в таком случае сумма выплаты будет более привлекательная. Гарантируем быструю возможность купить в каталоге или продать за 1 день <a href="https://mir-watch.ru">оценка часов</a>
Davidson
В 2025 году российский туризм продолжает активно развиваться, предлагая путешественникам новые направления и обновлённые достопримечательности. Ниже представлены ключевые события и тенденции в сфере туризма и культуры России <a href="https://vokrugo.ru/turizm-rossija/moskva">Туристическая москва</a>
JaredVethy
https://1xbetlklogin.com/
Donaldfoome
Pегистрация у операторов связи. Некоторые операторы связи также предоставляют возможность зарегистрировать виртуальный номер в своей сети <a href="https://www.justmedia.ru/news/russiaandworld/virtualnyye-nomera-udobstvo-i-bezopasnost-v-tsifrovom-mire">https://www.justmedia.ru/news/russiaandworld/virtualnyye-nomera-udobstvo-i-bezopasnost-v-tsifrovom-mire</a>
Grahamslima
Одноразовые номера не предназначены для голосового общения. С их помощью разрешено лишь получать или же быстро отправлять СМС в течение определенного отрезка времени. Они не привязаны ни к абонентам, ни к конкретным устройствам <a href="https://newsstroy.kharkiv.ua/virtualnyj-nomer-telefona-osobennosti-preimushhestva-i-sfery-primeneniya.html">https://newsstroy.kharkiv.ua/virtualnyj-nomer-telefona-osobennosti-preimushhestva-i-sfery-primeneniya.html</a>
Carltoncoito
Мобильное казино Пин Ап. Пин Ап обеспечивает комфортный доступ к слотам и Live-казино прямо с мобильных устройств. Игры доступны везде, где есть интернет <a href="https://maturidi.kz/">https://maturidi.kz/</a>
DwayneWhefe
Если вы хотите продать свои часы, лучше всего обратиться в специализированные компании, которые занимаются выкупом часов <a href="http://www.artpiter.spb.ru/forum/thread3425.html#4128">http://www.artpiter.spb.ru/forum/thread3425.html#4128</a>
Donaldmit
Букмекерская контора и онлайн-казино Mostbet приветствует вас на официальном сайте своего бесплатного приложения для Android телефонов. Здесь вы можете скачать <a href="https://jetairlines.kz/">https://jetairlines.kz/</a>
Hubertfew
Casino Mostbet успешно объединяет БК и слоты, занимая топовые позиции на рынке много лет. Каталог с игровым софтом на сайте содержит высококачественный контент, включая разнообразные слоты, Live, карточные и настольные развлечения <a href="https://mebel-komfort.kz/">mostbet официальный сайт скачать</a>
Alfredlet
Если вы ищете надежную платформу для спортивных ставок, обратите внимание на 1вин. Этот сервис предлагает широкий выбор спортивных событий и различных рынков, что делает ставку не только интересной, но и прибыльной <a href="http://introsystems.ru/component/kunena/suggestion-box/38325-1win-zerkalo-sovety-po-bezopasnomu-dostupu">http://introsystems.ru/component/kunena/suggestion-box/38325-1win-zerkalo-sovety-po-bezopasnomu-dostupu</a>
Jerrydeege
Широкая линия и LIVE-события. Онлайн ставки на спорт с бонусами и акциями. Высокие коэффициенты топовое онлайн-казино Казахстана <a href="https://regulator.kz/">https://regulator.kz/</a>
Kennethpek
Medispensary Marijuana Delivery is the the best service providing cannabis at any price and taste <a href="http://www.iheartmyteacher.org/proxy.php?link=https://www.sexand.toys/">link</a>
LorenzoPiods
I'm always impressed with their efficient system. <a href=" https://clomidpharm24.top/# ">buy generic clomid prices</a> Their international patient care is impeccable.
Donaldgaf
Осуществите Мечту о Идеальном Ремонте с Эксперт ремонта - Без Предоплаты! Доверьте Нам Свою Квартиру <a href="https://ekspert-remonta.blizko.kz/">ремонт квартир под ключ отзывы Алматы</a>
ThomasPoito
Prepare for IPL 2025 betting with top online casinos in India! We offer a list of the best IPL betting sites with great odds, quick payouts, and bonuses up to 500%. Find trusted platforms, safe payment methods, and expert IPL betting tips to enhance your season. Start betting today <a href="https://iplbettingonline.in/">ipl online betting</a>
Jetta
Pinco казино: увлекательные игры, продуманный сервис и выгодные предложения Современные интернет-казино предлагают гостям не только поймать удачу за хвост, а также погрузиться в удобную игру, в чем сочетаются азарт, простота и большая коллекция игр. Pinco казино – это одна из лучших среда, какая открывает двери любителям азартных игр получать эмоции отличными развлечениями, привлекательными акциями и эксклюзивными подарками. Если вы ищете платформу, где можно не лишь развлечься, но и выиграть крупные суммы, то этот игровой клуб станет отличным выбором. Телеграм-канал Pinco казино Чтобы всегда быть в курсе актуальной информации, старта конкурсов, обновлений каталога и специальных акций, стоит подписаться на проверенную группу в Telegram азартного клуба Pinco. На канале публикуются актуальные новости, плюс эксклюзивные предложения, которые помогут делать успешные ставки и повысить уровень азарта. Участники канала получают доступ к эксклюзивным поощрениям, секретным кодам и программам лояльности, позволяет играть с максимальной выгодой. Выбор игр и фишки казино Pinco казино даёт возможность своим пользователям разнообразие азартных развлечений. На платформе представлены игровые автоматы топовых студий, классические настольные игры, живое казино и множество других увлекательных опций. Клиенты получают доступ к разнообразием игровых автоматов, начиная от классических аппаратов вплоть до современных видеослотов с продвинутыми функциями и бонусными раундами. Помимо автоматов, на сайте представлены игра рулетка, карточные турниры, популярная карточная игра и настольные развлечения, которые привлекают игроков без опыта, а также опытных игроков. С интуитивным дизайном, каждый может за секунды разобраться с выбором и приступить к увлекательному процессу. Программы лояльности и акции Главным достоинством Pinco игровой платформы считаются выгодные бонусные предложения. Начинающие пользователи имеют возможность получить на приветственный пакет, который включает подарки при внесении денег и бесплатные вращения. Зарегистрированные игроки действуют эксклюзивные награды, кэшбэки и уникальные акции, которые позволяют периодически зарабатывать бонусы. Наиболее прибыльно соревноваться за призы и лотереях, которые проводятся регулярно. Игроки получают шанс не только проявить азартную стратегию, но и вероятность сорвать крупные денежные призы, дополнительные деньги и специальные подарки. Надёжность платформы Pinco онлайн-клуб гарантирует защиту клиентов. Платформа использует передовые алгоритмы безопасности, что гарантирует защиту персональных данных и финансовых транзакций. Кроме того, пользователи могут воспользоваться множество удобных способов внесения денег и вывода выигрышей, через платёжные системы, виртуальные платёжные системы и биткоин-кошельки. Отдел помощи функционирует без перерывов, клиенты имеют возможность обратиться за консультацией когда потребуется. Сотрудники быстро реагируют на запросы и оказывают профессиональную поддержку, по игровым аспектам, бонусами или платежами. Итог Pinco игровая площадка – это идеальное место для любителей разнообразные игровые возможности, выгодные бонусные предложения и отличное обслуживание. Подписка на официальный Telegram-канал гарантирует доступ к уникальным предложениям, огромный каталог слотов и специальные возможности сделают игровой процесс ещё интереснее. Независимо от того, новичок вы или опытный игрок, вы точно подберёте себе идеальную игру и испытать волнение азарта от захватывающих ставок. https://t.me/pinco_official_online/ pinko официальный сайт казино
WilbertCog
Рейтинг топ-20 лучших компаний по ремонту квартир в 2025 году с ценами под ключ, хорошей репутацией, отзывами, сайтами <a href="https://ekspert-remonta.blizko.kz/">отзывы о работе ремонт квартир Алматы</a>
WayneSaw
Частенько бонусные коды раздаются и во время значимых событий. Вся актуальная информация публикуется на канале в Telegram и её можно найти на тематических ресурсах, посвящённых беттингу <a href="https://podarishans.uz">мостбет казино</a>
DavidNet
Современные веб-приложения требуют не только красивого интерфейса, но и надежного, масштабируемого backend-а. Именно он отвечает за хранение данных, бизнес-логику <a href="https://shkolnie.ru/">https://shkolnie.ru/</a>
Bryanboync
Everything about medicine. <a href=" https://gabapentinpharm24.top/# ">gabapentin indications use</a> All trends of medicament.
Bryanboync
Everything what you want to know about pills. <a href=" https://cipropharm24.top/# ">can i get cheap cipro no prescription</a> They provide a global perspective on local health issues.
Bryanboync
Efficient, reliable, and internationally acclaimed. <a href=" https://lisinoprilpharm24.top/# ">can you get generic lisinopril price</a> Global expertise that's palpable with every service.
HaroldRes
Чтобы успешно войти в профессию или повысить квалификацию, важно выбрать качественное обучение, которое даст не только базовые знания, но и актуальные навыки, востребованные на рынке <a href="https://expert-rating.ru/luchshie-kursy-po-frontend-razrabotke-kak-vybrat-obuchenie/">https://expert-rating.ru/luchshie-kursy-po-frontend-razrabotke-kak-vybrat-obuchenie/</a>
Philipiroft
Для безопасной эксплуатации прицепа необходима регулярная экспертиза. Проведите тщательный осмотр перед началом сезона, чтобы убедиться в его исправности. Особое внимание уделите колесам, тормозам и световым приборям <a href="http://wisdomtarot.tforums.org/viewtopic.php?f=5&t=20106">http://wisdomtarot.tforums.org/viewtopic.php?f=5&t=20106</a>
Normanfib
Жилой комплекс «Поляна Пик» — это премиальный проект, расположенный в самом сердце Красной Поляны, окружённый величественными горами. Этот комплекс идеально подходит для тех, кто ценит комфорт, стиль и близость к природе <a href="https://xn----7sbzibmfhf0n.site">купить апартаменты в красной поляне сочи</a>
JamesWet
For users who prefer to place bets and play casino games from mobile devices, the issue of using a promo code in the 1XBET mobile application (APK) is relevant <a href="https://ritmohost.com/cpanel/nelp/index.php?1xbet_today_promo_code_bonus_up_to_130.html">https://ritmohost.com/cpanel/nelp/index.php?1xbet_today_promo_code_bonus_up_to_130.html</a>
WilliamKap
Одним из преимуществ 1Го Казино является простота и доступность. Регистрация аккаунта на сайте занимает несколько минут <a href="http://zanasite.free.fr/laripostedumardi/doku.php?id=%D0%B7%D0%B5%D1%80%D0%BA%D0%B0%D0%BB%D0%BE_%D0%BA%D0%B0%D0%B7%D0%B8%D0%BD%D0%BE_1go">1Го Казино</a>
Normannaign
В ассортименте Банда Казино представлен широкий выбор развлечений. Здесь имеются и популярные краш-игры, завоевавшие признание огромного количества игроков <a href="https://forum-otzyvov.ru/threads/avtomaty-banda-casino.314935/">Banda Casino</a>
Michaelrouse
Казино Аркада - это современная онлайн-платформа, которая максимально быстро стала одним из лидеров в игорной индустрии <a href="https://yiquan.org.ru/yiquan/content/arkada-casino-zerkalo">Аркада Казино официальный сайт</a>
MichaelruidA
Я думаю Вы искали именно про Flagman Casino вход или возможно хотите поведать больше про Флагман Казино мобильная версия <a href="https://laclifep.unicap.br/?p=330864">Флагман Казино официальный сайт</a>
Donaldren
Kometa Casino – это игровая среда, где азартные игры сочетаются с новейшими разработками, обеспечивая гостям удобство и стабильность <a href="http://naigle.borda.ru/?1-4-0-00002923-000-0-0-1741297456">Kometa Casino</a>
MatthewNit
Пневмозаглушки используются для надежного перекрытия трубопроводов диаметром от 40 до 2000 мм <a href="https://xn--80aaefhnxhfhoh5dwd.xn--p1ai">оболочки резинокордные</a>
Stevendenda
Whether you are into sporting activities betting, casino video games, or Are living casino action, the 1xBet promo code makes certain you get by far the most out of your very first deposit <a href="https://controlc.com/315d2dfb">https://controlc.com/315d2dfb</a>
DanielHek
This promotion is an excellent way to boost your betting experience, allowing you to bet on cricket, football, and other major sporting events with a larger bankroll <a href="https://share.evernote.com/note/d8616d11-878a-0043-3a22-0ac9f126ae26">https://share.evernote.com/note/d8616d11-878a-0043-3a22-0ac9f126ae26</a>
Woodrowfoome
Motor Casino – это современный игорный клуб, предлагающий широкий выбор развлечений, включая игровые автоматы, карточные игры и live-дилеров <a href="http://tamozhnya-info.ru/news/motor-kazino-motor-casino-igrovye-avtomaty-bonusy-i-mobilnaya-versiya.html">Motor Casino официальный сайт</a>
RonaldLig
Прежде чем принять решение о покупке автомобиля, определите его рыночную стоимость и техническое состояние. Сравните цены аналогичных моделей в интернете и внимательно изучите мнения владельцев <a href="http://nadegda.listbb.ru/viewtopic.php?f=3&t=1436">http://nadegda.listbb.ru/viewtopic.php?f=3&t=1436</a>
DavidAlike
https://mapletopcasinos.online/
KennethRat
Cat Casino — это отличная платформа для любителей азартных игр, которая предлагает множество бонусов и акций. Промокоды Cat Casino позволяют увеличить свои шансы на выигрыш и получить дополнительные преимущества <a href="https://chto-aktualno.forum2x2.ru/t3367-topic#6900">cat casino бездепозитный бонус за регистрацию</a>
Aaronbit
On our site a little more about Sukaaa Casino bonuses, as well as information about Sykaaa Casino official site <a href="http://serrok.kabb.ru/viewtopic.php?f=3&t=662">Сукааа Казино</a>
AnthonyKeedo
Комплексная УЗИ-диагностика всех органов и тканей в» Санкт-Петербургском центре Узи –диагностике» на оборудовнии экспертного класса <a href="https://uzi-diagnostica.ru/#rec864862108">УЗИ в Купчино</a>
Brianwek
Рефинансирование микрозаймов становится важным инструментом для тех, у кого имеется плохая кредитная история. Этот процесс позволяет объединить существующие долги в один займ с более выгодными условиями <a href="https://remontfor-you.ru/raznoe/finansy/vzyat-zajm-bez-propiski-put-k-finansovoj-uverennosti.html">казино мани х</a>
Victoresods
Money Икс Игральный клуб — это эксклюзивная платформа, которая дарит клиентам потрясающие варианты для выигрыша money x казино <a href="http://marbleinvestment.net/bbs/board.php?bo_table=free&wr_id=7269">money x casino бонус</a>
Michaelzok
Ирвин Казино - это место, где азартные игры становятся действительно увлекательными и безопасными. Под брендом Irwin Casino скрывается надежная и проверенная платформа для тех, кто хочет окунуться в мир азарта и развлечений <a href="https://vk.com/@-191158707-irvin-kazino">официальный сайт Ирвин Казино</a>
Jamesped
Капитал Икс Игральный клуб — это эксклюзивная платформа, которая обеспечивает клиентам фантастические возможности для успеха мани х казино <a href="http://www.olangodito.com/bbs/board.php?bo_table=free&wr_id=3592125">money x casino зеркало</a>
WendellBEW
На официальном сайте Мотор Казино любой игрок найдет широкий выбор развлечений: от классических игровых автоматов до современных видеослотов, настольных игр и живых дилеров <a href="http://virtvladimir.ru/forum/topic/41956">Казино Мотор</a>
DanielmydaY
A virtual number is a phone number that is not tied to a specific SIM card and does not require a physical device to operate <a href="https://golossokal.com.ua/porady/pochemu-vyrtualn-e-nomera-ukrayn-ot-hottelecom-luchshee-reshenye-dlia-sviazy.html">https://golossokal.com.ua/porady/pochemu-vyrtualn-e-nomera-ukrayn-ot-hottelecom-luchshee-reshenye-dlia-sviazy.html</a>
RichardInese
How does it work? A virtual number forwards calls to your primary device, allowing you to communicate as if you were using a regular phone <a href="https://rusnews.kharkiv.ua/virtualnye-telefonnye-nomera-polshi-vse-chto-stoit-znat.html">https://rusnews.kharkiv.ua/virtualnye-telefonnye-nomera-polshi-vse-chto-stoit-znat.html</a>
RichardOwept
Bongs have become an integral part of smoking culture, combining functionality and aesthetics. They not only make the process comfortable, but also allow you to reveal all the nuances of the taste of the mixture <a href="https://cobalts.com.ua/kak-vybrat-i-ispolzovat-bongi-dlya-kureniya/">купить бонг</a>
JamesEnefe
в грядущем году открывает двери ко множеству возможностей для играющих. Используя его, вы можете весьма повысить свои шансы на выигрыш, получать добавочные бонусы и чаще наслаждаться увлекающими играми <a href="https://oboyan.7bb.ru/viewtopic.php?id=1821#p17812">промокод kent казино при регистрации</a>
Josephdreaf
Thimble is considered the most affordable accessory, which is popular among lovers of herbal smoking mixtures <a href="http://yoip.com.ua/chto-takoe-bong-y-zachem-on-nuzhen/">бонг</a>
Bernardnib
The Rent Killer is the main antagonist from the 2020 slasher film The Rental <a href="https://cjseg.com">hire a hitman</a>
JustinOrafe
As the credits wrap up, we see the masked killer rush out of a closet to kill the first unsuspecting victim as they sleep <a href="https://cjseg.com">hire a hitman</a>
Rolandweacy
The CoinsBar resource offers one of the most favorable exchange rates on the market <a href="https://reporter.zp.ua/coinsbar-obmin-kryptovalyuty-onlajn.html">онлайн обмінник криптовалют</a>
WilsonPhils
Bonuses and promotions in the bookmaker 1xBet are a great opportunity to get additional benefits from your bets. The showcase of promo codes can offer a variety of promo codes that can be exchanged for prizes or free bets in the game <a href="http://alhambra.bestforums.org/viewtopic.php?f=10&t=57652">http://alhambra.bestforums.org/viewtopic.php?f=10&t=57652</a>
EdwardLot
With each passing year, the world of targeted games becomes more and more exciting, and online casinos continue to delight their subscribers with new opportunities and promotions <a href="http://pokupki.bestforums.org/viewtopic.php?f=12&t=42942">http://pokupki.bestforums.org/viewtopic.php?f=12&t=42942</a>
Davidtup
Before announcing a list of our exclusive products and services with an indication of their features and benefits, we urge you not to even try to write to us, begging to give you these products or provide services for free <a href="https://how-to-kill-yourself.com/">how to commit suicide</a>
GeorgeCIg
Oxys Crema es un tratamiento facial avanzado disponible en varios paises de Latinoamerica como Mexico, Uruguay, Paraguay, Chile y Peru; no se vende en farmacias tradicionales y solo se puede adquirir de forma segura a traves de su sitio web oficial <a href="https://oxyscrema.org/">oxys precio farmacia Guadalajara</a>
JorgehaG
Despite the fact that this advertisement is written in your native language, we communicate in international, English language <a href="https://mercenaries.pw">hire a hitman</a>
JefferyMum
In the online gambling environment, promo codes have become an integral part, offering insiders unique opportunities to receive prizes and promotions <a href="https://chto-aktualno.forum2x2.ru/t3366-topic#6899">https://chto-aktualno.forum2x2.ru/t3366-topic#6899</a>
Darrelguh
1xBet is a well-known online betting platform that is famous for its generous bonuses and attractive offers. If you are looking for a unique gaming experience and additional chances of success, then 1xBet bonuses will be an excellent choice for you <a href="https://mamamia.by/forum/viewtopic.php?p=31961#31961">https://mamamia.by/forum/viewtopic.php?p=31961#31961</a>
Michaelgop
Willkommen in einer Welt voller spannender Casino-Unterhaltung! Entdecke eine gro?e Auswahl an Online Slots, klassischen Tischspielen und Live-Casino-Erlebnissen <a href="https://michaelkiel.com/happy-hugo-casino-benutzererfahrung-anmeldung-und-registrierung.php">https://michaelkiel.com/happy-hugo-casino-benutzererfahrung-anmeldung-und-registrierung.php</a>
Ronaldrop
Автоматизация ресторанов: увеличиваем прибыль и сокращаем затраты. Программа для автоматизации кафе и ресторанов под ключ <a href="https://vc.ru/life/1860698-kak-my-otkryvali-kofeinyu-so-slaboumiem-otvagoi-i-sedymi-volosami">программа для общепита</a>
JamesFonge
Use 1XBET promo code: 1XTAX200 for VIP bonus up to €1950 + 150 free spins on casino and 100% up to €130 to bet on sports. Register on the 1xbet platform and get a chance to earn even more Rupees using bonus offers and special bonus code from 1xbet. Make sports bets, virtual sports or play at the casino <a href="https://webhitlist.com/profiles/blogs/1xbet-promo-code-vip-bonus-up-to-130-2">1xbet promo code bangladesh today</a>
CharliePayor
In the world of online betting and gambling, promo codes have become an integral part of the strategy of players looking for maximum benefit from their bets <a href="https://nastyapoleva.ru/templates/pages/promokod_melbet_bonus_do_15_000_rub.html">https://nastyapoleva.ru/templates/pages/promokod_melbet_bonus_do_15_000_rub.html</a>
Alfreddunda
Нейросеть для написания реферата – это удобный и современный инструмент, который помогает студентам быстро и легко готовить работы по любым учебным дисциплинам. С её помощью можно получить структурированный, грамотный и уникальный текст всего за несколько минут, значительно экономя время на поиске информации и её обработке. Благодаря этому студенты могут уделять больше внимания развитию своих аналитических навыков и освоению новых знаний <a href="http://alstudy.ru/">написать реферат gpt</a>
BernardWorry
Is there a catch in the Kent Casino bonus program? Or can I safely register? I want to create an account, but I am afraid of hidden conditions. For example, restrictions on games or sudden changes in the rules. Maybe someone has already encountered unexpected nuances <a href="https://4p.ru/main/forum/?PAGE_NAME=message&FID=6&TID=7785&MID=60090&result=new#message60090">https://4p.ru/main/forum/?PAGE_NAME=message&FID=6&TID=7785&MID=60090&result=new#message60090</a>
SamuelPauth
Les plateformes de paris sportifs francaises proposent principalement trois categories de bonus de bienvenue, chacune presentant des avantages specifiques selon votre profil de parieur <a href="https://share.evernote.com/note/3bbb4489-14fc-fc38-f658-e9644a55b652">https://share.evernote.com/note/3bbb4489-14fc-fc38-f658-e9644a55b652</a>
MelvinJal
Современный подход к созданию рефератов предлагает нейросеть — инструмент, позволяющий студентам за считанные минуты получать уникальные и грамотно структурированные тексты. Вместо самостоятельного поиска информации и её длительной обработки, учащиеся могут сразу использовать готовые материалы для решения учебных задач любой сложности. Высвободившееся благодаря этому время студенты направляют на углубление знаний и совершенствование аналитических способностей <a href="http://alshkola1.ru/">реферат с помощью chat gpt</a>
Bradleyduari
Kent Casino is a popular online platform that attracts players with profitable bonuses, promotions and promo codes. If you would like to increase your budget and get additional benefits, Kent Casino promo code high roller is what you need <a href="https://fr.beinsaduno.net/index.php?/gallery/image/443-kent-casino-%D0%BF%D1%80%D0%BE%D0%BC%D0%BE%D0%BA%D0%BE%D0%B4-%D0%B1%D0%BE%D0%BD%D1%83%D1%81-260-fs-%D0%B1%D0%B5%D0%B7-%D0%B4%D0%B5%D0%BF%D0%BE%D0%B7%D0%B8%D1%82%D0%B0/">https://fr.beinsaduno.net/index.php?/gallery/image/443-kent-casino-%D0%BF%D1%80%D0%BE%D0%BC%D0%BE%D0%BA%D0%BE%D0%B4-%D0%B1%D0%BE%D0%BD%D1%83%D1%81-260-fs-%D0%B1%D0%B5%D0%B7-%D0%B4%D0%B5%D0%BF%D0%BE%D0%B7%D0%B8%D1%82%D0%B0/</a>
Josephodowl
Look, for quite a long time I was interested in a question about Payout models in the MostBet affiliate program, so that you do not have any problems I can safely say that now the best conditions are on this site <a href="https://xn----7sbooikqbug1eg.xn--p1ai/user/juhumluh/">https://xn----7sbooikqbug1eg.xn--p1ai/user/juhumluh/</a>
HowardSip
Current link BlackSprut Marketplace 2025 <a href="https://bs2beast.cc">bs2best</a>
Davidref
When you have claimed the welcome bonus offer, it is however very important that you go through the terms and conditions of the 1x welcome bonus <a href="https://himki.myqip.ru/?1-11-0-00010221-000-0-0-1743743285">https://himki.myqip.ru/?1-11-0-00010221-000-0-0-1743743285</a>
Водка способы оплаты
Рады приветствовать в Водка Казино — платформа, где азарт сочетается с невероятными бонусами и шансами для выигрыша. У нас каждый игрок найдет свои любимые игры, будь то новичок или опытный игрок. Здесь вы также получите удовольствие, но и множество бонусов. Весь ассортимент игр в Водка Казино имеет высокие коэффициенты возврата, что увеличивает шансы на выигрыш. Мы подготовили уникальные слоты и классические настольные игры, которые делают игровой процесс еще более занимательным и прибыльным. Зачем ждать в очереди? В Водка Казино вы можете быстро зарегистрироваться и удобно пополнять свой счет, не тратя время на лишние шаги, чтобы начать сразу погрузиться в азарт. Мы всегда готовы предложить вам красивые бонусы для того, чтобы вы могли начать игру с дополнительным капиталом. Присоединяйтесь к Водка Казино, чтобы погрузиться в мир азартных игр с высочайшими шансами на успех! Мгновенная регистрация. Щедрые бонусы для первых игроков. Частые турниры и специальные предложения для тех, кто хочет повысить свои шансы на победу. Поддержка 24/7, чтобы помочь вам в любой момент. Мобильная версия. Погрузитесь в азартный мир Водка Казино и проверьте свою удачу! https://vodka-casinosphere.space/
Howardhep
French sports betting platforms mainly offer three categories of welcome bonuses, each with specific benefits depending on your betting profile <a href="https://cajunlens.site/2025/04/04/%d0%bf%d0%be%d0%ba%d0%b5%d1%80%d0%b4%d0%be%d0%bc-%d0%bf%d1%80%d0%be%d0%bc%d0%be%d0%ba%d0%be%d0%b4-%d0%bd%d0%b0-%d0%b4%d0%b5%d0%bf%d0%be%d0%b7%d0%b8%d1%82-%d0%ba%d0%b0%d0%ba-%d0%bf%d0%be%d0%bb%d1%83/">https://cajunlens.site/2025/04/04/%d0%bf%d0%be%d0%ba%d0%b5%d1%80%d0%b4%d0%be%d0%bc-%d0%bf%d1%80%d0%be%d0%bc%d0%be%d0%ba%d0%be%d0%b4-%d0%bd%d0%b0-%d0%b4%d0%b5%d0%bf%d0%be%d0%b7%d0%b8%d1%82-%d0%ba%d0%b0%d0%ba-%d0%bf%d0%be%d0%bb%d1%83/</a>
Terryopimb
The 1xBet welcome bonus is one of the most generous offers in the online betting market <a href="https://oregon-swing-netork.mn.co/posts/82548353?utm_source=manual">https://oregon-swing-netork.mn.co/posts/82548353?utm_source=manual</a>
FelixOptog
1xBet offers a weekly reload bonus system that is particularly advantageous for regular players <a href="https://payhip.com/b/yuL6n">https://payhip.com/b/yuL6n</a>
ClaudeSmomi
<a href="https://continent-telecom.com/virtual-number-ireland">виртуальный номер ирландии</a>
KeithRef
A phone number in the modern world is a second passport. A huge number of services, messengers, social networks, banking are tied to a phone number, and telephone communication is an integral part of business development <a href="https://dronreview.ru/virtualnyj-nomer-telefona-indonezii/">https://dronreview.ru/virtualnyj-nomer-telefona-indonezii/</a>
RolandGlimb
Convenience and accessibility: Virtual numbers can be obtained online in minutes, without leaving home. They are accessible from anywhere in the world where there is internet <a href="https://vitabreath.ru/news-566131-virtualnye-nomera-sovremennoe-reshenie-dlya-obscheniya-i-biznesa.html">https://vitabreath.ru/news-566131-virtualnye-nomera-sovremennoe-reshenie-dlya-obscheniya-i-biznesa.html</a>
Thomasjoutt
Telegram is one of the most popular apps for communication, which has been developed as a private messenger having the emphasis on encryption and security of users’ personal data <a href="https://sms.pro/">Купить симкарту для Telegram</a>
Samuelfouff
http://onlinesloti.ru
JustinSycle
Не знаете, что подарить на день рождения, юбилей или праздник? Сайт <a href="https://hepatitoff.ru/07/04/2025/238488/podarok-na-novosele-kriterii-vybora.html">https://hepatitoff.ru/07/04/2025/238488/podarok-na-novosele-kriterii-vybora.html</a> предлагает готовые решения — от практичных до креативных подарков. Подберите идеальный вариант за пару кликов!
DorseyNenly
For years, Pin Up has delivered thrilling gaming and betting experiences through its premier online casino platform. Whether you’re placing a bet on sports or enjoying games via the Pin-Up app, pinup caters to all players with secure, fast-paced entertainment <a href="https://pin-up1.ec/">pinup concept</a>
Ronaldfet
<a href=https://athens-rentalcars.com/ru/car-hire-thessaloniki-airport/>аренда машины в греции салоники</a>
Orvillevaw
Mycelium has earned a reputation as a robust and protected handheld Bitcoin wallet, serving to both novice and expert users <a href="https://mycelium-wallet.en.uptodown.com/android">mycelium wallet</a>
LesterJaita
Изготовление металлических значков методом химического травления позволяет создавать изделия с высокой детализацией и долговечностью <a href="https://orhimkom56.ru/izgotovlenie-metallicheskih-znachkov-metodom-himicheskogo-travleniya-iskusstvo-detalizaczii-i-dolgovechnosti/">https://orhimkom56.ru/izgotovlenie-metallicheskih-znachkov-metodom-himicheskogo-travleniya-iskusstvo-detalizaczii-i-dolgovechnosti/</a>
ClintonDrese
For years, Pin-Up has delivered premium betting, casino thrills, and the pinup app for seamless online gaming worldwide <a href="https://zakirhusainpgeve.in/">pin up casino app for android</a>
DanielRog
Baltour — блог о путешествиях с характером. Исследуем города, природу, маршруты и неожиданные места — по Балтике и не только. Без шаблонов, с душой и реальными впечатлениями <a href="https://baltour.ru/">https://baltour.ru/</a>
DavidExids
Vulkan Vegas is a casino known for its reliability and quality service. In 2025, Vulkan Vegas continues to delight players with a variety of games and convenient conditions for playing in rubles <a href="https://mandarintherapist.com/archives/7594">рейтинг казино</a>
Oscarfar
ТОП-10 лучших сервисов для WhatsApp-рассылки WhatsApp является одним из самых популярных мессенджеров в мире, с миллиардами активных пользователей <a href="https://marketing-i.ru/">https://marketing-i.ru/</a>
EddieCax
The authorization process at Arkada Casino is as simple as possible. The player needs to enter an email and password, after which he gets access to his personal account <a href="https://www.lucru.valeasiretuluidesus.ro/blog/2025/03/20/%d0%b0%d1%80%d0%ba%d0%b0%d0%b4%d0%b0-%d0%ba%d0%b0%d0%b7%d0%b8%d0%bd%d0%be-%d0%b7%d0%b5%d1%80%d0%ba%d0%b0%d0%bb%d0%be-%f0%9f%8e%b0-%d0%b0%d0%ba%d1%82%d1%83%d0%b0%d0%bb%d1%8c%d0%bd%d1%8b%d0%b9-%d0%b4/">официальный сайт казино Аркада</a>
VincentTox
The application is available for Android and iOS, providing quick access to the gameplay. Simple installation and user-friendly interface will make the game comfortable, and the mobile version will allow you to enjoy gambling entertainment anywhere <a href="https://www.estestvenkamak.com/2025/04/10/%f0%9f%8e%b0-%d0%b1%d0%b0%d0%bd%d0%b4%d0%b0-%d0%ba%d0%b0%d0%b7%d0%b8%d0%bd%d0%be-banda-casino-%d0%b2-2025-%d0%b3%d0%be%d0%b4%d1%83-%d0%bd%d0%be%d0%b2%d1%8b%d0%b5-%d0%b2%d0%be%d0%b7%d0%bc%d0%be/">Банда Казино 2025</a>
Jamescek
Mobile phone numbers in South Korea also follow a specific structure. South Korean mobile phone numbers usually start with 010 and consist of 11 digits in total <a href="https://www.readability.com/leveraging-saudi-arabia-virtual-phone-numbers-for-business-and-verification">https://www.readability.com/leveraging-saudi-arabia-virtual-phone-numbers-for-business-and-verification</a>
Willieeruct
Jetton Casino pleases its users with a variety of bonuses. For newcomers, there are welcome packages, including deposit incentives and free spins <a href="https://www.sharonsrl.it/%D0%B4%D0%B6%D0%B5%D1%82%D1%82%D0%BE%D0%BD-%D0%BA%D0%B0%D0%B7%D0%B8%D0%BD%D0%BE-%D0%B8-jetton-casino-%D1%80%D0%B5%D0%B3%D0%B8%D1%81%D1%82%D1%80%D0%B0%D1%86%D0%B8%D1%8F-%D0%B8-%D0%B2%D1%85%D0%BE%D0%B4/">Казино Jetton регистрация</a>
Keithvag
Nowadays, international communication is of great importance in both personal and business life. Especially in a country like South Korea, which is important in terms of technology and trade, communicating starts with knowing the correct phone numbers and codes <a href="https://tekraze.com/rent-a-phone-number-rental-service-virtual-numbers/">https://tekraze.com/rent-a-phone-number-rental-service-virtual-numbers/</a>
Anthonytox
детективное агентство экспертного уровня, при этом мы гарантируем одинаково внимательный подход как корпоративным клиентам, так и частным лицам <a href="http://justkidding-me.com">Заказать детектива</a>
официальный сайт казино Комета
Откройте для себя мир азарта в Kometa Casino — уникальное онлайн-казино, где представлены популярные слоты, классические настольные игры, а также эксклюзивные предложения, которые помогут получить максимум от игры! Kometa casino скачать. Какие преимущества у Kometa Casino? Мгновенные выплаты без скрытых платежей. Разнообразие развлечений от классики до новинок. Эксклюзивные предложения, повышающие шансы на победу. Присоединяйтесь к Kometa Casino и почувствуйте настоящий азарт! https://kometa-777-spin.bond/
WalterCaf
Официальный сайт казино Monro. Регистрация и вход в личный кабинет. В этом казино разрешается играть без регистрации, если использовать демо-режим <a href="https://xn--365-5cd9aglpjefbfv.xn--p1ai">казино монро игровые автоматы</a>
Johnniemed
How can you use random eggs and how hot can they be used in the world? What is the most popular version of Casino Ramenbet mobile version <a href="https://www.slagerij-trosbeiaard.be/2025/03/20/%d0%ba%d0%b0%d0%b7%d0%b8%d0%bd%d0%be-ramenbet-%d1%81%d1%82%d0%b0%d0%b2%d0%ba%d0%b8-%d0%bd%d0%b0-%d1%81%d0%bf%d0%be%d1%80%d1%82-%d0%b1%d0%be%d0%bd%d1%83%d1%81%d1%8b-%d1%80%d0%b5%d0%b3%d0%b8/">Раменбет казик</a>
AnthonyOxicy
Assortment of slots one of the silent stores of Triks Casino. This is the case — and the Trix Casino is not limited to its one-size-fits-all store <a href="https://agrolegasa.com/2025/04/04/%f0%9f%8e%af-%d1%82%d1%80%d0%b8%d0%ba%d1%81-%d0%ba%d0%b0%d0%b7%d0%b8%d0%bd%d0%be-%d0%b8-trix-casino-%d1%81%d1%82%d0%b0%d0%b2%d0%ba%d0%b8-%d0%bd%d0%b0-%d1%81%d0%bf%d0%be%d1%80%d1%82-%d0%be/">Trix Casino ставки на спорт</a>
Andreweneft
Оптовый интернет - магазин керамический плитки и керамогранита <a href="https://alliance-plitka.ru">Керамогранит оптом</a>
StevenVox
Promo Code Use: Promo codes provide additional chances to win but may have wagering requirements and time limitations <a href="https://linkmate.mn.co/posts/82578114?utm_source=manual">https://linkmate.mn.co/posts/82578114?utm_source=manual</a>
AnthonyZed
My-articles-online <a href="https://my-articles-online.com/">робота для кілера</a>
BrianFep
Оптовый интернет - магазин керамический плитки и керамогранита alliance-plitka <a href="https://alliance-plitka.ru">Керамогранит оптом</a>
VictorTotly
All links are in the description! (that mean - here) Valve want us to use Steam Guard Mobile Authenticator at all cost <a href="https://sdasteam.com/">скачать steam desktop authenticator</a>
CharlesCam
Steam Desktop Authenticator (SDA) is an open source program that is designed to use two-factor mobile authentication steam without a mobile application <a href="https://authenticatorsteamdesktop.com/">https://authenticatorsteamdesktop.com/</a>
Kennethesota
A suspected Russia-based cybercriminal decided to clone the website of a legitimate open-source desktop app (see here) called Steam Desktop Authenticator (SDA <a href="https://authenticatorsteamdesktop.com/">download steam desktop authenticator</a>
Donaldnoito
SteamGuard mobile authenticator authorization codes directly in your browser! Now you do not need to reach for your phone whenever Steam requests authorization <a href="https://sdasteam.com/">https://sdasteam.com/</a>
JosephVat
Если вы планируете поездку в Италию, первым шагом становится определение необходимой визы. Для граждан стран, не входящих в Шенгенскую зону, обязательно оформлять визу для въезда <a href="http://forum.enigmaprotector.com/viewtopic.php?t=18572">http://forum.enigmaprotector.com/viewtopic.php?t=18572</a>
Edwardchago
Choosing an online casino that doesn’t require verification can streamline your gaming experience <a href="http://jinos.com/bbs/board.php?bo_table=free&wr_id=2560578">http://jinos.com/bbs/board.php?bo_table=free&wr_id=2560578</a>
Williamvag
Whether you’re eyeing a Premier League upset or chasing jackpots on vibrant slots, this exclusive offer sets you up for success <a href="https://calisthenics.mn.co/posts/83188453?utm_source=manual">https://calisthenics.mn.co/posts/83188453?utm_source=manual</a>
JamesOrism
This promo code grants new players a 100% bonus on their first deposit, up to 15,600 BDT. This offer is designed to enhance your betting experience, allowing you to get extra funds as soon as you make your initial deposit <a href="https://minecraftcommand.science/forum/discussions/topics/1xbet-promo-code-free-best-offers-today">https://minecraftcommand.science/forum/discussions/topics/1xbet-promo-code-free-best-offers-today</a>
Clydeflumb
Джойказино: мир азарта и больших возможностей!Погрузитесь в атмосферу ярких эмоций! Сотни слотов, live-игры с реальными дилерами, турниры с призами — выбирайте развлечения по вкусу. Регистрация за пару кликов, бонусы для всех игроков и моментальные выплаты. Лицензия гарантирует честность, а поддержка работает круглосуточно. Удобный интерфейс и мобильная версия оценят даже новички <a href="https://www.vevioz.com/post/1408930_live-dilery-v-onlajn-kazino-budushee-azartnyh-igr-onlajn-kazino-dolgoe-vremya-as.html#">https://www.vevioz.com/post/1408930_live-dilery-v-onlajn-kazino-budushee-azartnyh-igr-onlajn-kazino-dolgoe-vremya-as.html#</a>
JamesGreat
Are you ready to feel thrilling emotions playing one of the best crash games ever <a href="https://krishnachildrenhospital.in/">1win aviator real or fake</a>
WilliamFiect
Promo Code Use: Promo codes provide additional chances to win but may have wagering requirements and time limitations <a href="https://my.omsystem.com/members/1xbetwelcome254">1xbet promo code for registration pakistan</a>
MichealSycle
Promo Code Use: Promo codes provide additional chances to win but may have wagering requirements and time limitations. Ensure to check the terms and conditions <a href="https://kenyabonus.com/">https://kenyabonus.com/</a>
Williambag
Discover thousands of offerings — from free courses to full degrees — delivered by world-class partners like Harvard, Google, Amazon and more <a href="https://auiator.in/">SEO BACKLINKS, BLACK-LINKS, TRAFFIC BOOST, LINK INDEXING – TELEGRAM @SEO_ANOMALY</a>
Davidreoff
One of the key benefits of time-based rewards is the sense of progression they provide <a href="https://imageevent.com/zieme223/crazytimeforecast">https://imageevent.com/zieme223/crazytimeforecast</a>
Tylergon
1xCasino welcome bonus is a package active across your first four deposits. New customers will claim up to €2205/$2420 <a href="https://theplayoffs.news/en/1xbet-bonus-code/">1xcasino promo kodu</a>
RaymondREK
Discover thousands of offerings — from free courses to full degrees — delivered by world-class partners like Harvard, Google, Amazon and more <a href="https://aviator-games-in.com/">BLACK SEO LINKS, BACKLINKS, SOFTWARE FOR MASS BACKLINKING — TELEGRAM @SEO_LINKK</a>
RobertOdogs
Это довольно короткий рассказ о девушке с необычной профессией. Марго – профессиональный киллер <a href="http://stickyday.com">как киллеры находят заказы</a>
Bryantus
Roller garage doors are easy to use, especially when you have a garage remote door system <a href="https://faceout.mn.co/posts/83267908?utm_source=manual">https://faceout.mn.co/posts/83267908?utm_source=manual</a>
eduobuche
Научитесь свежей специальности, пройдите онлайн курс! https://chudesenka.ru/6719-kak-vybrat-buduschuyu-professiyu-poshagovoe-rukovodstvo-k-osoznannomu-resheniyu.html
RogerDaync
What if you double your funds before even placing your first bet? With the 1xBet promo code 1XBRO200, new players can kick-start their adventure with a 100% welcome bonus <a href="https://webyourself.eu/blogs/1042485/Code-Promo-1xBet-RDC-100000-CDF-gratuit">https://webyourself.eu/blogs/1042485/Code-Promo-1xBet-RDC-100000-CDF-gratuit</a>
StuartEvend
The service will help you to attract the indexing robots of Google search engine (Googlebot) and get indexed your web page or backlinks faster <a href="https://aviator-games-in.com/">Online course — SEO for gambling in Turkey. TG — @helena_kaya</a>
Latashia
Добро пожаловать в Клубника Казино, где каждый игрок найдет для себя идеальные условия для выигрыша и наслаждения игрой. Мы предлагаем широкий выбор игр, включая классические слоты, рулетку, блэкджек и уникальные игры с живыми дилерами. В Клубника Казино мы гарантируем полную безопасность и прозрачность всех процессов, чтобы ваши данные и средства были в надежных руках. Почему стоит играть именно в Clubnika бонусы на регистрацию? Мы предлагаем щедрые бонусы и акции, чтобы каждый игрок мог увеличить свои шансы на победу и насладиться игрой. Кроме того, мы обеспечиваем быстрые выводы средств и круглосуточную поддержку, чтобы вы могли сосредоточиться на игре. Когда стоит начать играть в Клубника Казино? Зарегистрируйтесь в Клубника Казино и получите бонусы, которые сразу увеличат ваши шансы на победу. Вот что вас ждет: Щедрые бонусы и бесплатные спины для новых игроков. Промо-акции и турниры с крупными призами. Каждый месяц мы обновляем наш ассортимент игр, добавляя новые интересные слоты и настольные игры. Клубника Казино – это идеальное место для тех, кто хочет играть и выигрывать.
Lancejourn
Throughout this review, we will describe the advantages and benefits of betting on 1xBet from Argentina, as well as tell you a little about the brand, its promotions, and how to use these promo codes on its platform to take advantage of its promos <a href="https://penzu.com/p/642d64c7141501b6">https://penzu.com/p/642d64c7141501b6</a>
ManuelWrict
One of these tools is bonuses, with the help of which you can quickly get the attention of players, increase the interest of users in your own gaming product <a href="https://cesar.pe/wp-content/pgs/el-codigo-promocional-1xbet_bono_100.html">https://cesar.pe/wp-content/pgs/el-codigo-promocional-1xbet_bono_100.html</a>
eduobuche
Обучитесь новой профессии, пройдите онлайн экспресс-курс! https://citysakh.ru/news/slim/118354
Charlesskack
1xBet — download the app for Android and iOS. The 1xBet app allows millions of players from all over the world to place sports bets as quickly as possible <a href="https://www.gabitos.com/eldespertarsai/template.php?nm=1745148915">https://www.gabitos.com/eldespertarsai/template.php?nm=1745148915</a>
DavidPak
Melbet is not just a casino, but also a bookmaker platform with bets on popular sports: football, basketball, tennis, hockey and others <a href="https://minecraftcommand.science/forum/discussions/topics/code-promo-melbet-inscription-bonus-jusqu-a-1-750">https://minecraftcommand.science/forum/discussions/topics/code-promo-melbet-inscription-bonus-jusqu-a-1-750</a>
Darrelexali
Производитель прозрачных силиконовых скатертей гибкое стекло на современном оборудовании с доставкой по всей России <a href="https://dj-shop.ru/category/skaterti-prozrachnye/">Прозрачная скатерть недорого</a>
Daniellon
Ищете выгодные предложения в агропромышленности? Добро пожаловать на АгроПартнер.су <a href="https://agropartner.su/sales/aghrokhimiia.html">https://agropartner.su/sales/aghrokhimiia.html</a>
eduobuche
Online clicker for kids in browser! https://pervomajskoe.net/articles/the-rise-of-online-gaming-exploring-the-world-of-playgama.html
Albertspows
Скатерть из силикона от производителя является абсолютно безопасной. Она не испаряет токсичных соединений <a href="https://dj-shop.ru/">Тут</a>
eduobuche
Online clicker for kids in browser! https://all4webs.com/barry/iogames.htm?6952=56586
eduobuche
Online clicker for kids in browser! https://newpawsibilities.com/top-10-browser-based-io-games-for-competitive-players/
DerrickObsem
Elite Link Indexer is the top choice among digital marketing agencies looking to maximize the number of backlinks indexed for their clients <a href="https://howtokillyourself.substack.com/p/how-to-kill-yourself-best-ways-to">how to kill yourself</a>
eduobuche
Online clicker for kids in browser! https://www.storeboard.com/blogs/gaming/best-games-for-kids-to-play-online-in-browser/5905903
Bryan Parker
Hola hermanos, queria compartir mi experiencia personal con una de las cepas que mas me ha sorprendido ultimamente: las Magnum Buddha Seeds. https://www.oneidauniversity.com/
Joel William
Workout Playlist Upgrade: Alisha Larry’s Cover Is Your New Power Song. Need a high-energy boost? https://www.dentonhighschool.org/
JeffryNip
Нужен срочный вызов сантехника в Алматы? Профессиональные мастера оперативно решат любые проблемы с водопроводом, отоплением и канализацией. Доступные цены, выезд в течение часа и гарантия на все виды работ <a href="https://vyzov-santehnika-almaty.kz/">услуги сантехника</a>
AnthonyTut
Цены на сантехнические услуги формируются в зависимости от сложности работ, типа оборудования, объема и времени выезда <a href="https://vyzov-santehnika-almaty.kz/">сантехник на дом вызвать недорого</a>
Williamwal
Нужен срочный вызов сантехника в Алматы? Профессиональные мастера оперативно решат любые проблемы с водопроводом, отоплением и канализацией. Доступные цены, выезд в течение часа и гарантия на все виды работ <a href="https://vyzov-santehnika-almaty.kz/">сантехник на дом вызвать недорого</a>
Mariokat
Услуги сантехника Алматы. Все виды сантехнических услуг. Получите бесплатную консультацию по ремонту за 5 минут <a href="https://vyzov-santehnika-almaty.kz/">https://vyzov-santehnika-almaty.kz/</a>
Chesterwaw
http://gost-10303.ru/
FrankDiz
Hitman World of Assassination brings together the best elements of Hitman <a href="https://justpaste.it/gsbpk">hire a hitman</a>
Jeremytelia
The Assassin seeks a path to peace, although he himself allows murder <a href="https://pastelink.net/lvv3vqyc">How to get rid of a person</a>
StevenGrada
Promo Code Use: Promo codes provide additional chances to win but may have wagering requirements and time limitations. Ensure to check the terms and conditions <a href="https://1xbetbangla.technetbloggers.de/promo-code-for-1xbet-vip-bonus-up-to-eu130">https://1xbetbangla.technetbloggers.de/promo-code-for-1xbet-vip-bonus-up-to-eu130</a>
Jasonareby
аренда яхты греция <a href="https://european-yachts.com/rent-yacht-greece">https://european-yachts.com/rent-yacht-greece</a>
Ernestinace
Melbet isn’t just a betting site—it’s a global leader trusted by millions of players worldwide <a href="https://phat4life.mn.co/posts/activez-votre-iptv-en-moins-de-5-minutes/comments/129373099?utm_source=manual">https://phat4life.mn.co/posts/activez-votre-iptv-en-moins-de-5-minutes/comments/129373099?utm_source=manual</a>
Georgenen
Active players can earn promotional points through gameplay and exchange them for additional codes, offering further opportunities for bonuses <a href="https://qna.habr.com/user/xbetindia1">https://qna.habr.com/user/xbetindia1</a>
TylerKah
Seize the moment and you will be able to win a lot of money to realize your dreams <a href="https://bookmark.youmobs.com/1xbet-promo-code-today-use-1xwap200-to-get-e130/">https://bookmark.youmobs.com/1xbet-promo-code-today-use-1xwap200-to-get-e130/</a>
EdwardJep
Active players can earn promotional points through gameplay and exchange them for additional codes, offering further opportunities for bonuses <a href="https://a1xbetwelcome.hashnode.dev/1xbet-promo-code-india-today-bonus-100-up-to-130">https://a1xbetwelcome.hashnode.dev/1xbet-promo-code-india-today-bonus-100-up-to-130</a>
RobertGag
French sports betting platforms mainly offer three categories of welcome bonuses, each with specific benefits depending on your betting profile <a href="https://dev.to/code1xbet/activer-code-1xbet-bonus-100-jusqua-130eu-2ide">https://dev.to/code1xbet/activer-code-1xbet-bonus-100-jusqua-130eu-2ide</a>
Danielsuche
Наши эксперты с академическим опытом подготовят дипломную работу любой тематики «под ключ» — от исследования до оформления по ГОСТ. Гарантируем полную уникальность, соответствие всем требованиям и точное соблюдение сроков <a href="https://dplm24.ru/">диплом написать</a>
YourApart
Mortgage calculator USA https://clinicalpsychologistme.com/userinfo.php?userinfo=francine_nyholm_426848&com=profile&name=Your_Account&op=userinfo&mod=space
Josephhot
Virtual used numbers for Telegram verification are available instantly and can be accessed from any location <a href="https://wutdawut.com/read-blog/35345">https://wutdawut.com/read-blog/35345</a>
JasonInine
Команда опытных авторов разработает дипломную работу любой дисциплины с учётом методических указаний вашего вуза <a href="https://topdiploms.ru/">купить дипломную работу москва</a>
ChesterSed
<a href=https://kitehurghada.ru/>Кат Египет</a>
PhilipSpats
Жилищные споры в Алматы — не редкость. Ошибки в квитанциях, некачественные услуги, затопления, конфликты с управляющими компаниями — всё это требует юридической поддержки <a href="http://acglingyu.vip/home.php?mod=space&uid=11795&do=profile">http://acglingyu.vip/home.php?mod=space&uid=11795&do=profile</a>
Jerryreity
Now you know where the ten city region of Decapolis is <a href="https://www.kidsbiblemaps.com/tyre-and-sidon.html">where was tyre and sidon</a>
DavidCox
значок металлический круглый <a href=https://izgotovlenie-znachkov-moskva.ru/>изготовление значков из металла</a>
Josephbig
Каталог готовых фирм - купите юр лицо ООО в Москве недорого с историей и оборотами, расчетным счетом и без долгов, в продаже 1500+ готовых фирм <a href="https://biznesfirma.ru">купить ооо в москве</a>
BrianVes
Все Фрибеты за регистрацию без депозита 2025 и бонусы от букмекерских контор (БК) на одном сайте. Жми <a href="https://fribety.ru">бонус за регистрацию в бк</a>
DavidTek
That is why it is important to approach the choice consciously, taking into account the character, hobbies and lifestyle of a friend <a href="https://7starmovies.co.in/pgs/pro_filym_horisty.html">https://7starmovies.co.in/pgs/pro_filym_horisty.html</a>
FrankCed
<a href=https://t.me/ferixdi_digital>Яндекс плюс подписка</a> Яндекс – это не просто поисковая система, это целая экосистема, пронизывающая все сферы нашей цифровой жизни. И ключом к максимуму возможностей этой экосистемы является Яндекс Плюс. Но как получить этот заветный ключ? Ответ прост – Яндекс Инвайт. Инвайт – это персональное приглашение, открывающее доступ к премиальным функциям и эксклюзивным предложениям Яндекс Плюс. Это ваш шанс на год забыть об ограничениях и наслаждаться всеми преимуществами подписки.
LarryJaw
<a href=https://translatespb.ru/>https://translatespb.ru/</a>
WilliamOxisp
When choosing the right garage tiles, you need to consider many factors, including the classification, known as the tile grade <a href="https://bikersrights.com/articles/kak_sdelaty_spalynyu_udobnoy_5_sekretov.html">https://bikersrights.com/articles/kak_sdelaty_spalynyu_udobnoy_5_sekretov.html</a>
KennethAnene
Заказать корпоративные, сувенирные или памятные значки можно на сайте https://znaknazakaz.ru/ — профессиональное производство и индивидуальный подход.
LouisUterm
<a href=https://mentorfortheboss.com/>Повышение продаж</a> Как собрать эффективную команду? Эффективная команда — основа успешного бизнеса. Начните с подбора людей, которые разделяют ваши ценности и цели. Создайте атмосферу доверия и открытости, где каждый может высказать свое мнение. Установите четкие роли и обязанности, чтобы избежать путаницы. Регулярно проводите командные встречи для обсуждения прогресса и решения проблем. Это поможет вам создать сплоченную и продуктивную команду.
JamesGem
<a href=https://znaknazakaz.ru/>значки на заказ</a> В мире, где детали определяют имидж, значки на пиджак становятся не просто аксессуаром, а мощным инструментом самовыражения. Заказать металлические значки – значит подчеркнуть свою индивидуальность и принадлежность к определенному сообществу.
Williamdup
календарь март 2025 печать <a href=https://pechat-plakatov-spb.ru/>календарь печать спб</a>
MurrayEvoxy
сделать табличку из пластика <a href=https://tablichki-pvh.ru/>таблички из пластика</a>
StuartLiaph
печать наклеек золотом <a href=https://pechat-nakleek2.ru/>печать бумажных наклеек</a>
Mauricetap
печать плаката а2 цена <a href=https://pechat-plakatov-spb.ru/>стоимость печати плакатов</a>
Martincox
Горизонт - апарт отель бизнес класса, главным достоинством которого является расположение на первой береговой линии Черного моря <a href="https://xn-----6kcnufck5ahccutn7f.xn--p1ai">жк горизонт адлер последние</a>
Williamacele
изготовление стендов спб <a href=https://izgotovlenie-stendov2.ru/>изготовление стендов</a>
Georgetit
<a href=https://www.vesper.ru/presscenter/articles/chastotnyy-preobrazovatel-kak-sredstvo-povysheniya-effektivnosti-nasosov/>частотник для скважинного насоса</a> Преимущества Использования Частотного Преобразователя Внедрение частотного преобразователя обеспечивает плавный пуск и остановку насоса, что существенно снижает гидравлические удары в системе водоснабжения. Это, в свою очередь, продлевает срок службы насоса, трубопроводов и запорной арматуры.
Orlandojuift
Below is an outline of how the SOFTSWISS Casino Platform can help iGaming operators and casino websites with SEO and organic user acquisition <a href="https://1winonline.ci/">SEO BACKLINKS, CROSS-LINKS, HACKED WP-ADMIN – TELEGRAM @SEO_ANOMALY</a>
Charlesirrag
A virtual number for VK is a unique technology that allows you to register and confirm your account without using your personal phone <a href="https://svodnews.kr.ua/virtualnyj-nomer-ukrainy-komu-i-kogda-budet-interesen.html">https://svodnews.kr.ua/virtualnyj-nomer-ukrainy-komu-i-kogda-budet-interesen.html</a>
Richardguh
Гибкий камень Гибкий камень – это инновационный отделочный материал, сочетающий в себе эстетику натурального камня и удобство в применении. Изготавливается он путем нанесения тонкого слоя песчаника на текстильную основу. Благодаря этому, материал обладает гибкостью и легкостью, что позволяет использовать его для облицовки поверхностей любой сложности, включая криволинейные участки. Гибкий мрамор Гибкий мрамор представляет собой аналог гибкого камня, но в качестве основы используется мраморная крошка. Этот материал отличается более изысканным внешним видом, имитируя текстуру и цвет натурального мрамора. Гибкий мрамор применяется для создания элегантных интерьеров, облицовки каминов, колонн и других декоративных элементов. Облицовка стен Облицовка стен гибким камнем и мрамором – это современное решение для создания уникального дизайна интерьера и экстерьера. Материалы легко режутся и монтируются, не требуют специальной подготовки поверхности. Они устойчивы к перепадам температур, влаге и механическим повреждениям. Благодаря разнообразию цветов и текстур, гибкий камень и мрамор позволяют реализовать любые дизайнерские идеи, от классики до модерна. Облицовка стен этими материалами придает помещению неповторимый стиль и создает атмосферу комфорта и уюта. <a href=https://wallmramor.ru/>облицовка стен</a>
Edwardgoalp
Надёжный обмен валюты <a href=https://valutapiter.ru/>https://valutapiter.ru</a> в СПб — курсы в реальном времени, большой выбор валют, комфортные офисы. Конфиденциальность, без очередей, выгодно и с гарантией. Для туристов, жителей и бизнеса. Обмен, которому можно доверять!
MarcusTeecy
Займы под материнский капитал <a href=https://юсфц.рф/>https://юсфц.рф</a> быстрое решение для покупки квартиры, дома или участка. Без личных вложений, с полным юридическим сопровождением. Оформление за 1 день, надёжные сделки и опыт более 10 лет. Используйте господдержку с умом!
Scottlot
Кредитный потребительский кооператив <a href=https://юк-кпк.рф/>https://юк-кпк.рф</a> разумный выбор для тех, кто ценит стабильность. Выдача займов, приём сбережений, поддержка пайщиков. Всё по закону, без скрытых комиссий и с личным вниманием к каждому участнику.
RogerIromy
When all the preparatory work is completed, you can proceed directly to the wallpaper pasting process <a href="https://pohhuat.com/media/pgs/?postelynoe_belye_iz_tvila.html">https://pohhuat.com/media/pgs/?postelynoe_belye_iz_tvila.html</a>
ByronLof
This guide will take you through the steps of progressing from a beginner to a skilled trekker, ensuring your adventures become more enjoyable and fulfilling <a href="https://www.roundtheworldflights.com/">SEO BACKLINKS, BLACK-LINKS, TRAFFIC BOOST, LINK INDEXING – TELEGRAM @SEO_ANOMALY</a>
MarvinFex
Take the TR Gambling Intensive course – ensure yourself a decent income Learn to understand the core aspects <a href="https://1winonline.ci/">Г‡evrimiГ§i kurs – TГјrkiye’de Kumar (Casino) iГ§in SEO. Telegram – @aysu_kaya</a>
MarvinRew
Предлагаем приобрести диссертацию в Москве напрямую у профильных кандидатов наук, без посредников и скрытых доплат <a href="https://nauchnaya-statya24.ru/">написать диссертацию цена</a>
JohnnyTok
Looking for the best welcome bonus in online betting? 1xBet, a global gambling leader, gives new players an unbeatable 100% first deposit bonus <a href="https://ai.ceo/read-blog/337565">https://ai.ceo/read-blog/337565</a>
Arturotrola
A gift that is too cheap or expensive may be perceived as an insult. It is customary to refuse to accept a gift several times <a href="https://sorthealth.com/wp-content/pgs/?evolyuciya_ofisnogo_prostranstva_ot_kubiklov_k_kreativnym_kovorkingam_i_gibkim_rabochim_z.html">https://writerscolumn.com/articles/assassin&_039;s_creed_odyssey_prohoghdenie_pobochnyh_kvestov_piratskie_ostrova_vse_zadaniya.html</a>
ShawnSkada
Цена рассчитывается индивидуально после оценки темы и методических требований, включает глубокое исследование, оформление по ГОСТ, проверку уникальности и бесплатное сопровождение до защиты — без скрытых доплат и с чёткими сроками <a href="https://kandidatskaya24.ru/">сколько стоит защита кандидатской диссертации</a>
Andreweneft
Подготовим магистерскую диссертацию с нуля — от фундаментального исследования и анализа источников до оформления по ГОСТ и проверки уникальности <a href="https://magisterskaya24.ru/">написание магистерской диссертации на заказ</a>
ErnestIndug
After the child turns one and a half years old, mother's milk is no longer the only essential food, and the woman stops breastfeeding <a href="https://www.imdb.com/fr/list/ls592060892/">https://www.imdb.com/fr/list/ls592060892/</a>
Robertmet
Современные сувениры <a href=https://66.ru/news/stuff/278214/>https://66.ru/news/stuff/278214/</a> всё чаще становятся не просто подарками, а настоящими элементами бренда или корпоративной культуры. Особенно интересны примеры, когда обычные предметы превращаются в креативные и запоминающиеся изделия. Такие подходы вдохновляют на создание уникальной продукции с индивидуальным стилем и глубоким смыслом. Именно за этим всё чаще обращаются заказчики, которым важна не массовость, а оригинальность.
ZacharyAbism
Металлические бейджи <a href=https://gubkin.bezformata.com/listnews/beydzhi-dlya-brendov-i/140355141/>https://gubkin.bezformata.com/listnews/beydzhi-dlya-brendov-i/140355141/</a> для брендов и корпораций — стильное решение для сотрудников, партнёров и мероприятий. Прочные, износостойкие, с гравировкой или полноцветной печатью. Подчёркивают статус компании и укрепляют фирменный стиль. Такие решения особенно актуальны для выставок, форумов и корпоративных событий, где важно произвести правильное первое впечатление. Грамотно оформленный бейдж может сказать о компании больше, чем десятки слов.
Thomasfut
Заказные медали <a href=https://iseekmate.com/34740-medali-na-zakaz-nagrada-dlya-chempionov.html>https://iseekmate.com/34740-medali-na-zakaz-nagrada-dlya-chempionov.html</a> применяются для поощрения в спорте, образовании, корпоративной культуре и юбилейных мероприятиях. Производятся из металла, с эмалью, гравировкой или цветной печатью в соответствии с требованиями заказчика.
StephenQuevy
Хочешь оформить <a href=https://zddoc.ru/tehnicheskiy-pasport-zheleznodorozhnogo-puti-neobshhego-polzovaniya-podezdnogo-puti-razrabotka-i-soglasovanie/>паспорт на жд тупик</a> Документация включает технический паспорт железнодорожного пути, а также технический паспорт жд пути необщего пользования. Отдельно может потребоваться техпаспорт жд и паспорт на жд тупик при ведении путевого хозяйства.
CarlosOwnek
Not a struggle, but a conscious choice Understanding the reasons for cravings for sweets helps to shift the focus from an exhausting struggle to a conscious approach <a href="http://medmall.ru/img/pages/kak_zadelaty_dyry_i_treschiny_v_betonnoy_stene.html">http://medmall.ru/img/pages/kak_zadelaty_dyry_i_treschiny_v_betonnoy_stene.html</a>
RobertDiele
We will also come across the remains of a fort built in the Bronze Age, Early Christian churches and the best Irish pubs <a href="http://megadownload.net/MDT/pgs/?germaniy_sredstvo_ot_starosti.html">http://megadownload.net/MDT/pgs/?germaniy_sredstvo_ot_starosti.html</a>
Richardjaw
Оцениваем объём и сложность темы до старта, сразу фиксируем цену и готовим диссертацию «под ключ» с высокой уникальностью, оформлением по ГОСТ <a href="https://dissertaciyapro.ru/">интернет диссертация</a>
Francispar
Цена рассчитывается индивидуально после оценки темы и методических требований, включает глубокое исследование, оформление по ГОСТ <a href="https://bc-sfedu.ru/">написать диссертацию на заказ цена</a>
Shanestync
Сочетаем мощь современных нейросетей и опытных редакторов, чтобы оперативно собрать источники, сформировать структурированный текст, оформить по ГОСТ и обеспечить высокую уникальность <a href="https://gpt-content.ru/">gpt курсовая работа</a>
Thomasfut
Заказные медали <a href=https://iseekmate.com/34740-medali-na-zakaz-nagrada-dlya-chempionov.html>https://iseekmate.com/34740-medali-na-zakaz-nagrada-dlya-chempionov.html</a> применяются для поощрения в спорте, образовании, корпоративной культуре и юбилейных мероприятиях. Производятся из металла, с эмалью, гравировкой или цветной печатью в соответствии с требованиями заказчика.
ZacharyAbism
Металлические бейджи <a href=https://gubkin.bezformata.com/listnews/beydzhi-dlya-brendov-i/140355141/>https://gubkin.bezformata.com/listnews/beydzhi-dlya-brendov-i/140355141/</a> для брендов и корпораций — стильное решение для сотрудников, партнёров и мероприятий. Прочные, износостойкие, с гравировкой или полноцветной печатью. Подчёркивают статус компании и укрепляют фирменный стиль. Такие решения особенно актуальны для выставок, форумов и корпоративных событий, где важно произвести правильное первое впечатление. Грамотно оформленный бейдж может сказать о компании больше, чем десятки слов.
RodneyKap
Of course, there is a fly in the ointment. The main disadvantage of reusable diapers is the need for washing and drying <a href="https://medcentromsk.ru/files/pages/index.php?nanesenie_yaponskoy_shtukaturki_nedostatki_primeneniya.html">https://medcentromsk.ru/files/pages/index.php?nanesenie_yaponskoy_shtukaturki_nedostatki_primeneniya.html</a>
Duncanlig
The quality of the tools directly affects the result <a href="https://yopensource.com/wp-content/pgs/?anghe_franciya_srednevekovyy_zamok_anghe.html">https://yopensource.com/wp-content/pgs/?anghe_franciya_srednevekovyy_zamok_anghe.html</a>
Jamesmep
Many modern antidepressants are compatible with breastfeeding <a href="https://naziya.ru/images/pgs/generator_i_ego_remeny_tihaya_drama_pod_kapotom.html">https://naziya.ru/images/pgs/generator_i_ego_remeny_tihaya_drama_pod_kapotom.html</a>
JessePiosy
Используем нейросетевые алгоритмы для мгновенного подбора источников, генерации черновика и анализа уникальности, а команда методистов приводит материал к требованиям вашего вуза, оформляет по ГОСТ <a href="https://aifranch.ru/">чат gpt для написания курсовых работ</a>
ThomasNug
Продвинутые нейросети помогают оперативно собирать источники и формировать основу курсовой, а опытные редакторы завершают работу <a href="https://gptgetsmm.ru/">нейросеть пишет курсовую</a>
NormanShoms
Продвижение групп ВК <a href=https://vk.com/dizayn_vedenie_prodvizhenie_grup>https://vk.com/dizayn_vedenie_prodvizhenie_grup</a> от оформления и наполнения до запуска рекламы и роста подписчиков. Подходит для бизнеса, мероприятий, брендов и экспертов. Работаем честно и с аналитикой.
StevenNen
Изготавливаем значки <a href=https://znaknazakaz.ru/>https://znaknazakaz.ru</a> на заказ в Москве: классические, сувенирные, корпоративные, с логотипом и индивидуальным дизайном. Металл, эмаль, цветная печать. Быстрое производство, разные тиражи, удобная доставка по городу.
Carrollgar
Металлические значки <a href=https://techserver.ru/izgotovlenie-znachkov-iz-metalla-kak-zakazat-unikalnye-izdeliya-dlya-vashego-brenda/>https://techserver.ru/izgotovlenie-znachkov-iz-metalla-kak-zakazat-unikalnye-izdeliya-dlya-vashego-brenda/</a> это стильный и долговечный способ подчеркнуть фирменный стиль, создать корпоративную айдентику или просто сделать приятный сувенир. Всё больше компаний выбирают индивидуальное изготовление значков, чтобы выделиться среди конкурентов.
Davidtok
Quer <a href=https://comprarseguidores.io/>compre seguidores no Instagram</a>? Escolha o pacote que mais combina com voce: ao vivo, oferta ou misto. Adequado para blogueiros, lojas e marcas. Seguro, rapido e mantem a reputacao da sua conta.
LouisKaf
Изготовление значков <a href=https://3news.ru/izgotovlenie-znachkov-na-zakaz-pochemu-eto-vygodno-i-kak-vybrat-idealnyj-variant/>https://3news.ru/izgotovlenie-znachkov-na-zakaz-pochemu-eto-vygodno-i-kak-vybrat-idealnyj-variant/</a> на заказ любой сложности. Работаем по вашему дизайну или поможем создать макет. Предлагаем разные материалы, формы и типы креплений. Оперативное производство и доставка по всей России.
Altonprile
Изготовим значки с логотипом <a href=http://classical-news.ru/tehnologiya-izgotovleniya-znachkov-s-logotipom/>http://classical-news.ru/tehnologiya-izgotovleniya-znachkov-s-logotipom/</a> вашей компании. Металлические, пластиковые, с эмалью или цветной печатью. Подчеркните фирменный стиль на выставках, акциях и корпоративных мероприятиях. Качественно, от 10 штук, с доставкой.
Charlesvieva
Значки с логотипом компании <a href=https://press-release.ru/branches/markets/znachki-s-vashim-logotipom-iskusstvo-metalla-voploshchennoe-v-unikalnyh-izdeliyah/>https://press-release.ru/branches/markets/znachki-s-vashim-logotipom-iskusstvo-metalla-voploshchennoe-v-unikalnyh-izdeliyah/</a> это не просто элемент фирменного стиля, а настоящее искусство, воплощённое в металле. Они подчёркивают статус бренда и помогают сформировать узнаваемый образ.
urwork-ru
Юридическое сопровождение <a href=https://urwork.ru/uslugi/bankrotstvo-fizicheskih-licz-yuridicheskie-uslugi/>банкротство физических лиц спб</a>: от анализа документов до полного списания долгов. Работаем официально, по закону №?127-ФЗ. Возможна рассрочка оплаты услуг.
DominicNap
Подбираем актуальные источники, пишем рефераты строго по методичке вашего вуза <a href="https://buhu5.ru/">сделать реферат на заказ</a>
Brucebup
Our top-tier consultants specialize in performance marketing and data analysis <a href="https://aviator-game-official.in/">SEO BACKLINKS, CROSS-LINKS, HACKED WP-ADMIN - TELEGRAM @SEO_ANOMALY</a>
Delbertseeft
Сочетаем экспертный опыт и возможности GPT, чтобы быстро подготовить курсовую работу с глубокой аналитикой <a href="https://forumgpt.ru/">нейросеть написать курсовую</a>
Antoniosouse
Закажите металлические значки <a href=https://metal-archive.ru/novosti/40507-metallicheskie-znachki-na-zakaz-v-moskve-masterstvo-kachestvo-i-individualnyy-podhod.html>https://metal-archive.ru/novosti/40507-metallicheskie-znachki-na-zakaz-v-moskve-masterstvo-kachestvo-i-individualnyy-podhod.html</a> с индивидуальным оформлением. Материалы: латунь, сталь, алюминий. Эмаль, гравировка, печать. Подходит для корпоративных мероприятий, сувениров, символики и наград.
Scottzem
Металлические нагрудные значки <a href=https://str-steel.ru/metallicheskie-nagrudnye-znachki.html>https://str-steel.ru/metallicheskie-nagrudnye-znachki.html</a> стильный и долговечный аксессуар для сотрудников, мероприятий и награждений. Изготавливаем под заказ: с логотипом, гравировкой или эмалью. Разные формы, крепления и варианты отделки.
GroverSlisa
Выполним контрольную работу любой сложности — от точных расчётов и развернутых ответов до оформления по ГОСТ <a href="https://matematiku5.ru/">контрольная на заказ</a>
JeremyEmume
Корпоративные значки <a href=https://electrikexpert.ru/korporativnye-znachki-kak-malenkie-detali-sozdayut-bolshuyu-kulturu/>https://electrikexpert.ru/korporativnye-znachki-kak-malenkie-detali-sozdayut-bolshuyu-kulturu/ это не только стиль, но и имидж. Отличный вариант для персонала, деловых встреч, награждений и брендированных подарков. Предлагаем разные материалы, формы и способы нанесения.
Williamexeks
1xBet code with an exclusive welcome bonus, we present details on how to use the code <a href="http://www.volgogradsky.ru/forum/viewtopic.php?p=1055487#1055487">http://www.volgogradsky.ru/forum/viewtopic.php?p=1055487#1055487</a>
Jacobmus
Выполним курсовую «под ключ» — от подбора темы и анализа источников до оформления по ГОСТ и проверки уникальности, строго соблюдая сроки и предоставляя бесплатные правки <a href="https://juristu5.ru/">курсовые работы</a>
KevinEnage
открыть бизнес в великобритании <a href=https://zaregistrirovat-kompaniyu-england.com/>открыть бизнес в великобритании</a>
Delbertvep
Выполним диплом под ключ — от глубокого исследования и расчётов до оформления по ГОСТ и проверки Антиплагиат, гарантируя конфиденциальность и точное соблюдение сроков <a href="https://vkomforte.su/">написание дипломной работы на заказ</a>
Michaelapold
Подготовим дипломную работу «под ключ» — от разработки структуры и сбора данных до защиты, обеспечив оригинальность, оформление по ГОСТ, бесплатные доработки и строгое соблюдение дедлайна <a href="https://eurekamag.ru/">дипломная работа написать на заказ</a>
HectorNow
If you want to make sure you're choosing the best promo code option to start your betting, check out the comparison table below <a href="https://phat4life.mn.co/posts/about-me-83974648/comments/130197962?utm_source=manual">https://phat4life.mn.co/posts/about-me-83974648/comments/130197962?utm_source=manual</a>
JosephDor
Выполним дипломные работы любого профиля под ключ, учитывая методические требования вуза, обеспечим высокую уникальность, детальные расчёты и оформление по ГОСТ, соблюдём сроки и бесплатно внесём правки до полной защиты <a href="https://ekonomistu5.ru/">помощь в написании дипломной работы</a>
HectorNow
Proven 1xBet casino bonuses: no deposit for registration, free spins, current codes, and promo codes for today <a href="https://articlescad.com/c-digo-promocional-para-1xbet-bono-100-hasta-130-142653.html">https://articlescad.com/c-digo-promocional-para-1xbet-bono-100-hasta-130-142653.html</a>
LarryWrelf
Берём на себя подготовку дипломной работы — от выбора темы и поиска литературы до расчётов, оформления по ГОСТ и проверки уникальности, гарантируя качественный результат точно в срок <a href="https://fiziku5.ru/">написать диплом</a>
HerbertAvath
Создаём рефераты любой сложности с грамотной структурой, актуальными источниками и гарантией оригинальности; выполняем срочные заказы и бесплатно вносим правки до полного принятия <a href="https://textreferatov.ru/">реферат написать на заказ</a>
Michaelboymn
Оперативно пишем рефераты под ключ, точно соблюдая методические требования вуза и форматирование, гарантируем высокую оригинальность, бесплатные правки и сдачу в оговорённый срок <a href="https://referatlira.ru/">реферат купить</a>
Jamesdok
Think of them like your favorite childhood candy, but with a relaxing twist <a href="https://concretesubmarine.activeboard.com/t71884922/cdigo-promocional-registro-1xbet-bono-hasta-130/?page=last#lastPostAnchor">https://concretesubmarine.activeboard.com/t71884922/cdigo-promocional-registro-1xbet-bono-hasta-130/?page=last#lastPostAnchor</a>
Jamesmox
зарегистрировать компанию в англии <a href=https://zaregistrirovat-kompaniyu-england.com/>https://zaregistrirovat-kompaniyu-england.com</a>
WilliamDon
Рейтинг лучших сервисов <a href=https://vc.ru/telegram/1926953-nakrutka-podpischikov-v-telegram>https://vc.ru/telegram/1926953-nakrutka-podpischikov-v-telegram</a> для накрутки Telegram-подписчиков: функциональность, качество, цены и скорость выполнения. Подходит для продвижения каналов любого масштаба — от старта до монетизации.
JerryFroro
Jacuzzi, sauna, hammam <a href=https://spaplanet.net/>https://spaplanet.net/</a> turnkey - full cycle: from design and selection of equipment to finishing and commissioning. We work with any premises. Reliable, aesthetically pleasing and with a guarantee.
LeonardMam
Мы разрабатываем дипломы«под ключ» — от выбора темы и глубокой аналитики до оригинального текста с проверкой Антиплагиат и бесплатными доработками, строго соблюдая сроки и требования вашего вуза <a href="https://prof-elita.ru/">Читать</a>
PeterDuh
открыть бизнес в англии <a href=https://zaregistrirovat-kompaniyu-england.com/>регистрация компании в британии</a>
Williamsoync
<a href="https://easy-remodeling.com/the-best-ways-to-remove-mould-from-bathroom-tiles-step-by-step-guide/">https://easy-remodeling.com/the-best-ways-to-remove-mould-from-bathroom-tiles-step-by-step-guide/</a>
PeterDob
Долгие годы мы готовим дипломные проекты для студентов технических, гуманитарных и экономических вузов, обеспечивая высокую оригинальность <a href="https://interactiveideas.ru/">купить дипломную работу</a>
ThomasMox
Современный и удобный сайт <a href=https://prokhv.ru/>prokhv.ru</a> на котором легко найти нужную информацию, товары или услуги. Простая навигация, понятный интерфейс и актуальное содержание подойдут как для новых пользователей, так и для постоянной аудитории. Работает быстро, доступен круглосуточно.
Kerryadeld
Current 1xBet Casino bonus offers are collected here <a href="http://cs-headshot.phorum.pl/viewtopic.php?p=605182#605182">código promocional 1xbet casino</a>
Johnnybed
Gambling Intensive course – ensure yourself a decent income Learn to <a href="https://dorraraleimanroyal.com/">SEO BACKLINKS, CROSS-LINKS, TRAFFIC BOOST, LINK INDEXING – TELEGRAM @SEO_ANOMALY</a>
MichaelDiunc
cloud server for rent <a href=https://cloud-server1.com/>https://cloud-server1.com/</a>
Kennethpurge
It is available to all beginners who want to become professional players <a href="https://webhitlist.com/profiles/blogs/code-promo-1xbet-bonus-de-bienvenue-130-1">comment crГ©er code promo 1xbet</a>
MatthewmeN
Si quieres asegurarte de estar eligiendo la mejor opcion de codigo promocional para comenzar tus apuestas <a href="https://webhitlist.com/profiles/blogs/c-digo-promocional-1xbet-hoy-bono-vip-130-1">codigo promocional de 1xbet</a>
AlbertSexut
Кейтеринг давно перестал быть просто доставкой еды — сегодня это полноценный сервис, способный превратить любое мероприятие в изысканное гастрономическое событие <a href="https://banket.space/">заказ кейтеринга</a>
Philliprek
Курительная трубка — это не просто способ насладиться табаком, а целый ритуал, требующий внимания к деталям. Чтобы получить максимум удовольствия от процесса, важно подобрать правильные аксессуары: от удобных тамперов до качественных ёршиков и фильтров <a href="https://pair-store.ru/">Читать</a>
Bradytok
After entering the promo code, bonuses appear on the balance <a href="http://c90226sl.beget.tech/2025/05/06/r7-kazino-promokod/">http://c90226sl.beget.tech/2025/05/06/r7-kazino-promokod/</a>
WilliamLew
Навес — практичное решение для тех, кто хочет уберечь автомобиль от солнца, дождя, снега и других капризов погоды, не строя капитальный гараж <a href="https://zabor.space/">недорогие навесы для дачи</a>
Herbertnub
Онлайн проект <a href=https://stv-it.ru/>stv-it.ru</a> где собраны полезные данные, инструменты и сервисы для повседневной жизни и профессиональной деятельности. Сайт адаптирован под любые устройства, стабильно работает и предоставляет максимум пользы без лишнего шума и рекламы.
StevenWhode
cloud server web hosting <a href=https://cloud-server1.com/>cloud server best</a>
Albertgalse
Современный сайт <a href=https://blackmaskfresh.ru/>blackmaskfresh.ru</a> на котором легко найти нужную и полезную информацию, товары или услуги. Простая навигация, понятный интерфейс и актуальное содержание подойдут как для новых пользователей, так и для постоянной аудитории. Работает быстро, доступен круглосуточно.
Jamesnax
average price of heroin <a href=https://tronenergy.market/>where to buy a cocaine warehouse</a>
MarionJah
Car service <a href=https://online-carshop.com/importance-of-ventilation-in-automobiles/>cabin air filter replacement cost</a> services We provide car repair services: from quick diagnostics to major restoration. Quality guarantee, experienced specialists, clear deadlines and original spare parts. We work with private and corporate clients.
Andrewclole
porn lesbians <a href=https://tronsave.io/>buy cocaine in stavropol</a>
Josephbah
«МиграРостов» оказывает консультационную помощь в решении кадровых и миграционных вопросов, помогая работодателям снижать расходы на персонал и устранять любые кадровые и миграционные риски https://autstaffing-rnd.ru/
JamesDoB
porn video sluts <a href=https://itrx.io/en/>where to buy heroin</a>
Marcussiz
Finally, what other 1x promotions and bonuses await players <a href="https://anotepad.com/notes/aec4sdr9">código promocional 1xbet perú</a>
Arthurkex
To enjoy the atmosphere of a real casino in a virtual environment <a href="https://starburstsoccer.com/comprehensive-guide-to-soccer-substitution-rules-for-fans-and-players/">Comprehensive Guide to Soccer Substitution Rules</a>
Josephgek
At the same time, you can use bonus points in a variety of ways <a href="https://daunemas8a.blogspot.com/2025/05/code-promo-1xbet-bonus-exclusif-de-130.html">code promo pour 1xbet</a>
DavidVoice
курсовые купить <a href=https://kursoviehelp.ru/>заказ курсовых работ</a>
JerryApoth
hezbollah hassan <a href=https://tronpulse.io/>buy stash heroin</a>
JasonMit
Geographic Information Systems (GIS) have revolutionized <a href="https://bible-history.com/maps/old-testament-world">map of the old testament</a>
CharlieGuinC
Современные модели также могут включать перколяторы <a href="https://www.04597.com.ua/list/507646">купить гриндер для травы</a>
AaronFak
En la industria del juego, la marca 1xBet es bien conocida <a href="https://penposh.com/blogs/410516/C%C3%B3digo-Promocional-1xBet-Hoy-Bono-de-Bienvenida-130">código promocional 1xbet panama</a>
Normandvum
Предлагаем качественные <a href=https://kss.plus/shop/stupeni-prostupi/klinkernye-stupeni/>плитка для ступеней</a> — ступени и плитка для наружных и внутренних работ. Устойчив к износу, влаге и морозу. Подходит для лестниц, крылец, балконов. Консультации и заказ в один шаг.
CesarGed
Значки из металла <a href=https://all-5.ru/izgotovlenie-metallicheskih-znachkov-metodom-himicheskogo-travleniya/>https://all-5.ru/izgotovlenie-metallicheskih-znachkov-metodom-himicheskogo-travleniya/</a> эффектный способ подчеркнуть корпоративный стиль или отметить событие. Изготавливаем тиражи любого объёма, предоставляем консультации по выбору технологии и креплений.
RobertWat
Предлагаем изготовление <a href=https://deezme.ru/biznes/pochemu-metallicheskie-znachki-premialnogo-kachestva-zakazyvajut-napryamuju-u-proizvoditelya/>https://deezme.ru/biznes/pochemu-metallicheskie-znachki-premialnogo-kachestva-zakazyvajut-napryamuju-u-proizvoditelya/</a> значков из металла под ключ: от идеи и макета до готового изделия. Разнообразие форм, покрытий, технологий. Подходит для организаций, мероприятий и персональных заказов.
Brooksemils
Выбор правильной технологии <a href=https://wfinbiz.com/bez-rubriki/proizvodstvo-premialnyh-znachkov-tehnologii-i-metody-izgotovleniya-znachkov-vklyuchaya-himicheskoe-travlenie-i-ego-preimushhestva/>https://wfinbiz.com/bez-rubriki/proizvodstvo-premialnyh-znachkov-tehnologii-i-metody-izgotovleniya-znachkov-vklyuchaya-himicheskoe-travlenie-i-ego-preimushhestva/</a> ключ к созданию значков, которые действительно производят впечатление. Чтобы значки премиального уровня действительно выглядели достойно, необходимо правильно подобрать технологию производства. Методы, такие как химическое травление, обеспечивают высокую детализацию и благородный внешний вид, который сохраняется надолго.
RobertBiP
Лечение в Китае <a href=https://chemodantour.ru/>стоматология в китае</a> туры в лучшие медицинские центры страны. Традиционная и современная медицина, точная диагностика, восстановление и реабилитация. Сопровождение на всех этапах поездки.
Diegojug
отправить курсовую <a href=http://kursoviehelp.ru/>kursoviehelp.ru/</a>
VernonJox
What makes the multiplier bonus so appealing is its unpredictability <a href="https://zszp8.resman.pl/wp-content/articles/?Sugar_Rush_Slots_A_Sweet_Adventure_in_Online_Gaming.html">https://zszp8.resman.pl/wp-content/articles/?Sugar_Rush_Slots_A_Sweet_Adventure_in_Online_Gaming.html</a>
WayneCrilm
The 1xBet bookmaker has established itself as one of the most generous <a href="https://webyourself.eu/blogs/1179888/РџСЂРѕРјРѕРєРѕРґ-для-1xBet-Приветственный-Р±РѕРЅСѓСЃ-РґРѕ-32-500-RUB">промокод на 1xbet</a>
Twyla
Лев Казино приглашает вас в мир захватывающих игр и невероятных побед. В нашем казино вас ждут не только популярные игры, но и эксклюзивные предложения для всех игроков. Каждая игра в Лев Казино тщательно проверена, и мы делаем все, чтобы ваши данные и средства были в полной безопасности. Почему стоит выбрать онлайн казино для всех? В нашем арсенале только лучшие игры, которые прошли сертификацию и отвечают мировым стандартам. Бонусы, турниры и акции — это шанс увеличить свой банк и сделать игру еще более увлекательной. Просто начните играть, и победа обязательно будет на вашей стороне. Множество бонусов и акций для новых игроков. Постоянные обновления и новинки в игровом каталоге. Поддержка клиентов 24/7. Быстрая регистрация и удобство в пополнении счета. Присоединяйтесь к Лев Казино, станьте победителем и наслаждайтесь каждой минутой игры!.
MarionBox
The most commonly used types of promotional <a href="https://vegetalid.com/files/pgs/?dieta_medikov.html">https://clubgti.com/wp-content/pages/?preimuschestva_i_nedostatki_samostoyatelynoy_moyki_fasada_doma.html</a>
DoyleDen
O site oficial 1win bet <a href=https://1winbr.com.br/>https://1winbr.com.br/</a> e apostar em desporto, casinos, jogos e torneios. Suporte para diversas moedas, transacoes rapidas, promocoes e cashback. Jogue confortavelmente no seu PC ou atraves da aplicacao.
Brendanbence
Celebrating in a restaurant or cafe, or just having a glass <a href="https://hamanoji.jp/wp-content/pgs/detskiy_infantilynyy_akropustulez.html">https://hamanoji.jp/wp-content/pgs/detskiy_infantilynyy_akropustulez.html</a>
Jamestub
India ensures its loyal users are rewarded with frequent promotions <a href="https://ameblo.jp/greenwichodeum/entry-12892983104.html">1xbet promo code free bet</a>
Marvinbon
1xBet promo code <a href=https://judgingthefuture.net/wp-content/pgs/?tainstvennye_reki_na_morskom_dne_chasty_2.html>https://judgingthefuture.net/wp-content/pgs/?tainstvennye_reki_na_morskom_dne_chasty_2.html</a> is an opportunity to get a bonus of up to 100% on your first deposit. Register, enter the code and start betting with additional funds. Fast, simple and profitable.
MartinAdemi
1xBet promo code <a href=https://patrelle.com/pgs/proekty_domov__4.html>https://patrelle.com/pgs/proekty_domov__4.html</a> is your chance to start with a bonus! Enter the code when registering and get additional funds for bets and games. Suitable for sports events, live bets and casino. The bonus is activated automatically after replenishing the account.
TerryTut
Today you can get to know a modern <a href="https://csmmsz.org">brooke monk deepfake porno</a>
VictorCrurf
Установка заборов и ограждений под ключ из металлопрофиля и евроштакетника <a href="http://ieef.msu.ru/index.php?subaction=userinfo&user=uxyku">http://ieef.msu.ru/index.php?subaction=userinfo&user=uxyku</a>
Shanecib
LuckyPari is a young site created by professionals <a href="https://luckypari-online-kazino.ru">https://luckypari-online-kazino.ru</a>
Haroldmix
Экскурсии по Красноярску <a href=https://tour-guide8.ru/>tour-guide8.ru</a> индивидуальные прогулки и групповые туры. Красивые виды, история города, заповедные места. Гиды с опытом, удобные форматы, гибкий график. Подарите себе незабываемые впечатления!
KeithGag
led экран уличный <a href=https://svetodiodnye-ekrany-videosteny.ru/>https://svetodiodnye-ekrany-videosteny.ru</a>
techalpaka
Нужен номер для ТГ? Предлагаем <a href=https://techalpaka.online/>https://techalpaka.online</a> для одноразовой или постоянной активации. Регистрация аккаунта без SIM-карты, в любом регионе. Удобно, надёжно, без привязки к оператору.
XavierBrino
After consuming a certain amount <a href="https://jinding.fr/wp-content/pgs/zametki_na_razlichnye_temy_2.html">https://jinding.fr/wp-content/pgs/zametki_na_razlichnye_temy_2.html</a>
Jasonenecy
Botulinum injections are ideal for removing horizontal wrinkles <a href="https://cosmedclinic.co.in/blog/pages/alybendazol_otzyvy.html">https://cosmedclinic.co.in/blog/pages/alybendazol_otzyvy.html</a>
HarryDic
Домприемка - помощь в приёмке квартир в новостройках <a href="https://dompriemka.ru">приемка дома перед покупкой</a>
CharlesFek
ноутбук asus цена <a href=https://kupit-noutbuk213.ru/>игровой ноутбук</a>
PatrickBig
магазин электроники товары <a href=https://magazin-elektroniki213.ru/>https://magazin-elektroniki213.ru</a>
Stevenpurgy
смартфон 10 цена <a href=https://smartfon-v-msk-cena.ru/>купить смартфон нова</a>
Robertwak
If you are interested in a 1xbet promo code for today <a href="https://withorwithout02.blogspot.com/2025/05/1xbet-promo-code-bonus-codes-valid-today.html">https://withorwithout02.blogspot.com/2025/05/1xbet-promo-code-bonus-codes-valid-today.html</a>
Dannysuida
https://kontraktnik.info
Mariondrype
The 1xBet bookmaker has established itself as one <a href="https://www.trimartolod.fr/pages/uhod_za_zubnymi_syemnymi_protezami.html">https://www.trimartolod.fr/pages/uhod_za_zubnymi_syemnymi_protezami.html</a>
RobertRok
электроника магазин интернет товары <a href=https://magazin-elektroniki213.ru/>маркетплейс техники и электроники</a>
TeodoroRer
Make the most of your cryptocurrency <a href="http://aspider.free.fr/index.php?file=Members&op=detail&autor=yjidocih">http://aspider.free.fr/index.php?file=Members&op=detail&autor=yjidocih</a>
PhilipCog
To help your website visitors easily navigate <a href="https://toppinvestors.com/profile.php?com=profile&username=geri-hardey-431315&name=Your_Account">https://toppinvestors.com/profile.php?com=profile&username=geri-hardey-431315&name=Your_Account</a>
MichaelHilia
купить ноутбук 2025 <a href=https://kupit-noutbuk213.ru/>ноутбук купить в москве</a>
urwork
Оказываем услуги <a href=https://urwork.ru/uslugi/zashhita-prav-potrebitelej-yuridicheskie-uslugi/>юрист по закону о защите прав потребителей</a>: консультации, подготовка претензий и исков, представительство в суде. Поможем вернуть деньги, заменить товар или взыскать компенсацию. Работаем быстро и по закону.
TysonRog
смартфон хонор цена <a href=https://smartfon-v-msk-cena.ru/>смартфон магазин цена</a>
Jamesrax
To receive the bonus, you need to register <a href="https://www.shakhty.su/board/post.php?mode=post&f=2104">как ввести промокод в мелбет</a>
pechat-nakleek
широкоформатная печать наклеек <a href=https://pechat-nakleek-spb11.ru/>печать круглых наклеек</a>
RobertpuH
Нужен номер для Телеграма? <a href=https://techalpaka.online/>купить одноразовый номер для телеграм</a> для безопасной регистрации и анонимного использования. Поддержка популярных регионов, удобный интерфейс, моментальный доступ.
Robertnat
Начните свое путешествие с 1xBet уже сегодня <a href="https://www.apelsin.su/wp-includes/articles/promokod_240.html">как получить промокод 1хбет</a>
Francistus
Свежие тенденции <a href=https://www.life-ua.com/>https://www.life-ua.com</a> советы по стилю и обзоры коллекций. Всё о моде, дизайне, одежде и аксессуарах для тех, кто хочет выглядеть современно и уверенно.
RaymondMer
Свежие тенденции <a href=https://www.life-ua.com/>https://www.life-ua.com</a> советы по стилю и обзоры коллекций. Всё о моде, дизайне, одежде и аксессуарах для тех, кто хочет выглядеть современно и уверенно.
ClairMip
Money Men is a 9 episode audio drama <a href="https://inextremis-antigaspi.fr/la-librairie/conseils_ecolos/la-mode-de-seconde-main-une-astuce-ecolonomique/">https://inextremis-antigaspi.fr/la-librairie/conseils_ecolos/la-mode-de-seconde-main-une-astuce-ecolonomique/</a>
pokerbonuses
Любимые карточные игры на <a href=https://pokerbonuses.ru/>покерок</a>. Новички и профессиональные игроки всё чаще выбирают площадку благодаря её стабильности и удобству. Здесь доступны кэш-игры, турниры с большими призовыми и эксклюзивные акции. Интерфейс адаптирован под мобильные устройства, а служба поддержки работает круглосуточно.
Abduljar
Инженерные системы <a href=https://usteplo.ru/>https://usteplo.ru</a> основа комфортного и безопасного пространства. Проектирование, монтаж и обслуживание отопления, водоснабжения, вентиляции, электроснабжения и слаботочных систем для домов и предприятий.
Thomasemore
консультации и онлайн услуги <a href=https://urwork.ru/uslugi/zashhita-prav-potrebitelej-yuridicheskie-uslugi/>юридические услуги по защите прав потребителей</a>: консультации, подготовка претензий и исков, представительство в суде. Поможем вернуть деньги, заменить товар или взыскать компенсацию. Работаем быстро и по закону.
Normanplami
Строительный портал <a href=https://stroydelo33.ru/>https://stroydelo33.ru</a> источник актуальной информации для тех, кто строит, ремонтирует или планирует. Полезные советы, обзоры инструментов, этапы работ, расчёты и готовые решения для дома и бизнеса.
JamesOmila
PDF documents are broadly used for sharing <a href="https://dailytrust.com/unlocking-the-power-of-pdf-word-counting-a-comprehensive-guide/">https://dailytrust.com/unlocking-the-power-of-pdf-word-counting-a-comprehensive-guide/</a>
JessieElomb
Любимые карточные игры на <a href=https://pokerbonuses.ru/>покерок</a>. Новички и профессиональные игроки всё чаще выбирают площадку благодаря её стабильности и удобству. Здесь доступны кэш-игры, турниры с большими призовыми и эксклюзивные акции. Интерфейс адаптирован под мобильные устройства, а служба поддержки работает круглосуточно.
Arthurcok
консультации и онлайн услуги <a href=https://urwork.ru/uslugi/zashhita-prav-potrebitelej-yuridicheskie-uslugi/>юрист по закону о защите прав потребителей</a>: консультации, подготовка претензий и исков, представительство в суде. Поможем вернуть деньги, заменить товар или взыскать компенсацию. Работаем быстро и по закону.
MichaelCok
ГГУ имени Ф.Скорины <a href=https://www.gsu.by/>https://www.gsu.by/</a> крупный учебный и научно-исследовательский центр Республики Беларусь. Высшее образование в сфере гуманитарных и естественных наук на 12 факультетах по 35 специальностям первой ступени образования и 22 специальностям второй, 69 специализациям.
Jimmydap
Francisk Skorina <a href=https://www.gsu.by/>https://www.gsu.by</a> Gomel State University. One of the leading academic and scientific-research centers of the Belarus. There are 12 Faculties at the University, 2 scientific and research institutes. Higher education in 35 specialities of the 1st degree of education and 22 specialities.
sajenci
свг гибрид саженцы <a href=https://sajenci.ru/>https://sajenci.ru</a>
vsibiry
ежевика высокого качества <a href=https://vsibiry.ru/>абрикосы морозостойкие</a>
Tommyboype
Алкогольные напитки купить с доставкой за 60 минут <a href="https://ru.pinterest.com/pin/701365342005068793/">доставка алкоголя</a>
AngelSpole
Create vivid images with <a href=https://promptchan.org/>Promptchan AI</a> — a powerful neural network for generating art based on text description. Support for SFW and NSFW modes, style customization, quick creation of visual content.
WallacePep
Недвижимость в Болгарии у моря <a href=https://byalahome.ru/>https://byalahome.ru</a> квартиры, дома, апартаменты в курортных городах. Продажа от застройщиков и собственников. Юридическое сопровождение, помощь в оформлении ВНЖ, консультации по инвестициям.
AngeloCat
The PARI bookmaker has a healthy number <a href="http://www.roller.ru/newforum/board/post.php?mode=post&f=7925">http://www.roller.ru/newforum/board/post.php?mode=post&f=7925</a>
EdwardSoona
Срочный выкуп квартир <a href=https://proday-kvarti.ru/>https://proday-kvarti.ru</a> за сутки — решим ваш жилищный или финансовый вопрос быстро. Гарантия законности сделки, юридическое сопровождение, помощь на всех этапах. Оценка — бесплатно, оформление — за наш счёт. Обращайтесь — мы всегда на связи и готовы выкупить квартиру.
DonaldPag
Портал о недвижимости <a href=https://akadem-ekb.ru/>https://akadem-ekb.ru</a> всё, что нужно знать о продаже, покупке и аренде жилья. Актуальные объявления, обзоры новостроек, советы экспертов, юридическая информация, ипотека, инвестиции. Помогаем выбрать квартиру или дом в любом городе.
JesseIsolf
мужской букет <a href=https://flowersspb.com/8marta>цветы на заказ с доставкой спб</a>
Jamesnup
букеты спб <a href=https://2gis.ru/spb/firm/70000001081058501>цветы рядом</a>
Kennethgak
букетная мастерская <a href=https://www.yp.ru/detail/id/roza_vetrov_tsvetochnaya_masterskaya_4629340>цветочное оформление свадьбы</a>
sajt-kopirajtera
Ищете копирайтера? <a href=https://sajt-kopirajtera.ru/jandeks-uslugi-prodvizhenie-profilja/>https://sajt-kopirajtera.ru/jandeks-uslugi-prodvizhenie-profilja/</a> Пишу тексты, которые продают, вовлекают и объясняют. Создам контент для сайта, блога, рекламы, каталога. Работаю с ТЗ, разбираюсь в SEO, адаптирую стиль под задачу. Чистота, смысл и результат — мои приоритеты. Закажите текст, который работает на вас.
topdommsk
Архитектурные решения <a href=https://топдом-мск.рф/>https://топдом-мск.рф</a> под ваши желания и участок. Создадим проект с нуля: планировка, фасад, инженерия, визуализация. Вы получите эксклюзивный дом, адаптированный под ваш образ жизни. Работаем точно, качественно и с любовью к деталям.
AdrianCet
Туристический портал <a href=https://prostokarta.com.ua/>https://prostokarta.com.ua</a> для путешественников: маршруты, достопримечательности, советы, бронирование туров и жилья, билеты, гайды по странам и городам. Планируйте отпуск легко — всё о путешествиях в одном месте.
Willydob
Фитнес-портал <a href=https://sportinvent.com.ua/>https://sportinvent.com.ua</a> ваш помощник в достижении спортивных целей. Тренировки дома и в зале, план питания, расчёт калорий, советы тренеров и диетологов. Подходит для начинающих и профессионалов. Всё о фитнесе — в одном месте и с реальной пользой для здоровья.
JamesSmaRk
Инновации, технологии, наука <a href=https://technocom.dp.ua/>https://technocom.dp.ua</a> на одном портале. Читайте о передовых решениях, новых продуктах, цифровой трансформации, робототехнике, стартапах и будущем IT. Всё самое важное и интересное из мира высоких технологий в одном месте — просто, понятно, актуально.
Merledes
Всё о мобильной технике <a href=https://webstore.com.ua/>https://webstore.com.ua</a> и технологиях: смартфоны, планшеты, гаджеты, новинки рынка, обзоры, сравнения, тесты, советы по выбору и настройке. Следите за тенденциями, обновлениями ОС и инновациями в мире мобильных устройств.
Phillipzem
YouTube Promotion <a href=https://laurasandra.medium.com/9-best-sites-to-buy-youtube-views-real-safe-d51001e5632e>buy youtube views</a> for your videos and increase reach. Real views from a live audience, quick launch, flexible packages. Ideal for new channels and content promotion. We help develop YouTube safely and effectively.
Denniserove
Натяжные потолки под ключ <a href=https://medium.com/@ksv.viet87/натяжные-потолки-мифы-о-вреде-и-экспертное-мнение-от-nova-28054185c2fd>https://vc.ru/id4737932/1977920-natyazhnye-potolki-mify-o-vrede</a> установка любых видов: матовые, глянцевые, сатиновые, многоуровневые, с фотопечатью и подсветкой. Широкий выбор фактур и цветов, замер бесплатно, монтаж за 1 день. Качественные материалы, гарантия и выгодные цены от производителя.
JoshuaBioke
Автомобильный портал <a href=https://autodream.com.ua/>https://autodream.com.ua</a> для автолюбителей и профессионалов: новости автоиндустрии, обзоры, тест-драйвы, сравнение моделей, советы по уходу и эксплуатации. Каталог авто, форум, рейтинги, автоновости. Всё об автомобилях — в одном месте, доступно и интересно.
Gabrielpaype
https://contract.moscow/
Hectorgor
Портал про авто <a href=https://livecage.com.ua/>https://livecage.com.ua</a> всё для автолюбителей: обзоры машин, тест-драйвы, новости автопрома, советы по ремонту и обслуживанию. Выбор авто, сравнение моделей, тюнинг, страховка, ПДД. Актуально, понятно и полезно. Будьте в курсе всего, что связано с автомобилями!
JasontrilS
Ты можешь всё <a href=https://love.zt.ua/>https://love.zt.ua</a> а мы подскажем, как. Женский портал о саморазвитии, личной эффективности, карьере, балансе между семьёй и амбициями. Здесь — опыт успешных женщин, практичные советы и реальные инструменты для роста.
JosephAcery
Современный женский портал <a href=https://beautyrecipes.kyiv.ua/>https://beautyrecipes.kyiv.ua</a> стиль жизни, мода, уход за собой, семья, дети, кулинария, карьера и вдохновение. Полезные советы, тесты, статьи и истории. Откровенно, интересно, по-настоящему. Всё, что важно и близко каждой женщине — в одном месте.
Michaelbem
На женском портале <a href=https://happytime.in.ua/>https://happytime.in.ua</a> статьи для души и тела: секреты красоты, женское здоровье, любовь и семья, рецепты, карьерные идеи, вдохновение. Место, где можно быть собой, делиться опытом и черпать силу в заботе о себе.
Jeffreypax
Добро пожаловать на женский портал <a href=https://lidia.kr.ua/>https://lidia.kr.ua</a> ваш гид по миру красоты, стиля и внутренней гармонии. Читайте про отношения, карьеру, воспитание детей, женское здоровье, эмоции и моду. Будьте вдохновлены лучшей версией себя каждый день вместе с нами.
NelsonCroky
Женский онлайн-журнал <a href=https://loveliness.kyiv.ua/>https://loveliness.kyiv.ua</a> о стиле, красоте, вдохновении и трендах. Интервью, мода, бьюти-обзоры, психология, любовь и карьера. Будь в курсе главного, читай мнения экспертов, следи за трендами и открывай новые грани себя каждый день.
Matthewvom
Онлайн-журнал для женщин <a href=https://mirwoman.kyiv.ua/>https://mirwoman.kyiv.ua</a> которые ищут не только советы, но и тепло. Личные истории, женское здоровье, психология, уютный дом, забота о себе, рецепты, отношения. Без давления, без шаблонов. Просто жизнь такой, какая она есть.
RonnieVex
Портал для женщин <a href=https://oa.rv.ua/>https://oa.rv.ua</a> всё, что важно: красота, здоровье, семья, карьера, мода, отношения, рецепты и саморазвитие. Полезные статьи, советы, тесты и вдохновение каждый день. Онлайн-пространство, где каждая найдёт ответы и поддержку.
Davidmuh
Современный женский портал <a href=https://womanonline.kyiv.ua/>https://womanonline.kyiv.ua</a> с актуальными темами: тренды, уход, макияж, фитнес, fashion, интервью, советы стилистов. Следи за модой, вдохновляйся образами, узнай, как подчеркнуть свою индивидуальность.
Pierrebuh
https://contract116.ru/
Haroldcrork
Сайт для женщин <a href=https://womenclub.kr.ua/>https://womenclub.kr.ua</a> всё, что волнует и вдохновляет: мода, красота, здоровье, отношения, дети, психология и карьера. Практичные советы, интересные статьи, вдохновение каждый день. Онлайн-пространство, созданное с заботой о вас и вашем настроении.
Franktiefe
Медицинский портал <a href=https://lpl.org.ua/>https://lpl.org.ua</a> с проверенной информацией от врачей: симптомы, заболевания, лечение, диагностика, препараты, ЗОЖ. Консультации специалистов, статьи, тесты и новости медицины. Только достоверные данные — без паники и домыслов. Здоровье начинается с знаний.
RaymondHieri
Надёжный медицинский портал <a href=https://una-unso.cv.ua/>https://una-unso.cv.ua</a> созданный для вашего здоровья и спокойствия. Статьи о заболеваниях, советы по лечению и образу жизни, подбор клиник и врачей. Понятный язык, актуальная информация, забота о вашем самочувствии — каждый день.
Randallmub
Чайная энциклопедия <a href=https://etea.com.ua/>https://etea.com.ua</a> всё о мире чая: сорта, происхождение, свойства, способы заваривания, чайные традиции разных стран. Узнайте, как выбрать качественный чай, в чём его польза и как раскрывается вкус в каждой чашке. Для ценителей и новичков.
GeorgeJes
Кулинарный портал <a href=https://mallinaproject.com.ua/>https://mallinaproject.com.ua</a> тысячи рецептов, пошаговые инструкции, фото, видео, удобный поиск по ингредиентам. Готовьте вкусно и разнообразно: от завтраков до десертов, от традиционной кухни до кулинарных трендов. Быстро, доступно, понятно!
RicardoTam
Современный мужской портал <a href=https://smart4business.net/>https://smart4business.net</a> о жизни, успехе и саморазвитии. Личный рост, инвестиции, бизнес, стиль, технологии, мотивация. Разбираем стратегии, делимся опытом, вдохновляем на движение вперёд. Для тех, кто выбирает силу, разум и результат.
BrianMab
Все новинки технологий <a href=https://axioma-techno.com.ua/>https://axioma-techno.com.ua</a> в одном месте: презентации, релизы, выставки, обзоры и утечки. Следим за рынком гаджетов, IT, авто, AR/VR, умного дома. Обновляем ежедневно. Не пропустите главные технологические события и открытия.
Lesterplage
Новинки технологий <a href=https://dumka.pl.ua/>https://dumka.pl.ua</a> портал о том, как научные открытия становятся частью повседневности. Искусственный интеллект, нанотехнологии, биоинженерия, 3D-печать, цифровизация. Простым языком о сложном — для тех, кто любит знать, как работает мир.
DavidPew
Автомобильный сайт <a href=https://kolesnitsa.com.ua/>https://kolesnitsa.com.ua</a> для души: редкие модели, автофан, необычные тесты, автоистории, подборки и юмор. Лёгкий и увлекательный контент, который приятно читать. Здесь не только про машины — здесь про стиль жизни на колёсах.
RalphSer
Актуальные новости <a href=https://polonina.com.ua/>https://polonina.com.ua</a> каждый день — политика, экономика, культура, спорт, технологии, происшествия. Надёжный источник информации без лишнего. Следите за событиями в России и мире, получайте факты, мнения и обзоры.
RobertoLEN
Следите за трендами автопрома <a href=https://viewport.com.ua/>https://viewport.com.ua</a> вместе с нами! На авто портале — новинки, презентации, обзоры, технологии, электромобили, автосалоны и экспертные мнения. Ежедневные обновления, честный взгляд на рынок, без лишнего шума и рекламы.
Phillipbuh
Полезные статьи и советы <a href=https://britishschool.kiev.ua/>https://britishschool.kiev.ua</a> на каждый день: здоровье, финансы, дом, отношения, саморазвитие, технологии и лайфхаки. Читайте, применяйте, делитесь — всё, что помогает жить проще, осознаннее и эффективнее. Достоверная информация и реальная польза.
Edwardclevy
Внедрите современные инструменты и сократите рутинные задачи, чтобы сосредоточиться на развитии бизнеса [url=https://forumsilverstars.forum24.ru/?1-5-0-00004784-000-0-0-1746551120]автоматизация магазина розничной торговли[/url]
Michaelunmap
Помогаем получить туристическую визу для поездки в страны Европы <a href="http://spain-about.ru/statti/2022/05/15/2012746385-viza-v-greciyu.html">http://spain-about.ru/statti/2022/05/15/2012746385-viza-v-greciyu.html</a>
Davidvof
A multiple-entry visa allows you to travel to Schengen countries as many times [url=https://deutschlanddeutsch.ru/chto-proishodit-v-vizovom-centre/]https://deutschlanddeutsch.ru/chto-proishodit-v-vizovom-centre/[/url]
Ramirotrent
Сайт для женщин <a href=https://funtura.com.ua/>https://funtura.com.ua</a> всё, что интересно каждый день: бьюти-советы, рецепты, отношения, дети, стиль, покупки, лайфхаки и настроение. Яркие статьи, тесты и вдохновение. Просто, легко, по-женски.
Michaeletele
Это не просто сайт для женщин <a href=https://godwood.com.ua/>https://godwood.com.ua</a> это пространство, где вас слышат. Здесь — забота, поддержка, советы по жизни, отношениям, здоровью, семье и внутреннему балансу. Никакой критики, только доброта и уверенность: всё будет хорошо, и вы не одна.
DonaldNiz
Информационно-познавательный <a href=https://golosiyiv.kiev.ua/>https://golosiyiv.kiev.ua</a> портал для мужчин и женщин: полезные статьи, советы, обзоры, лайфхаки, здоровье, психология, стиль, семья и финансы. Всё, что важно знать для жизни, развития и комфорта. Читайте, развивайтесь, вдохновляйтесь вместе с нами.
DustinlaW
трековые натяжные потолки <a href=https://natyazhnye-potolki-moskva1.ru/>сколько стоит натяжной потолок</a>
GregoryFug
Сильная, умная, стильная <a href=https://lugor.org.ua/>https://lugor.org.ua</a> вот для кого наш женский онлайн-журнал. Темы: мода, карьера, дети, отношения, дом, здоровье. Разговор о реальной жизни: без глянца, но со вкусом.
Raymondpef
Женский онлайн-журнал <a href=https://gorod-lubvi.com.ua/>https://gorod-lubvi.com.ua</a> о красоте, стиле и уходе. Советы визажистов, подбор образов, секреты молодости, модные тренды. Всё, чтобы чувствовать себя уверенно и выглядеть на миллион. Будь в курсе, вдохновляйся и подбирай стиль по душе.
WilliamSlilt
Женский онлайн-журнал <a href=https://inclub.lg.ua/>https://inclub.lg.ua</a> о силе выбора. Карьера, финансы, тайм-менеджмент, уверенность, стиль и баланс. Для женщин, которые двигаются вперёд, строят, влияют, мечтают. Говорим по делу — без стереотипов и с уважением к вашему пути.
Roberttuh
I have a multiple entry visa and my friend [url=https://vista.news/society/52346]https://vista.news/society/52346[/url]
RobertArott
Apply for a visa online or at one of our offices <a href="https://discoveric.ru/statyi/all/passport/osobennosti-oformleniya-vizovyh-dokumentov-vo-franciyu-dlya-rossiyan-73700">https://discoveric.ru/statyi/all/passport/osobennosti-oformleniya-vizovyh-dokumentov-vo-franciyu-dlya-rossiyan-73700</a>
JosephMek
Портал для женщин <a href=https://prettiness.kyiv.ua/>https://prettiness.kyiv.ua</a> которые любят жизнь во всех её красках. Советы, мода, рецепты, отношения, вдохновение, дом и путешествия. Каждый день — новая идея, интересная мысль и повод улыбнуться.
Rubenvex
Портал для активных <a href=https://onlystyle.com.ua/>https://onlystyle.com.ua</a> стильных, современных женщин. Мода, карьера, здоровье, бьюти-тренды, фитнес, лайфхаки, вдохновение. Будь в курсе, живи ярко, выбирай смело. Никаких скучных статей — только драйв, стиль и реальная польза.
Wilburnrit
Модный журнал <a href=https://psilocybe-larvae.com/>https://psilocybe-larvae.com</a> всё о стиле, трендах, бьюти-новинках, звёздах и вдохновении. Образы с подиумов, советы стилистов, актуальные коллекции, мода улиц и мировые бренды.
Martinanync
Профессиональный <a href=https://taplink.cc/ivanteevkamassage>массаж Ивантеевка</a>: для спины, шеи, поясницы, при остеохондрозе и сколиозе. Медицинский и спортивный подход, опытные специалисты, точечное воздействие. Снятие болей, восстановление подвижности, улучшение самочувствия.
Lestertic
Онлайн-портал для женщин <a href=https://rpl.net.ua/>https://rpl.net.ua</a> всё о жизни, стиле, здоровье, отношениях, карьере, детях, красоте и вдохновении. Полезные статьи, советы, идеи и актуальные темы.
DonaldJax
Женский онлайн-портал <a href=https://sweaterok.com.ua/>https://sweaterok.com.ua</a> это не просто сайт, а поддержка в повседневной жизни. Честные темы, важные вопросы, советы и тепло. От эмоций до материнства, от тела до мыслей.
PedroLaphy
The tourism business is one of the most attractive business areas <a href="http://portal.krasno.ru/viewtopic.php?f=2&t=57792&view=print">http://portal.krasno.ru/viewtopic.php?f=2&t=57792&view=print</a>
RobertTog
One of them is if the applicant has relatives or friends [url=http://astravel.ru/portal/publikacii/284-oformlenie-vizy-za-granicu.html]http://astravel.ru/portal/publikacii/284-oformlenie-vizy-za-granicu.html[/url]
Louissix
Онлайн-журнал для женщин <a href=https://tiamo.rv.ua/>https://tiamo.rv.ua</a> которые ищут баланс. Психология, эмоции, отношения, самоценность, женское здоровье. Честные тексты, поддержка, путь к себе. Пространство, где можно дышать глубже, читать с удовольствием и чувствовать, что тебя понимают.
Williamvak
Женский онлайн-журнал <a href=https://trendy.in.ua/>https://trendy.in.ua</a> о выборе, деньгах, успехе и личных целях. Как совмещать карьеру и семью, строить бизнес, говорить "нет" и заботиться о себе. Истории, советы, интервью, вдохновение. Для тех, кто идёт вперёд — в своих темпах и с опорой на себя.
DarylWep
Онлайн фитнес-журнал <a href=https://bahgorsovet.org.ua/>https://bahgorsovet.org.ua</a> полезные статьи от тренеров и нутрициологов: программы тренировок, восстановление, питание, биомеханика, анализ ошибок. Говорим на языке результата. Научный подход без воды — для тех, кто ценит эффективность.
DannyImind
Всё о лечении диабета <a href=https://diabet911.com/>https://diabet911.com</a> типы заболевания, симптомы, диагностика, питание, образ жизни и лекарственная терапия. Объясняем просто и понятно. Актуальная информация, советы врачей, статьи для пациентов и близких.
Joshualeals
Сайт о здоровье глаз <a href=https://eyecenter.com.ua/>https://eyecenter.com.ua</a> полезные статьи, советы офтальмологов, симптомы заболеваний, диагностика, лечение, упражнения для зрения. Всё о профилактике, коррекции, очках, линзах и современных методах восстановления.
Perrybed
Сайт для женщин <a href=https://expertlaw.com.ua/>https://expertlaw.com.ua</a> которые любят моду, красоту и стильную жизнь. Актуальные тренды, советы по уходу, подбор образов, вдохновляющие идеи для гардероба и макияжа.
Thomasbeict
дипломная работа срочно на заказ <a href=https://diplomastudy.ru/>дипломные работы на заказ</a>
Thomasundut
купить реферат цена <a href=https://referatymarketing.ru/>заказать реферат недорого</a>
Andrewcen
Сайт о мужском здоровье <a href=https://kakbog.com/>https://kakbog.com</a> достоверная информация о гормональном фоне, потенции, урологических проблемах, профилактике, питании и образе жизни. Советы врачей, диагностика, лечение, препараты.
DamonJeons
Современный медицинский портал <a href=https://medfactor.com.ua/>https://medfactor.com.ua</a> с упором на технологии: телемедицина, онлайн-запись, цифровые карты, расшифровка анализов, подбор препаратов. Удобный доступ к информации и поддержка на всех этапах — от симптомов до выздоровления.
Vernonlax
Надёжный медицинский портал <a href=https://pobedilivmeste.org.ua/>https://pobedilivmeste.org.ua</a> с удобной навигацией и актуальной информацией. Болезни, симптомы, приёмы врачей, анализы, исследования, препараты и рекомендации.
Josephviefs
Мужской портал <a href=https://realman.com.ua/>https://realman.com.ua</a> всё, что интересно и полезно: спорт, здоровье, стиль, авто, отношения, технологии, карьера и отдых. Практичные советы, обзоры, мнения и поддержка.
Alfredvew
Кулинарные рецепты <a href=https://kulinaria.com.ua/>https://kulinaria.com.ua</a> на каждый день и для особых случаев. Домашняя выпечка, супы, салаты, десерты, блюда из мяса и овощей. Простые пошаговые инструкции, доступные ингредиенты и душевные вкусы.
Nelsonded
Сайт для мужчин <a href=https://phizmat.org.ua/>https://phizmat.org.ua</a> всё о жизни с характером: здоровье, спорт, стиль, авто, карьера, отношения, технологии. Полезные советы, обзоры, мужской взгляд на важные темы.
TyroneSnuby
Новостной портал <a href=https://sensus.org.ua/>https://sensus.org.ua</a> главные события дня в России и мире. Политика, экономика, общество, культура, спорт и технологии. Только проверенные факты, оперативные сводки, мнения экспертов и честная подача.
Allenbot
медицинский портал <a href=https://pobedilivmeste.org.ua/>https://pobedilivmeste.org.ua</a> с удобной навигацией и актуальной информацией. Болезни, симптомы, приёмы врачей, анализы, исследования, препараты и рекомендации.
RobertLaf
взять микрозаем онлайн <a href=https://vzyat-mikrozajm-5.ru/>деньги онлайн</a>
RichardFen
Klavier noten <a href=https://klavier-noten-3.ru/>noten von klavier</a>
Miguelcedia
Ready to ignite your betting or gaming adventure [url=http://programmersforum.ru/forum/post.php?mode=post&f=1636]http://programmersforum.ru/forum/post.php?mode=post&f=1636[/url]
ArthurAceri
оформить онлайн займ <a href=https://vzyat-mikrozajm-5.ru/>мфо взять займ</a>
DanielSputt
Пианино по нотам <a href=https://noty-fortepiano.ru/>ноты для пианино песни</a>
JoshuaUNsum
Лучшие специалисты <a href=https://gid-po-kaliningradu.ru/>индивидуальные гиды Калининград</a> ждут вас.
BrianKnork
На нашем сайте вы найдёте <a href=https://sebe-na-zametku.ru/>поздравительные картинки</a> для любого случая. Яркие изображения, тёплые слова, праздничное настроение и стильный дизайн. Поделитесь эмоциями с близкими и сделайте каждый день особенным. Обновления каждый день, удобный формат, всё бесплатно!
Michaelnal
Недавно у меня была возможность познакомиться с компанией Matsushita Kogyo Co https://matsushita-kk.com
Marcustah
сколько стоит реферат <a href=http://referatymarketing.ru/>готовые рефераты</a>
TitusCrilA
дипломная работа цена <a href=http://diplomastudy.ru/>дипломная работа срочно на заказ</a>
Edgaramups
I recently started using stats-japan.jp for a research project, and I have to say it's a goldmine for anyone interested in Japan’s demographic, economic, and industrial data https://stats-japan.jp/
Brentscexy
натяжные потолки недорого <a href=https://natyazhnye-potolki-moskva1.ru/>заказать установку натяжных потолков</a>
Williamrap
Мы предлагаем <a href=https://komfortvl.ru/>услуги по ремонту квартир</a> с гарантией качества, соблюдением сроков и полным сопровождением. Индивидуальный подход, современные материалы и прозрачные цены. Работаем по договору. Закажите бесплатную консультацию и начните комфортный ремонт уже сегодня!
arenda-avto
сайт прокат авто <a href=https://www.innov.ru/news/auto/prokat-avtomobiley-v-sankt-peterburge-lyubye-klassy-ot-ekonom-do-premium/>аренда авто без залога</a>
Rickynar
аренда авто недорого <a href=https://ambox.ru/puteshestvujte-po-kaliningradu-na-svoyom-avto/>прокат авто круглосуточно</a>
RogerSycle
У нас вы можете купить саженцы гортензий, роз, плодовых деревьев и ягодных культур, очень много многлетних цветов с доставкой по Новосибирску и всей России — только проверенные сорта, идеально подходящие для вашего климата [url=https://nsksad.ru]https://nsksad.ru[/url]
falloutbuy
Играешь в Fallout 76? Хочешь <a href=https://falloutbuy.com/>прокачка Fallout 76</a>? Широкий ассортимент предметов, включая силовую броню, легендарное оружие, хлам, схемы и многое другое для Fallout 76 на PC, Xbox и PlayStation. Мы предлагаем услуги буста, прокачки персонажа и готовые комплекты снаряжения.
diabloshop
На diabloshop.ru вы можете купить <a href=https://diabloshop.ru/product-category/diablo-3-reaper-of-souls/ >https://diabloshop.ru/product-category/diablo-3-reaper-of-souls/</a> золото Diablo 4, руны Diablo 2 Resurrected, а также уникальные предметы и легендарное снаряжение для всех платформ — PC, Xbox, PlayStation и Nintendo Switch. Мы предлагаем быстрый буст персонажа, услуги прокачки, сбор лучших билдов и готовые комплекты снаряжения.
ManuelSault
The main purpose of this incentive is to motivate new players to place <a href="http://share.psiterror.ru/2025/05/18/promokod-melbet-1.html">http://share.psiterror.ru/2025/05/18/promokod-melbet-1.html</a>
ThomasBurgy
На diabloshop.ru вы можете купить <a href=https://diabloshop.ru/product-category/diablo-4/>https://diabloshop.ru/product-category/diablo-4/</a> золото Diablo 4, руны Diablo 2 Resurrected, а также уникальные предметы и легендарное снаряжение для всех платформ — PC, Xbox, PlayStation и Nintendo Switch. Мы предлагаем быстрый буст персонажа, услуги прокачки, сбор лучших билдов и готовые комплекты снаряжения.
Richardzot
Unlock an exclusive welcome offer by using the 1xBet [url=https://bookmark-group.com/story5186556/1xbet-free-bet-promo-code-sri-lanka]https://bookmark-group.com/story5186556/1xbet-free-bet-promo-code-sri-lanka[/url]
KennethGok
Играешь в Fallout 76? Хочешь <a href=https://falloutbuy.com/>прокачка Fallout 76</a>? Широкий ассортимент предметов, включая силовую броню, легендарное оружие, хлам, схемы и многое другое для Fallout 76 на PC, Xbox и PlayStation. Мы предлагаем услуги буста, прокачки персонажа и готовые комплекты снаряжения.
ekskursii-kaliningrad
интересные экскурсии в калининграде <a href=https://ehkskursii-v-kaliningrade.ru/>экскурсии в калининграде 2025 цены</a>
Alfredbip
Контроль расходов, исключение "человеческого фактора" и рост среднего чека — проверенные решения для вашего бизнеса <a href="https://forumsilverstars.forum24.ru/?1-5-0-00004784-000-0-0-1746551120">программа учета для кафе</a>
RafaelNog
Участвуйте в государственных и коммерческих тендерах онлайн — находите новых поставщиков и покупателей без лишних затрат [url=https://saby.ru/news/tenders/289144e3-168b-4a99-b8c6-1e1ba3ab5c06]торги кз[/url]
NathanDyefe
юрист по семейному праву консультация <a href=https://urwork.ru/uslugi/semejnyj-yurist/>юрист по семейным делам санкт петербург</a>
Williammus
ст о взыскании задолженности <a href=https://urwork.ru/uslugi/vzyskanie-zadolzhennostej-yuridicheskie-uslugi/>https://urwork.ru/uslugi/vzyskanie-zadolzhennostej-yuridicheskie-uslugi/</a>
JamesGot
New players receive a 100% first deposit bonus <a href="https://nybookmark.com/story21342474/1xbet-promo-code-registration-bangladesh">https://nybookmark.com/story21342474/1xbet-promo-code-registration-bangladesh</a>
DanielLaula
The main reason is often a lack of information about what bonuses [url=https://phat4life.mn.co/posts/about-me-84838535/comments/131210285?utm_source=manual]https://phat4life.mn.co/posts/about-me-84838535/comments/131210285?utm_source=manual[/url]
DailyDeals
http://elecdz.cn/elec/xcj/home.php?mod=space&uid=7447&do=profile
DeweySow
We recently partnered with pro-s.jp to help us streamline our internal operations, and I have to say — it made a real difference https://pro-s.jp/
ChrisEsona
New players receive a 100% first deposit bonus up to €130 for sports betting <a href="https://scrapbox.io/allblogs/CГіdigo_Promocional_1xBet_para_Bono_Gratis_hasta_€130">https://scrapbox.io/allblogs/CГіdigo_Promocional_1xBet_para_Bono_Gratis_hasta_€130</a>
pornjourney
Discover <a href=https://pornjourney.app/>create porn</a>, a platform where artificial intelligence makes your desires come true. Create your perfect AI heroines, chat in real time, and enjoy personalized content tailored to your tastes. The next level of sex technology is here.
Wilfredoxype
Металлические ограждения <a href=https://osk-stroi.ru/>https://osk-stroi.ru</a> для дома, дачи, промышленных и общественных объектов. Качественные материалы, долговечность, устойчивость к коррозии. Быстрая установка и индивидуальное изготовление под заказ.
Nathanfrelo
Пиломатериалы от производителя <a href=https://tsentr-stroy.ru/>https://tsentr-stroy.ru</a> по доступным ценам. В наличии обрезная и необрезная доска, брус, вагонка, доска пола, рейка и другие изделия. Работаем с частными и корпоративными заказами. Качество, доставка, гибкие условия.
Mosesmaync
Инвестиции в строительство <a href=https://permgragdanstroy.ru/>https://permgragdanstroy.ru</a> жилой и коммерческой недвижимости. Прибыльные проекты, прозрачные условия, сопровождение на всех этапах. Участвуйте в строительстве с гарантированной доходностью.
RobertJaima
Агентство недвижимости <a href=https://assa-dom.ru/>https://assa-dom.ru</a> покупка, продажа, аренда квартир, домов, участков и коммерческих объектов. Полное сопровождение сделок, помощь с ипотекой, юридическая поддержка. Надежно, удобно, профессионально.
WilliamDut
Betting specials with enhanced odds, and cashout functionality for full [url=https://www.bloodtobaby.com/profile/promokodp21i15677/profile]https://www.bloodtobaby.com/profile/promokodp21i15677/profile[/url]
CharlesFub
Недвижимость Черноземья <a href=https://nedvizhimostchernozemya.ru/>https://nedvizhimostchernozemya.ru</a> квартиры, дома, участки, коммерческие объекты. Продажа и аренда во всех крупных городах региона. Надежные застройщики, проверенные предложения, прозрачные сделки.
Jamesmoica
These numbers are suitable for both personal and business use [url=http://www.st70.cn/20241017/49473296.html]http://www.st70.cn/20241017/49473296.html[/url]
CharlesTeamp
Discover everything you need to know about renting a car in Dubai. Learn about the requirements, traffic rules, parking options, and how to avoid fines <a href="https://insiderpaper.com/the-rise-of-electric-vehicle-rentals-how-yeti-is-leading-the-green-charge-in-dubai/">https://insiderpaper.com/the-rise-of-electric-vehicle-rentals-how-yeti-is-leading-the-green-charge-in-dubai/</a>
RichardVom
In cases like this, the advantage signal supplies a 30% boost [url=https://anotepad.com/notes/k8hawkjx3]https://anotepad.com/notes/k8hawkjx3[/url]
Andrewcucky
The two most popular types of business phone numbers are geographical [url=http://www.hntoo.cn/20241017/43443493.html]http://www.hntoo.cn/20241017/43443493.html[/url]
Thomasunpar
интернет магазин на laravel <a href=https://razrabotka-sayta-laravel.ru/>разработка интернет сайтов минск</a>
Edwardbreaf
изготовление шильдика металлического <a href=https://metallicheskie-shildy.ru/>изготовление шильд</a>
MichaelOffew
The first promo code from 1xBet is given for free <a href="https://www.imdb.com/list/ls592947575/">https://www.imdb.com/list/ls592947575/</a>
Donaldsax
металлический бейдж <a href=https://premium-badge-msk.ru/>бейджики из латуни</a>
JasonAdugh
Free Cam helps you quickly create videos, edit them and post them [url=https://bbw-cams.net/]meet bbw[/url]
HowardGem
Откройте для себя лучшие мероприятия и развлечения в Санкт-Петербурге [url=https://kudaspb.com/afisha]Афиша СПб[/url]
Russellcow
Регистрация бизнеса в Грузии - откроем ИП Грузии под ключ. Поможем получить ВНЖ Грузии по ИП <a href="https://ip-georgia.com/">ВНЖ Грузии</a>
Justinavere
Микрозаймы без отказа без проверки <a href=https://zajm-bez-otkaza.ru/>быстрый займ без отказа</a>
EugeneTem
Быстрые деньги онлайн на карту <a href=https://zajm-onlajn-1.ru/>взять деньги в займ на карту</a>
VicenteLib
Займ взять <a href=https://bystryj-zajm.ru/>взять в займ</a>
Kevinpat
В интернет-магазине Miele в Москве можно купить качественную бытовую кухонную технику [url=https://prodam-pylesos.ru/]miele купить[/url]
ThomasEcogy
This is a tested and verified chode. It works in all countries [url=https://bookmaker-ratings.ru/wiki/promokod-1xbet-kak-poluchit/]порно онлайн студентки[/url]
Michaelbub
Поможем вам подобрать авто из большого выбора марок и моделей - американских, европейских и китайских <a href="https://avtoservis-gid.ru/komp/pikap-tsentr-moskva">https://avtoservis-gid.ru/komp/pikap-tsentr-moskva</a>
Anthonychivy
латунные шильдики <a href=https://izgotovlenie-shildov-na-zakaz.ru/>шильды металлические изготовление</a>
Melvingom
шильда методом травления <a href=https://shildi-iz-metalla.ru/>металлические шильды пришивные</a>
RussellBoync
продвижение раскрутка <a href=https://seoprocessoptimization.ru/>заказать продвижение</a>
Richardmopes
1Win Promo Code - enter it upon registration to receive a bonus [url=https://fr.johnnybet.com/code-de-parrainage-1xbet-1]порно девушек онлайн[/url]
Zacharypoece
Сотрудничество с аутсорсинговой компанией позволяет снизить операционные расходы [url=http://bpf.ru/finansovaya-gramotnost/rekomendatsii-dlya-rabotodatelej-chto-dolzhen-umet-bukhgalter.html]http://bpf.ru/finansovaya-gramotnost/rekomendatsii-dlya-rabotodatelej-chto-dolzhen-umet-bukhgalter.html[/url]
Victortup
Чтобы определить какой автомобиль лучше выбрать, необходимо определить Ваши потребности и предпочтения <a href="https://www.easycounter.com/report/pickup-center.ru">https://www.easycounter.com/report/pickup-center.ru</a>
DonnieGof
Бесплатная панель управления <a href=https://1panel.click/>panel 1Panel</a> сервером с открытым исходным кодом. Удобный интерфейс, поддержка популярных ОС, автоматизация задач, резервное копирование, управление сайтами и базами. Оптимально для вебмастеров и системных администраторов.
WilliamDob
услуги юриста <a href=https://advokat-abramov.ru/>семейный юрист</a>
Jamesincop
cloud browser <a href=https://bitco.biz/2025/05/23/headless-web-automation-leveraging-chrome-and-cloud-platforms/>headless chrome browser</a>
devrum
управление строительными проектами <a href=https://devrum.ru/modul-upravleniya-personalom/>модуль управления персоналом</a>
WalterRor
В статье рассказываем, как аутсорсинг и аутстаффинг упрощают бизнес-процессы [url=https://www.oreanda-news.com/other/Minfin_schitaet_chto_v_blijayshee_vremya_vozmojno_pridetsya_povysit_nalogi/article957764/]https://www.oreanda-news.com/other/Minfin_schitaet_chto_v_blijayshee_vremya_vozmojno_pridetsya_povysit_nalogi/article957764/[/url]
DwightAbize
бейдж на заказ <a href=https://badge-moscow-na-zakaz.ru/>бейджики латунные с гравировкой срочно москва</a>
DavidEvelt
корпоративные значки на заказ <a href=https://znachki-metallicheskie-zakaz.ru/>металлические значки под заказ</a>
JeffreymeT
Сравнение возраста автомобиля и его пробега помогает уменьшить фактор «повезло/не повезло» <a href="https://autonovosib.ru/companies/69159/">https://autonovosib.ru/companies/69159/</a>
znachki-zakaz
металлические пины на заказ <a href=https://znachki-zakaz-moskva.ru/>производство значков из металла</a>
PhilipCem
Bы можете зaкaзать медицинскую справку в Москве в нашей клинике [url=https://xn--90af3aacbbgg8a.xn--p1ai/2025/05/%d1%81%d0%bf%d1%80%d0%b0%d0%b2%d0%ba%d0%b0-%d0%be%d1%82-%d0%b3%d0%b8%d0%bd%d0%b5%d0%ba%d0%be%d0%bb%d0%be%d0%b3%d0%b0/]https://xn--90af3aacbbgg8a.xn--p1ai/2025/05/%d1%81%d0%bf%d1%80%d0%b0%d0%b2%d0%ba%d0%b0-%d0%be%d1%82-%d0%b3%d0%b8%d0%bd%d0%b5%d0%ba%d0%be%d0%bb%d0%be%d0%b3%d0%b0/[/url]
DonniealbuH
сколько стоит раскрутка сайта в яндекс <a href=http://seoprocessoptimization.ru/>раскрутка сайта сколько стоит</a>
StevePlate
значки из металла на заказ москва <a href=https://izgotovit-znachki-metalicheskie.ru/>изготовление значков из металла на заказ</a>
Alonzoruh
seo продвижение сайта компании москва <a href=https://seoprocessoptimization.ru/>агентство контекстной рекламы</a>
Williaminomb
сайт типографии спб <a href=https://tipografiya-spb7.ru/>https://tipografiya-spb7.ru</a>
Jerryjounc
типография изготовление <a href=https://tipografiya-spb11.ru/>типография напечатать</a>
JamesGal
типография спб дешево <a href=https://tipografiya-spb55.ru/>типография цена</a>
Henryvon
Ищете, где <a href=https://motoreuro.ru/>https://motoreuro.ru</a> с гарантией и доставкой? Мы предлагаем проверенные агрегаты с пробегом до 100 тыс. км из Японии, Европы и Кореи. Подбор, установка, оформление документов — всё под ключ.
KennethNup
печать визиток недорого <a href=https://pechat-vizitok33.ru/>https://pechat-vizitok33.ru</a>
BlakeMex
печать визиток быстро <a href=https://pechat-vizitok11.ru/>печать визиток на заказ</a>
stanki-a
Станки для производства <a href=https://stanki-a.ru/>вальцовочный станок купить</a> металлообработка, резка, сварка, автоматизация. Продажа новых и восстановленных моделей от ведущих брендов. Гарантия, обучение персонала, техподдержка.
JeffreyBrems
Онлайн сервис <a href=https://picex.ru/>сервис для скачивания изображений с сайта</a> для получения картинок с любого сайта. Вставьте URL — и мгновенно получите изображения на своём устройстве. Поддержка всех форматов, никаких ограничений и лишних действий. Работает бесплатно и круглосуточно.
nakleyki-pechat
Нужна <a href=https://pechat-nakleek1.ru/>печать наклеек купить</a>? Закажите стикеры любых форм и размеров с доставкой. Яркие, прочные, влагостойкие наклейки на пленке и бумаге — для рекламы, декора, маркировки и упаковки.
tipografiya-spb
Профессиональная <a href=https://tipografiya-spb33.ru/>типография производство</a>. Изготовим любые печатные материалы — от визиток до каталогов. Качественно, быстро, с гарантией. Закажите онлайн или приезжайте в офис в СПб.
pechat-nakleek
Изготовление и <a href=https://pechat-nakleek44.ru/>https://pechat-nakleek44.ru</a>. Стикеры для бизнеса, сувениров, интерьера и упаковки. Печатаем тиражами от 1 штуки, любые материалы и формы. Качественно, недорого, с доставкой по СПб.
Charleslam
mexican rx online: <a href=" https://rxexpressmexico.com/# ">RxExpressMexico</a> - mexico drug stores pharmacies
JosephSOg
Безболезненная <a href=https://lazernaya-epilyaciya33.ru/>лазерная эпиляция волос</a> Удаление волос на любом участке тела. Работаем с чувствительной кожей, используем новейшие лазеры. Акции, абонементы, индивидуальный подход.
RobertEnhap
Удаление волос <a href=https://lazernaya-epilyaciya-spb1.ru/>https://lazernaya-epilyaciya-spb1.ru</a>: гладкая кожа на долгое время. Аппараты последнего поколения, опытные мастера, комфортная обстановка. Эпиляция для женщин и мужчин. Онлайн-запись, гибкие цены, без лишнего стресса.
PatrickCeava
Профессиональная <a href=https://lazernaya-epilyaciya11.ru/>процедура лазерной эпиляции</a>. Эффективное удаление волос на любом участке тела, подход к любому фототипу. Сертифицированные специалисты, стерильность, скидки. Запишитесь прямо сейчас!
Jamesapart
грузчик нанять <a href=https://gruzoperevozki-svao.ru/>https://gruzoperevozki-svao.ru</a>
Michaeldoons
грузчики услуги <a href=https://gruzchikiise.ru/>грузчик срочно</a>
Brianprogy
грузчики недорого <a href=https://ungruzchiki.ru/>правильные грузчики</a>
Michealrip
услуги грузчиков городу <a href=https://gruzoperevozki-svao.ru/>услуги грузчиков заказать</a>
Charlieliack
медицинский центр отзывы <a href=https://medicinskiy-centr11.ru/>телефон медицинского центра</a>
MichaelRog
Избавьтесь от волос <a href=https://lazernaya-epilyaciya-spb5.ru/>сеансы лазерной эпиляции</a> навсегда — с помощью лазерной эпиляции. Эффективные процедуры на любом участке тела, минимальный дискомфорт, заметный результат уже после первого сеанса.
magazin-soft
программное обеспечение купить цена <a href=https://internet-magazin-soft.kz/>программное обеспечение компьютера купить</a>
JorgeBeill
Looking for love? Join our online dating site and find your perfect match today [url=https://t.me/s/bbwcamsnet]bbw porn[/url]
Robertblome
Soil compaction is one of the most important operations carried [url=https://betonly.ru/stati/innovacii-na-styke-nauki-i-stroitelstva-poliplast-i-vniig-im.-vedeneeva-obedinyayut-usiliya.html]Инновации на стыке науки и строительства: «Полипласт» и ВНИИГ им. Веденеева объединяют усилия[/url]
Harleymoire
заказать цветы с доставкой <a href=https://dostavka-cvetov1.ru/>заказать цвет с доставкой</a>
DavidRam
кабинет узи абакан <a href=https://uzi-abakan11.ru/>узи цена</a>
Jorgebut
дерматологи абакана отзывы <a href=https://dermatolog-abakan1.ru/>дерматолог абакан взрослый</a>
Felixsmize
сайт клиники <a href=https://medicinskiy-centr-abakan11.ru/>клиника абакан официальный</a>
Winstonrexia
Culinary diplomacy is the practice of using food and culinary [url=https://amanimiami.com/services/chauffeur-services]Chauffeur Services[/url]
Javierlon
нейросеть чат GPT <a href=https://ruschatgpt.ru/>чат жпти</a>
CharlesAttaf
Единый портал аренды. На Аренда24 можно взять в аренду или сдать в аренду коммерческую недвижимость, строительную технику, оборудование от ИП и организаций по всей Беларуси [url=https://arenda24.by/category/avtokrany-20t]Аренда крана 20 тонн[/url]
Jamesdax
кабинет терапевта <a href=https://terapevt-abakan1.ru/>терапевт абакан</a>
Jerryhaips
Квартирный и офисный <a href=https://declarant-iv.livejournal.com/20546.html>https://declarant-iv.livejournal.com/20546.html</a> переезд под ключ с грузчиками. Бережная упаковка, погрузка, транспортировка и сборка мебели. Быстро, аккуратно, по доступной цене. Работают опытные специалисты.
Victortub
Уже много лет мы доставляем алкоголь прямо к вашему дому в Москве в любое время дня и ночи [url=https://alcomagaz.ru/]алкоголь купить круглосуточно с доставкой[/url]
WilliamMeels
грузчики услуги <a href=https://vog-pereezd.ru/>грузчика заказать</a>